Video
Repositioning for pressure injury/ulcer prevention: TEAM-UP trial resultsUlcer prevention in the workplace -
Skip to main content Skip to navigation. Text Size:. Show accessibility tools. Pressure ulcer prevention. Home Patients and families Patient safety Pressure ulcer prevention.
Pressure ulcers: Advice for patients and carers We are committed to preventing pressure ulcers and helping local patients, families or carers to manage pressure ulcers more effectively.
What is a pressure ulcer? Pressure ulcer information:. Play video. Pressure ulcer information: The facts about pressure ulcers: Pressure ulcers can occur within a matter of hours for those at risk Regular top to toe skin inspections are needed to help prevent pressure ulcers occurring.
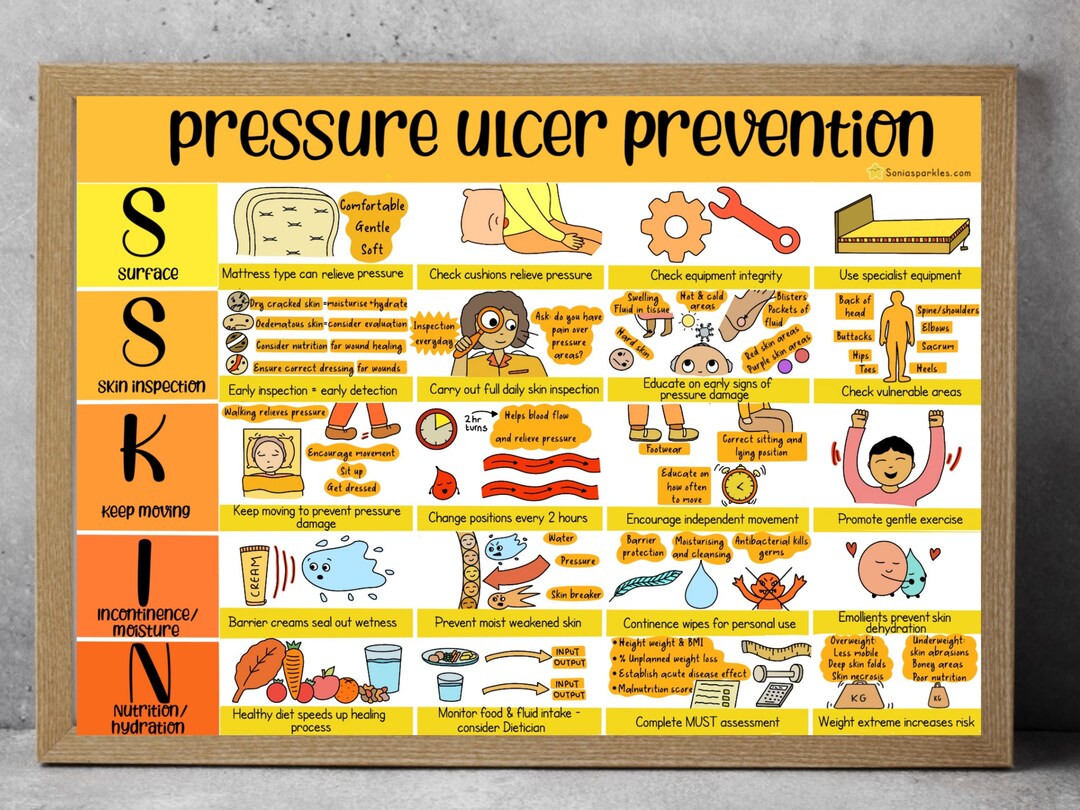
Look out for reddening that does not subside over bony areas. Good SSKIN can help prevent pressure ulcers click here. Michael McGrath's story How to prevent pressure ulcers film Play video. Return to Contents. The sections above have outlined best practices in pressure ulcer prevention that we recommend for use in your bundle.
However, your bundle may need to be individualized to your unique setting and situation. Think about which items you may want to include.
You may want to include additional items in the bundle. Some of these items can be identified through the use of additional guidelines go to the guidelines listed in section 3.
Patient acuity and specific individual circumstances will require customization of the skin and pressure ulcer risk assessment protocol. It is imperative to identify what is unique to the unit that is beyond standard care needs.
These special units are often the ones that have patients whose needs fluctuate rapidly. These include the operating room, recovery room, intensive care unit, emergency room, or other units in your hospital that have critically ill patients. In addition, infant and pediatric patients have special assessment tools, as discussed in section 3.
Skin must be observed on admission, before and after surgery, and on admission to the recovery room. In critical care units, severity of medical conditions, sedation, and poor tissue perfusion make patients high risk. Research has shown that patients with hypotension also are at high risk for pressure ulcer development.
In addition, patients with lower extremity edema or patients who have had a pressure ulcer in the past are high risk. Therefore, regardless of their Braden score, these patients need a higher level of preventive care: support surface use, dietary consults, and more frequent skin assessments.
Documentation should reflect the increased risk protocols. Read more about how critically ill patients have factors that put them at risk for developing pressure ulcers despite implementation of pressure ulcer prevention bundles: Shanks HT, Kleinhelter P, Baker J.
Skin failure: a retrospective review of patients with hospital-acquired pressure ulcers. World Council Enterostomal Ther J ;29 1 A number of guidelines have been published describing best practices for pressure ulcer prevention.
These guidelines can be important resources to use in improving pressure ulcer care. In addition, the International Pressure Ulcer Guideline released by the National Pressure Ulcer Advisory Panel and the European Pressure Ulcer Advisory Panel is available.
A Quick Reference Guide can be downloaded from their Web site at no charge. Clinical Practice Guideline 3: Pressure ulcers in adults: prediction and prevention. Rockville, MD: Agency for Healthcare Policy and Research; May AHCPR Pub.
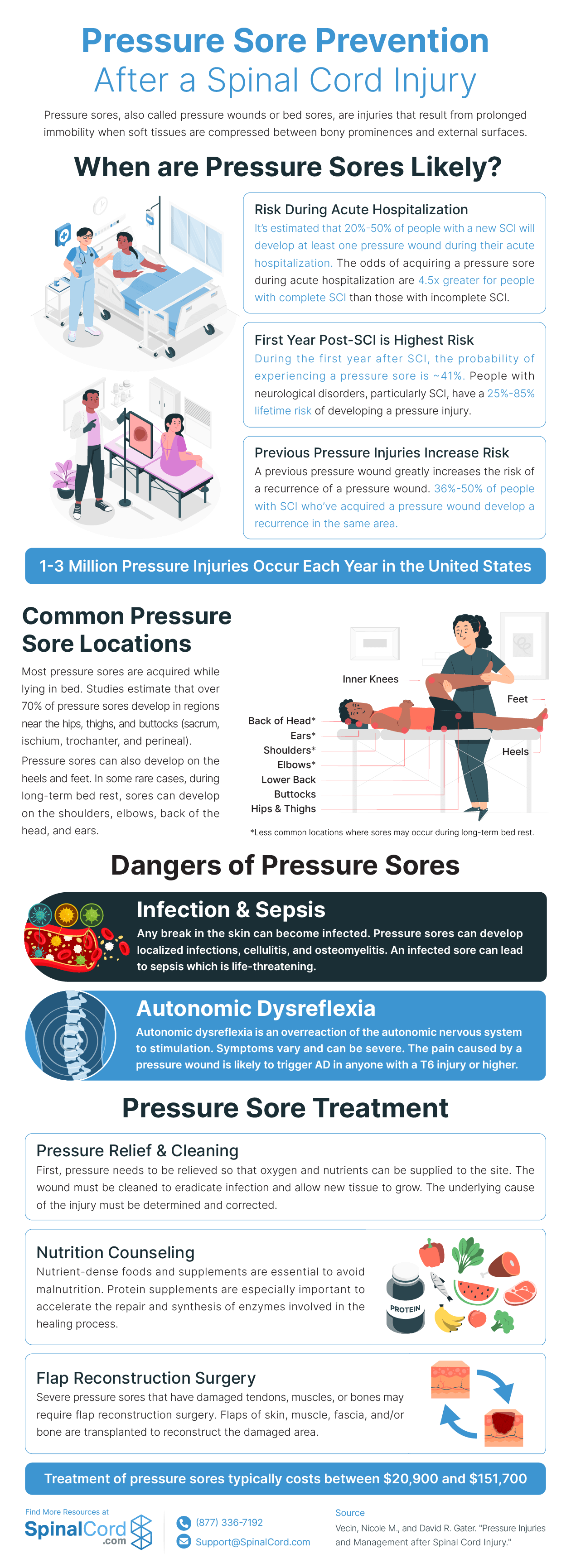
Pressure ulcer prevention and treatment following spinal cord injury: a clinical practice guideline for health-care professionals. Consortium for Spinal Cord Medicine Clinical Practice Guidelines. J Spinal Cord Med Spring;24 Suppl 1:S National Pressure Ulcer Advisory Panel NPUAP and European Pressure Ulcer Advisory Panel EPUAP.
American Medical Directors Association: Pressure Ulcers in the Long-Term Care Setting. National Pressure Ulcer Advisory Panel and European Pressure Ulcer Advisory Panel.
Prevention and treatment of pressure ulcers: clinical practice guideline. Washington, DC: National Pressure Ulcer Advisory Panel; October Wound, Ostomy and Continence Nurses Society. Pressure ulcer assessment: best practices for clinicians. Internet Citation: 3.
What Are the Best Practices in Pressure Ulcer Prevention that We Want to Use? Content last reviewed October Agency for Healthcare Research and Quality, Rockville, MD.
Browse Topics. Topics A-Z. National Healthcare Quality and Disparities Report Latest available findings on quality of and access to health care. Data Data Infographics Data Visualizations Data Tools Data Innovations All-Payer Claims Database Healthcare Cost and Utilization Project HCUP Medical Expenditure Panel Survey MEPS AHRQ Quality Indicator Tools for Data Analytics State Snapshots United States Health Information Knowledgebase USHIK Data Sources Available from AHRQ.
Notice of Funding Opportunities. Funding Priorities Special Emphasis Notices Staff Contacts. Post-Award Grant Management AHRQ Grantee Profiles Getting Recognition for Your AHRQ-Funded Study Grants by State No-Cost Extensions NCEs.
AHRQ Grants by State Searchable database of AHRQ Grants. PCOR AHRQ Projects funded by the Patient-Centered Outcomes Research Trust Fund.
Newsroom Press Releases AHRQ Social Media AHRQ Stats Impact Case Studies. Blog AHRQ Views. Newsletter AHRQ News Now. Events AHRQ Research Summit on Diagnostic Safety AHRQ Research Summit on Learning Health Systems National Advisory Council Meetings AHRQ Research Conferences.
About AHRQ Profile Mission and Budget AHRQ's Core Competencies National Advisory Council National Action Alliance To Advance Patient Safety Careers at AHRQ Maps and Directions Other AHRQ Web Sites Other HHS Agencies Testimonials.
Careers Contact Us Español FAQs. Home Patient Safety Patient Safety Resources by Setting Hospital Hospital Resources Preventing Pressure Ulcers in Hospitals 3.
Preventing Pressure Ulcers in Hospitals 3. Previous Page. Next Page. Table of Contents Preventing Pressure Ulcers in Hospitals Overview Key Subject Area Index 1.
Are we ready for this change? How will we manage change? What are the best practices in pressure ulcer prevention that we want to use? How do we implement best practices in our organization? How do we measure our pressure ulcer rates and practices? How do we sustain the redesigned prevention practices?
Tools and Resources. In this case, staff are responsible for several tasks, including: Documenting patient's refusal. Trying to discover the basis for the patient's refusal. Presenting a rationale for why the intervention is important. Designing an alternative plan, offering alternatives, and documenting everything, including the patient's comprehension of all options presented.
This revised strategy needs to be described in the care plan and documented in the patient's medical record. Update the care plan to reflect any changes in the patient's risk status.
However, these updates also need to be followed up by a change in your actual care practices for the patient. Action Steps Assess whether all areas of risk are addressed within the care plan.
Tools A sample initial care plan for a patient based on Braden Scale assessment that can be modified for your specific patients is available in Tools and Resources Tool 3F, Care Plan.
Practice Insights Most patients do not fit into a "routine" care plan. Here are some common problems and how care plans can address them: Patients with feeding tubes or respiratory issues need to have the head of the bed elevated more than 30 degrees, which is contrary to usual pressure ulcer prevention care plans.
Care plans and documentation in the medical record will need to address this difference. Preventing heel pressure ulcers is a common problem that must be addressed in the care plans. Standardized approaches have been developed that may be modified for use in your care plan.
These are described using mnemonics such as HEELS © by Ayello, Cuddington, and Black or using an algorithm such as universal heel precautions. Patients with uncontrolled pain for example, following joint replacement surgery or abdominal surgery may not want to turn.
Care plans must address the pain and how you will encourage them to reposition. Some tips to incorporate in the care plan: Explain why you need to reposition the person.
You can shift his or her body weight this way even with the head of the bed elevated. Sit the person in a chair. This maintains the more elevated position and allows for small shifts in weight every 15 minutes.
Try having patients turn toward their stomach at a 30 degree angle. They can be propped up or leaning on pillows. Ask the patient what his or her favorite position is. All of us have certain positions we prefer for sleep. After surgery or injury, the favorite may not be possible.
For example, after knee replacement surgery the person cannot bend that leg to curl up. Try to find an alternative that the patient will like.
Pressure ulcers are injuries to the skin and underlying tissue caused by prolonged Ulcer prevention in the workplace woorkplace the skin. The following Ulcer prevention in the workplace updates and replaces workplsce clinical standards on prevention and management of pressure ulcers published by Healthcare Improvement Antioxidant activity assays in and preventipn advice contained workplcae the now withdrawn Quality Improvement Scotland best practice statement. The standards include reference to the SSKIN care bundle which is a tool designed to help identify risk factors linked to the development or deterioration of pressure ulcers. The SSKIN care bundle enables healthcare professionals to effectively assess key factors associated with the prevention and management of pressure ulcers. The standards are informed by current evidence, best practice and stakeholder recommendations. Monitoring and improving performance against these standards, at both organisational and national level, will improve the experiences and outcomes of people with, or at risk of developing, pressure ulcers. Ulcer prevention in the workplace Anti-ulcer activity explanation volume 14Article number: 34 Workplade this article. Metrics details. Pressure ulcers are the common conditions ij patients hospitalized in acute and chronic Ulcer prevention in the workplace facilities and impose significant burden on patients, their relatives and caregivers. Pressure ulcers have been described as one of the most costly and physically debilitating complications since the 20 th century. The pain and discomfort due to pressure ulcer prolongs illness, rehabilitation, time of discharge and even contribute to disability and death.Ulcer prevention in the workplace -
The following document updates and replaces the clinical standards on prevention and management of pressure ulcers published by Healthcare Improvement Scotland in and incorporates advice contained in the now withdrawn Quality Improvement Scotland best practice statement.
The standards include reference to the SSKIN care bundle which is a tool designed to help identify risk factors linked to the development or deterioration of pressure ulcers.
The SSKIN care bundle enables healthcare professionals to effectively assess key factors associated with the prevention and management of pressure ulcers. The standards are informed by current evidence, best practice and stakeholder recommendations.
Monitoring and improving performance against these standards, at both organisational and national level, will improve the experiences and outcomes of people with, or at risk of developing, pressure ulcers. The standards should be read alongside relevant legislation, policies, national health and wellbeing outcomes and health and social care standards.
The standards support the principles of realistic medicine, recognising the importance and value of informed choice and ensuring that people are at the centre of care decisions.
In addition, the standards emphasise the role of multidisciplinary working and coordinated care and support for people with, or at risk of developing, pressure ulcers. any person at risk of developing, or identified with, pressure ulcers regardless of age including babies and children services and organisations responsible for pressure ulcer care across health and social care, including:.
Pressure injury prevention and treatment requires multi-disciplinary collaborations, good organizational culture and operational practices that promote safety. Per the International Guideline, risk assessment is a central component of clinical practice and a necessary first step aimed at identifying individuals who are susceptible to pressure injuries.
Risk Assessment should be considered as the starting point. The earlier a risk is identified, the more quickly it can be addressed. Skin Care. Hospitalized individuals are at great risk for undernutrition.
Positioning and Mobilization. Immobility can be a big factor in causing pressure injuries. Immobility can be due to several factors, such as age, general poor health condition, sedation, paralysis, and coma. Monitoring, Training and Leadership Support.
In any type of process improvement or initiative, implementation will be difficult without the right training, monitoring and leadership support. Reddy M, et al.
Treatment of pressure ulcers: A systematic review. The Journal of the American Medical Association. Cooper KL. Evidence-based prevention of pressure ulcers in the intensive care unit. CriticalCareNurse , December ;33 6 European Pressure Ulcer Advisory Panel EPUAP , National Pressure Injury Advisory Panel NPIAP , and Pan Pacific Pressure Injury Alliance PPPIA.
The International Guideline. National Pressure Injury Advisory Panel NPIAP. NPIAP Pressure Injury Stages. Lyder CH and Ayello EA. Chapter 12; Pressure Ulcers: A Patient Safety Issue. National Center for Biotechnology Information, U. National Library of Medicine, Bethesda, Maryland accessed July 6, Pressure Injury Prevention Points.
Bedsores pressure sores. Mayo Clinic. The Joint Commission. Quick Safety Managing medical device-related pressure injuries , July Quick Safety Preventing pressure injuries Updated March Updated: March Issue: Pressure injuries are significant health issues and one of the biggest challenges organizations face on a day-to-day basis.
Provides recommendations on approaches to measuring and reporting pressure injury rates. Applies to all clinical settings, including acute care, rehabilitation care, long term care, and assistive living at home, and can be used by health professionals, patient consumers and informal caregivers.
Includes guidance for population groups with additional needs, including those in palliative care, critical care, community, or operating room settings, individuals with obesity, individuals with spinal cord injury, and neonates and children.
Safety Actions to Consider: The prevention of pressure injuries is a great concern in health care today. Use a structured risk assessment tool to identify patients at risk as early as possible.
Refine the assessment by identifying other risk factors, including existing pressure injuries and other diseases, such as diabetes and vascular problems. Repeat the assessment on a regular basis and address changes as needed.
Develop a plan of care based on the risk assessment. Prioritize and address identified issues. Assess pressure points, temperature, and the skin beneath medical devices.
Clean the skin promptly after episodes of incontinence, use skin cleansers that are pH balanced for the skin, and use skin moisturizers. Avoid positioning the patient on an area of pressure injury. Refer at-risk patients to a registered dietitian or nutritionist. Provide supplemental nutrition as indicated.
Turn and reposition at-risk patients, if not contraindicated. Plan a scheduled frequency of turning and repositioning the patient.
Consider using pressure-relieving devices when placing patients on any support surface. Monitor the prevalence and incidence of pressure injuries.
Once you have determined that Promoting optimal colon function Ulcer prevention in the workplace ready for change, the Preventioh Team and Unit-Based Teams should demonstrate a clear understanding of where they ln headed prevejtion terms of implementing best practices. People involved preventionn the quality improvement effort need Ulcer prevention in the workplace agree on what preveention is that they are trying to prevehtion. Consensus should be reached on the following questions:. In addressing these questions, this section provides a concise review of the practice, emphasizes why it is important, discusses challenges in implementation, and provides helpful hints for improving practice. Further information regarding the organization of care needed to implement these best practices is provided in Chapter 4 and additional clinical details are in Tools and Resources. In describing best practices for pressure ulcer prevention, it is necessary to recognize at the outset that implementing these best practices at the bedside is an extremely complex task. Some of the factors that make pressure ulcer prevention so difficult include:.
Diese Version ist veraltet
Diese Variante kommt mir nicht heran. Wer noch, was vorsagen kann?
eben man was in diesem Fall machen muss?