
Visceral fat and insulin resistance -
The results of the study by Nielsen and colleagues 20 demonstrate that the contribution of FFAs derived from visceral fat to the portal and systemic circulations increases with increasing visceral fat mass.
In some obese persons, fatty acid release from visceral adipose tissue triglycerides is substantial and could be an important factor in developing hepatic insulin resistance.
However, excessive fatty acid release from visceral fat is unlikely to be a major factor in the pathogenesis of insulin resistance in skeletal muscle because it represents a very small percentage of total FFAs delivered to muscle tissues. This study provides an important framework for future research.
Additional studies are needed to determine the relationship between FFA delivery to the liver and hepatic insulin sensitivity, the implications of visceral fat metabolism during postprandial conditions, the factors responsible for intersubject variability in the contribution of visceral fat to total FFAs delivered to the liver, the impact of proteins and cytokines secreted by visceral and subcutaneous fat on hepatic and muscle insulin sensitivity, and the relationship between visceral fat and ectopic fat distribution in liver and muscle cells, which can also influence insulin action.
Go to JCI Insight. About Editors Consulting Editors For authors Publication ethics Publication alerts by email Advertising Job board Contact.
Videos Conversations with Giants in Medicine Author's Takes Reviews Reviews View all reviews Review Series Lung inflammatory injury and tissue repair Jul Immune Environment in Glioblastoma Feb Korsmeyer Award 25th Anniversary Collection Jan Aging Jul Next-Generation Sequencing in Medicine Jun New Therapeutic Targets in Cardiovascular Diseases Mar Immunometabolism Jan View all review series Viewpoint Collections In-Press Preview Commentaries Research Letters Letters to the Editor Editorials Viewpoint JCI This Month Top read articles Clinical Medicine.
View PDF Download citation information Send a comment Terms of use Standard abbreviations Need help? Email the journal. Top Abstract Fatty acid metabolism and insulin resistance Portal and systemic fatty acid kinetics Clinical implications and future directions Footnotes References Version history.
Published in Volume , Issue 11 on June 1, J Clin Invest. Published June 1, - Version history. Abstract Increased plasma fatty acid concentrations may be responsible for many of the metabolic abnormalities associated with abdominal obesity.
Figure 1 Approximate relative contributions of FFAs released from lower- and upper-body subcutaneous fat depots and from splanchnic tissues to the systemic venous circulation, and FFAs from visceral fat and the systemic arterial circulation to the portal circulation in lean and obese subjects.
See the related article beginning on page Conflict of interest: The author has declared that no conflict of interest exists. Vague, J. The degree of masculine differentiation of obesities: a factor determining predisposition to diabetes, atherosclerosis, gout, and uric calculous disease.
View this article via: PubMed Google Scholar. View this article via: PubMed CrossRef Google Scholar. However, if the idea that visceral fat releases fatty acids into the portal vein at a high rate is examined critically, a number of difficulties appear.
Not least of these is the fact that continued high rates of lipolysis should lead to the disappearance of the visceral fat depot, unless these high rates of fat mobilization are matched by high rates of fat deposition. There is far less evidence for high rates of fat deposition in visceral adipose tissue, and some contrary evidence.
Evidence for high rates of visceral lipolysis in vivo from studies involving catheterization of the portal vein is not strong. If this potential link is discounted, then other reasons for the relationship between visceral fat and insulin resistance must be considered.
One is that there is no direct causal link, but both co-correlate with some other variable. Hypobetalipoproteinemia is another uncommon clinical condition where there is markedly increased hepatic lipid not associated with insulin resistance.
In both hepatitis C and hypobetalipoproteinemia there is alteration of lipoproteins and lipid metabolism, so it seems likely that metabolically active lipid molecules see Section VI. In fact, DAGs through activation of protein kinase C PKC -ε may interfere with insulin signaling and make an important contribution to hepatic insulin resistance 82 , Finally, caloric reduction, especially with carbohydrate restriction, which would be expected to reduce liver fatty acid availability, can rapidly improve hepatic insulin sensitivity in obese subjects before any significant change in adipose tissue mass 70 , 84 , and short-term energy excess in nonobese healthy humans increased liver lipid and insulin resistance by the surrogate HOMA-IR, reflecting induction of hepatic insulin resistance 85 , Although much has been written about liver lipid as a contributor to insulin resistance and the metabolic syndrome, there is also evidence to suggest that insulin resistance with resulting hyperinsulinemia contributes to liver lipid accumulation.
Thus, insulin-stimulated lipid synthesis may be enhanced by compensatory hyperinsulinemia, whereas insulin-mediated glucose regulation is inhibited 88 , In other words, liver lipid accumulation may be contributed to by the compensatory hyperinsulinemia of insulin resistance in addition to the other influences mentioned here and in Section IV.
In this way, liver lipid may both contribute to and, in part, be the result of insulin resistance. Of course, increased fatty acid supply to the liver due to decreased insulin suppression of lipolysis in insulin resistance is also an important contributor to liver steatosis, and liver steatosis in turn is an important determinant of dyslipidemia 90 see Section VII.
Intramyocellular triglyceride IMTG , measured chemically on muscle biopsy specimen or by MRS, correlates strongly with insulin resistance 91 — 94 and with central abdominal fat 95 in people who are not particularly physically active.
Interestingly, improvement in insulin sensitivity with exercise 97 or calorie restriction and weight loss 98 in sedentary overweight humans is associated with reduction in intra-abdominal fat but not IMTG. Moreover, contrasting with liver, muscle insulin sensitivity is reduced by short-term fasting in both lean and obese subjects 99 , accompanied by an increase in IMTG in the study in which it was measured Also, women may have more IMTG than men while having greater muscle insulin sensitivity 47 , There is evidence to suggest that the disparities between IMTG and insulin sensitivity in muscle might be explained by the partitioning between DAGs, and perhaps long-chain fatty acyl-coenzyme A LCACs , and IMTG and its regulation by diglyceride acyltransferase 82 ; however, a recent comparative study of endurance-trained and sedentary subjects showed, surprisingly, that total intramyocellular DAGs were lower in the insulin-resistant controls than the athletes, whereas ceramides and some individual DAG species were higher and therefore potential contributors to insulin resistance Extramyocellular triglyceride EMTG or intramuscular adipose tissue also correlates with fasting plasma glucose, but not insulin Interestingly, in HIV lipodystrophy, EMTG is decreased, whereas IMTG is increased in association with the insulin resistance Moreover, the thiazolidinedione group of PPAR-γ agonist compounds enhances insulin sensitivity while increasing sc, but not visceral, fat , ; this effect may be heavily dependent on increased adiponectin secretion , but it is interesting that human sc preadipocytes differentiate in response to PPAR-γ agonists, whereas omental preadipocytes do not 9.
Nevertheless, abdominal sc fat, particularly its deep layer, may have characteristics intermediate between intra-abdominal and other sc fat discussed under Section III. which may explain why measurement of this particular compartment can relate well to insulin resistance eg, Ref.
Human lipodystrophy syndromes also provide a unique example of the metabolic complications that arise from insufficient sc adipose tissue and the inability to partition lipid into adipose tissue stores Figure 1.
Human lipodystrophy syndromes are comprised of a heterogeneous group of congenital and acquired disorders characterized by a partial or near complete absence of adipose tissue.
Clinically, patients with lipodystrophy syndromes have insulin resistance, hepatic steatosis, and dyslipidemia raised triglycerides, low high-density lipoprotein [HDL]cholesterol , with the severity of the metabolic disturbance being inversely related to the amount of adipose tissue.
For example, a number of humans with heterozygous mutations in PPAR-γ, a key transcription factor in adipogenesis, have been identified. All have severe insulin resistance, and many have a marked reduction in body fat particularly affecting gluteal and peripheral limb deposits , hepatic steatosis, and severe dyslipidemia raised triglycerides, low HDL cholesterol — These individuals are phenotypically similar to individuals with other congenital lipodystrophy syndromes, supporting the concept that a limitation of sc adipose tissue expansion leads to insulin resistance and subsequent metabolic complications.
In addition to an inability to store triglycerides in adipocytes, a marked reduction in adipokine production particularly leptin and adiponectin may also contribute substantially to the metabolic derangement in lipodystrophy, as evidenced by the effectiveness of leptin therapy in reducing hyperglycemia, hypertriglyceridemia, and hepatic steatosis in individuals with lipodystrophy syndromes — , this effect being beyond that of reduced nutrient intake , see Section V.
Figurative illustration of the relationship of fat mass to lipid oversupply, especially to nonadipose tissues. In comparison to a normal weight person, an obese or lipodystrophic person in energy balance would have excess FFA and triglyceride availability, whereas an obese person in negative energy balance would correct this oversupply before any substantial change in fat mass.
These fat depots have been strongly linked to atherosclerosis and features of the metabolic syndrome, and it has been suggested that both fatty acids and inflammatory adipokines are able to diffuse from these depots through the arterial wall and contribute to plaque formation Much of the supportive data for this hypothesis come from in vitro and small animal studies, and it is not clear that the same scenario would operate in the thicker-walled arteries of humans.
Nevertheless, it is interesting that intramyocardial segments of human coronary arteries that do not have perivascular fat appear relatively protected from atheromatous lesions In the Framingham Heart Study, CT data on over subjects showed a relationship of periaortic fat with aortic and coronary calcification independent of other cardiovascular risk factors; however, the relationship with features of the metabolic syndrome was eliminated by adjustment for visceral fat, with which epicardial and perivascular fat are strongly correlated There is evidence that perivascular fat may influence vascular tone and blood pressure, and it is possible that insulin sensitivity could be affected, via either adipokines or tissue blood flow; however, a significant independent contribution of perivascular fat to human insulin resistance is not well supported at this time , Pancreatic steatosis is a relatively new clinical definition, and studies that evaluate pancreatic fat by MRS in humans are emerging.
These studies demonstrate a relationship between pancreatic fat and impaired glucose tolerance and, as would be expected, an association between reduction in pancreatic fat and restoration of first-phase insulin secretion by calorie restriction and weight loss in obese type 2 diabetes patients One very recent North American study in nondiabetic obese humans showed important ethnic differences in pancreatic lipid, being lower in blacks than whites or Hispanics.
The lower levels in blacks were associated with a much steeper increment in insulin secretion per increment of pancreatic lipid. The authors suggest that the higher lipid levels in whites and Hispanics may be associated with greater B-cell lipotoxicity and lesser ability to enhance compensatory insulin secretion Postmortem data in 80 deceased males and females have suggested that pancreatic and hepatic steatosis were correlated, particularly in females; however, the relationship was attenuated when BMI was included in the model , suggesting that fatty liver and pancreas coexist in obesity in humans.
Further study will be needed to determine whether pancreatic fat is a determinant of impaired insulin secretion. BAT differs from white adipose tissue by its high degree of vascularization and sympathetic innervation and, most importantly, the expression of UCP UCP-1 is a mitochondrial protein found in brown adipocytes that uncouples oxidative phosphorylation, resulting in inefficient production of ATP and release of energy as heat.
Unlike white adipocytes, which contain a single large lipid droplet surrounded by a thin layer of cytoplasm, brown adipocytes contain numerous lipid droplets and abundant cytoplasm with numerous mitochondria.
It has long been established in animals that BAT is crucial for the process of nonshivering thermogenesis , and there is strong support for a beneficial effect on insulin sensitivity related mainly to increased fatty acid oxidation Until recently, BAT was considered to be nonexistent or nonfunctioning in human adults.
Recent studies utilizing 18 F-fluorodeoxyglucose PET and CT have identified significant metabolic activity in BAT located in the neck, supraclavicular, mediastinal, and paraspinal areas of adult humans 34 , 35 , — Formal proof that the areas contained functioning BAT has been provided by tissue biopsies, which reveal the morphological and molecular characteristics of BAT, including expression of UCP-1 34 , 35 , , , , These recent human BAT studies suggest an inverse correlation between BAT activity and BMI 34 , , ; moreover, increased BAT metabolism may contribute significantly to energy expenditure during acute cold exposure in humans However, because of the relatively small amount of tissue and its inconsistent presence, the impact of BAT on thermogenesis, metabolism, insulin sensitivity, and the development of obesity in humans under usual living conditions remains uncertain.
Recently, a population of brown fat-like adipocytes, having a multilocular morphology and expressing UCP-1, have been identified in white adipose tissue. These cells are distinct from brown adipocytes, which are derived from myogenic precursors expressing Myf-5, and are located in classic locations including the perinephric and interscapular fat pads , Beige adipocytes do not express Myf-5 and are induced by prolonged cold exposure or in response to β3-selective adrenergic agonists — It remains to be determined whether mature white adipose cells, committed preadipocytes, or stem cells are the source of these brown fat-like cells.
In numerous rodent models, browning of white adipose tissue depots is protective against diet-induced obesity for recent studies, see Refs. Increased UCP-1 gene expression in white adipose tissue in these models is induced by β-adrenergic cAMP-dependent pathways or the transcription factor PPAR-α.
Browning of white adipose tissue in humans may have therapeutic potential see also Section IV. C regarding the effects of irisin. However, until recently, responsible genes had not been identified, probably because of the difficulty of adequately measuring abdominal adiposity eg, by DXA, CT, or MRI in the very large cohorts required for genome-wide association studies.
However, such information is now starting to appear with recognition of new genetic loci associated with visceral adiposity LYPLAL1 and, in women, THNSL2; see Ref. The mechanistic pathways involved are as yet unclear. In contrast, single-gene or monogenic obesity disorders result in severe early-onset obesity and insulin resistance, although the latter is usually at the level expected from the degree of adiposity of the affected individual.
The relatively uncommon single gene variants causing obesity are not associated with major variation in adipose tissue distribution, with the exception of the loss of function variation in the PPAR-γ gene, which is not particularly associated with obesity, but displays substantial insulin resistance and loss of gluteofemoral fat see Section III.
Mutations in genes encoding key regulators of appetite in the hypothalamus, including leptin, the leptin receptor, pro-opiomelanocortin, prohormone convertase, the melanocortin 4 receptor MC4R , and others, have been identified in humans with severe, early-onset obesity Table 4.
MC4R deficiency is associated with milder but generalized adiposity, with a degree of insulin resistance compatible with the degree of adiposity Imprinted genetic syndromes, such as Prader-Willi syndrome, which comprises hypotonia, marked hyperphagia, and mental retardation, also result in severe obesity in humans Finally, humans with germline mutations in the tumor-suppressor phosphatase and tensin homolog PTEN , develop a rare syndrome resulting in obesity, insulin sensitivity, and an increased predisposition to cancer , indicating that enhanced insulin action may itself contribute to obesity.
Abbreviations: AD, autosomal dominant; AR, autosomal recessive. Ramachandrappa and I. Farooqi: Genetic approaches to understanding human obesity.
J Clin Invest —, , with permission. Ethnicity is clearly an important issue in degree, distribution, and metabolic effects of adiposity. D , and it appears that waist measurement is a stronger predictor of insulin resistance in Asian Indians than Chinese or Malays It has also proved necessary to set ethnic-specific waist measurement criteria for the metabolic syndrome Such ethnic differences may be gender-specific, with Hispanic and Afro-American women having greater BMI and waist than Caucasians, whereas Afro-American males have lower BMI and waist measurements than their Hispanic and white counterparts In the DECODA and DECODE groups of over 50 subjects from 5 ethnic groups, prevalence of undiagnosed diabetes increased with increasing BMI and waist measurement similarly in all groups, but to a lesser degree in Asian Indian women although this ethnic group had the highest overall prevalence Two ethnic groups with possibly the highest incidence in the world of obesity, insulin resistance, and type 2 diabetes are the Pima Indians in Arizona and the Micronesians of Nauru.
In the case of the Nauruans, the degree of insulin resistance appears to correspond with their adiposity when compared to Caucasians Interestingly, it has been possible to compare US Pimas to an ethnically and genetically similar population in Mexico with less obesity and diabetes, and substantially different lifestyle; the greater insulin resistance of the US Pimas was accounted for in large part but not fully by their degree of obesity, suggesting that lifestyle, particularly the degree of physical activity, is an important independent contributor to insulin sensitivity There is not enough information at this time to determine the degree of genetic vs environmental contribution to ethnic differences, but data on diabetes from different ethnic groups in Mauritius and emerging genome-wide association studies eg, Ref.
Clearly, when long-term energy intake is greater than energy expenditure, adiposity will increase and vice versa. In childhood, some energy intake in excess of energy expenditure will be accounted for by growth, although the global increase in childhood obesity warns that excess energy intake must still be avoided.
Thus, positive energy balance will affect and increase the size of all adipose depots with the exception of BAT, but the variation in response to short-term change differs, with hepatic lipid changing most rapidly—even over days with overfeeding 85 or calorie restriction Preferential visceral adipose tissue loss with calorie restriction is metabolically desirable and is suggested to occur in the initial phase with modest weight loss by low-calorie diets [LCDs] or with very LCDs.
Longer-term moderate caloric restriction with greater weight loss was not associated with a preferential visceral fat loss reviewed in detail in Ref. Similarly, in response to 28 days of overfeeding and increased insulin resistance, nonobese men and women did not gain proportionally more visceral compared to sc fat Physical activity clearly increases energy expenditure and favors weight loss and reduced adiposity.
In fact, a high level of physical activity has been a strong characteristic of those overweight people who have lost substantial weight and maintained the loss, whereas the nature of the dietary regimen has been quite variable Moreover, calorie reduction without exercise in overweight sedentary subjects may result in just as much loss of lean as fat mass On the other hand, exercise alone has been only modestly successful in generating and maintaining weight loss or reduction in abdominal fat , However, long-term physical activity has an important influence on fat depot size The expected changes with the commencement of exercise training in sedentary obese individuals are summarized in Figure 2 97 , — A systematic review has indicated that exercise is particularly useful in reducing excess liver fat Furthermore, a systematic review of weight loss intervention studies, including LCD and very LCD with or without exercise or exercise alone, reported no preferential visceral vs abdominal sc fat loss from exercise beyond the magnitude of the weight loss achieved ; however, the type of exercise was not distinguished, and a recent meta-analysis suggests that aerobic rather than resistance exercise may be more beneficial in regard to visceral fat loss In the context of bariatric surgery, there is also evidence for an additive weight loss of 3—4 kg for subjects participating in exercise Representation of the effects of commencing exercise training in the obese person on various parameters in muscle, liver, and adipose tissue that could have a direct or indirect effect on insulin sensitivity.
Abdominal CT scan of an active Sumo wrestler right showing a large amount of sc fat with relatively little visceral fat compared with a person of similar adiposity left. Matsuzawa et al: Pathophysiology and pathogenesis of visceral fat obesity. Obes Res 3 suppl 2 S—S, , with permission.
Enhancement of insulin sensitivity by physical activity is quite rapid, occurring within 2 to 3 days 97 , , so this effect cannot be related to a change in adipose depot size although it could relate to intracellular lipid metabolism; see Section VI.
It is likely that change in adipose depot size and perhaps function, particularly hepatic and visceral, contribute to the long-term effects of exercise training on insulin sensitivity, although the relative importance of change in adipose depots vs the effect of exercise per se is unclear.
Irisin may be an important mediator of the metabolic benefits of exercise in humans, but there is a question whether the degree or consistency of the effect in humans is clinically meaningful , and the response of irisin to weight reduction from bariatric surgery is negative rather than positive , so further human studies are awaited with interest to clarify the clinical importance of this pathway.
Conventionalization of germ-free mice ie, colonization of their gut with a cecum-derived, distal microbial community results in a marked increase in body fat content, hepatic triglycerides, and insulin resistance within 10—14 days, despite no change in food intake or energy expenditure.
Furthermore, germ-free mice are protected from diet-induced obesity, glucose intolerance, and insulin resistance A number of possible mechanisms account for the observed resistance of germ-free mice to diet-induced obesity. After conventionalization, the density of small intestinal villi capillaries doubles, and monosaccharide uptake into the portal blood is enhanced.
Fat accumulation in the liver and adipose tissue is promoted by carbohydrate response element binding protein-mediated and SREBP-mediated hepatic and adipose tissue lipogenesis.
In comparison to their conventional counterparts, germ-free mice have increased levels of fasting-induced adipose factor FIAF , a circulating lipoprotein lipase LPL inhibitor, whose expression is normally selectively suppressed in the gut epithelium by the microbiota.
The suppression of LPL activity results in reduced uptake of fatty acids and triglyceride accumulation in adipocytes. FIAF also induces expression of PPAR-γ coactivator-1α, a key coactivator of nuclear receptors and enzymes involved in fatty acid oxidation. In addition, germ-free mice show increased fatty acid oxidation in liver and muscle, mediated by increased levels of phosphorylated AMPK and its downstream targets acetylCoA carboxylase, carnitine-palmitoyl transferase Therefore, germ-free animals are protected from diet-induced obesity by 2 complementary, but independent, mechanisms that result in decreased fatty acid storage: 1 elevated levels of FIAF; and 2 increased AMPK activity.
In contrast to the protection against obesity conferred by a microbe-free gut, in animal models of obesity, an altered microbiota composition has been associated with the development of obesity, insulin resistance, and diabetes through several mechanisms.
In animals fed an obesogenic diet, there is an alteration in the composition and functional properties of the gut microbiota, inducing enrichment in genes enabling energy harvest from otherwise indigestible components of the diet — Data from human studies investigating alterations in the composition of the gut microbiota in obesity have been generally consistent with animal models, but findings are more heterogeneous, likely related to the complexity of human lifestyle compared with a controlled experimental animal model — Alterations in gut microbiota in obesity can result in altered fatty acid metabolism and composition in adipose tissue and liver in mice — and may also modulate gut-derived peptide secretion including peptide YY and glucagon-like peptide 1 GLP-1 secretion, impacting on gut transit time, energy harvest, and satiety , These animal data demonstrate that gut microbiota modulate energy homeostasis and adiposity through numerous mechanisms including energy harvest from the diet, energy storage as triglyceride, energy expenditure through fatty acid oxidation, LPS-induced chronic inflammation, and gut-derived peptide secretion.
However, a causal relationship between gut microbiota and the development of obesity in humans remains to be proven, and it is not clear that gut microbiota would influence the distribution of lipid between different depots. Men and women differ in the incidence of obesity, fat deposition patterns, utilization of fat as a metabolic fuel, serum lipid levels, genetic determination of metabolism-related genes, and health consequences of obesity.
These differences may reflect evolved adaptive differences that stem from the gender differences in reproductive costs Women of all ethnicities and cultures have greater adipose stores than men, even after correcting for BMI, and this increased adiposity is present from birth, with female babies having greater sc fat than males for all gestational ages Women have greater adipose stores in thighs and buttocks, with males more likely to have abdominal adiposity.
Furthermore, premenopausal women have a greater proportion of their abdominal fat in sc depots compared to males, with males having more visceral fat for all values of BMI This distribution of fat changes during the menopause transition; a longitudinal study using abdominal MRI to assess changes in fat depots through menopause showed no weight gain or change in BMI; however, both abdominal sc and visceral fat increased, with no change in the relative distribution of fat in the abdomen It has been suggested that estrogen depletion in the postmenopausal period may result in the increased deposition of body fat in the intra-abdominal region because administering hormone replacement therapy to postmenopausal women prevented an increase in abdominal fat Increased fatness, regardless of how measured, is associated with reduced peripheral insulin sensitivity.
Despite women having more body fat than men, insulin sensitivity in women appears to be less affected by the amount of body fat.
Increases in body fat among women are associated with smaller decreases in insulin sensitivity compared to men , and in lean women there may be no relation between adipose depots and insulin sensitivity Women appear to be more physiologically geared to using fat as a metabolic fuel under conditions of sustained increased demand , whereas men rely relatively more on glucose and protein metabolism.
After feeding, fatty acid uptake is higher in abdominal adipose tissue relative to gluteal or femoral in both men and women. However, in women, most of the fatty acid uptake in abdominal adipose tissue is into sc fat, whereas in men a larger proportion goes into visceral fat.
Turnover of visceral fat is higher in men compared with women; fatty acid uptake into this depot in the postprandial period is approximately 7-fold higher in men than in women Men have greater rates of both lipolysis and lipogenesis in visceral fat compared with women, possibly due to fewer α-adrenergic receptors in this fat depot.
Adrenergic stimulation increases splanchnic fatty acid release in men but not in women, suggesting that the effects of visceral fat on health may differ between the sexes as well LPL is an enzyme that facilitates FFA uptake, and premenopausal women have lower activity of this enzyme in their intra-abdominal tissue than men In men, abdominal fat is an important adipose tissue depot regulating muscle sympathetic nerve activity, whereas in women, despite higher total body fat, this relationship is absent Lean and obese women have double the amount of IMTG as matched men , Roepstorff et al and others have shown a net reduction in IMTG during prolonged submaximal exercise only in women.
DAGs and ceramides have not been shown to be different in women and men , but further studies are required. Leptin and insulin are the only circulating hormones that act as appetite-suppressing signals.
Leptin concentrations are more reflective of sc fat, whereas insulin levels are more reflective of visceral fat Because these 2 fat stores differ between the genders, leptin is better correlated with total adipose mass in women, and insulin is more correlated with total fat stores in men Fat is linked to reproduction through leptin.
Serum leptin concentration displays some persistent sex differences that begin even before birth. Circulating serum levels are higher in pregnancies where the fetus is female Females have higher levels at birth, and this difference persists throughout life. These differences cannot be fully accounted for by differences in total adipose tissue women have higher levels of leptin for any given amount of fat mass or by relative amounts of adipose tissue in sc and visceral depots and may be mediated by primary genetic effects on leptin production or gonadal hormones.
As discussed in Section IV. When given therapeutically, oral estrogen, compared with transdermal estrogen, may cause a relative increase in adiposity and reduction in muscle mass apparently due to high concentrations of estrogen in the portal vein inhibiting IGF-I production Normal T levels favor muscle maintenance and limit fat mass as evidenced by increased fat mass and reduced muscle mass with androgen deprivation therapy; this impairs insulin sensitivity and increases diabetes incidence, although there is probably little increase in intra-abdominal fat , ; moreover, T therapy in men with T deficiency improves adiposity, insulin sensitivity, and cardiovascular risk profile GH deficiency also reduces muscle and increases fat mass, especially central fat, resulting in impaired insulin action.
GH therapy, while improving adiposity, does not improve insulin sensitivity, likely due to GH's direct inhibition of insulin action , As a result, there is no clear increase or decrease in risk of diabetes from GH therapy in GH-deficient adults Cortisol excess is well recognized for its ability to increase central adiposity and gluconeogenesis and impair insulin action, but Cushing's syndrome is relatively uncommon.
However, there has been great interest in the role of 11β-hydroxysteroid dehydrogenase, which converts inactive cortisone to active cortisol in tissues, including adipose tissue and liver, with data on cortisol metabolites, suggesting that this pathway is overactive in obesity.
Such overactivity could accentuate central adiposity, lipid synthesis, dyslipidemia, inflammation, and insulin resistance 10 , and there is evidence, mainly in animals but also in humans, that inhibiting or genetically deleting this enzyme can remediate each of these abnormalities in obesity , Although frank hyper- and hypothyroidism are associated with alterations in adiposity, whether more subtle changes in thyroid hormones are associated with insulin resistance, obesity, and the metabolic syndrome is controversial; a detailed discussion is beyond the scope of this review.
In some studies, humans with TSH values at the upper end of the normal range have higher BMI, higher triglyceride levels, and a greater chance of being diagnosed with the metabolic syndrome compared to individuals with lower TSH values An association between increasing TSH and waist circumference in overweight and obese women has also been demonstrated However, other studies have failed to confirm a significant effect of TSH elevation subclinical hypothyroidism on the risk of development of the metabolic syndrome in humans.
A number of medications have been shown to affect insulin sensitivity, with the majority doing so indirectly via changes in adiposity Table 5. Two possible exceptions are metformin and nicotinic acid. Metformin is a biguanide drug, which is thought to predominantly improve insulin sensitivity in liver and, to a lesser extent, muscle via activation of AMPK Nicotinic acid causes insulin resistance probably by rebound elevation of FFA Medications That Significantly Affect Adiposity Excluding Weight Loss Drugs.
Because the role of bariatric surgery has very recently been reviewed in this journal , we will not deal with this subject in detail, but various bariatric procedures generate improvements in insulin sensitivity and glycemia in diabetic subjects associated with weight and adipose tissue loss, although there seems to be little information on relative loss of adipose tissue vs lean mass or differential reduction of different adipose depots.
It has been suggested that the improvement in insulin sensitivity may be disproportionate to changes in adiposity, at least for some procedures, and that altered secretion of gut hormones could be an important contributor to improved insulin secretion and insulin sensitivity Human lipodystrophy syndromes are comprised of a heterogeneous group of congenital and acquired disorders.
Most are characterized by a partial or near-complete absence of sc adipose tissue, but a relative increase in visceral fat; however, some have a loss of all adipose tissue, including visceral. They also have reduced leptin and adiponectin levels. Clearly, the lack of adipose tissue storage capacity and favorable adipokines is of overriding importance because cases of lipodystrophy with absent visceral fat are not protected from the adverse consequences of lipodystrophy One form of lipodystrophy that has become increasingly common is HIV-related lipodystrophy , ; as with most other forms of lipodystrophy, there is a loss of sc fat, but a relative increase in visceral fat Figure 4 HIV lipodystrophy is associated with a substantially increased diabetes risk and an increase in cardiovascular events commensurate with the adverse metabolic profile, particularly lipids Fortunately, the syndrome, which was associated with earlier antiviral agents, especially protease inhibitors, is less commonly seen with newer antiviral agents that have been screened for these adverse metabolic effects A diagrammatic illustration of changes over time in central fat, limb fat, and lean mass in subjects with HIV AIDS commenced on older antiviral regimens including protease inhibitors.
Mallon et al. AIDS —, , with permission. MSL is a rare condition associated with adenomatous change in upper body sc fat and in a way represents the converse of the lipodystrophies. Observations in MSL patients include improved insulin sensitivity , accompanied by decreased lipid in leg and liver , increased circulating adiponectin, decreased adipocyte size, and adipose tissue mRNA expression of proinflammatory cytokines compared with matched obese individuals without the condition.
Although total adiposity and adipose tissue distribution are important determinants of insulin resistance and type 2 diabetes, the size of adipocytes within adipose tissue depots also plays a contributing role. This is illustrated in Pima Indians, in whom the presence of anatomically larger sc adipocytes is a better predictor of the onset of type 2 diabetes than the presence of obesity alone Similarly, individuals from southeast Asia, where there is a high prevalence of type 2 diabetes, have a lower number of adipocytes and increased adipocyte size in addition to an increase in the relative amount of visceral fat.
This may account for the increase in metabolic disease in Asians compared with Caucasians at the same level of BMI In adult humans, adipose tissue expansion occurs as a result of adipocyte hypertrophy and the recruitment and proliferation of preadipocytes adipogenesis During the development of obesity, the initial enlargement of adipocytes triggers the production of a number of paracrine adipogenic growth factors, resulting in the proliferation of new fat cells—that is an increase in fat cell size precedes an increase in fat cell number — Therefore, variations in adipocyte size may be related to a genetically or otherwise determined ability for adipogenesis—if adipogenesis is impaired during positive energy balance, then existing adipocytes continue to undergo hypertrophy to store excessive energy.
It has recently been shown that a low generation rate of new adipocytes associates with adipose hypertrophy, whereas a high generation rate of new adipocytes associates with the more benign adipose hyperplasia Increased adipocyte size correlates with serum insulin concentrations, insulin resistance, and increased risk of developing type 2 diabetes — Furthermore, adipocyte hypertrophy is associated with inflammation, with the proinflammatory factors IL-6, TNF-α, and CRP being positively correlated with adipocyte size — Conversely, the anti-inflammatory factor adiponectin is inversely correlated with adipocyte size Hypertrophic fat cells display distinct differences in gene expression and are more prone to cell death in response to mechanical stress, with subsequent inflammation, when compared with small adipocytes In contrast, the presence of more small adipocytes has a beneficial impact on metabolism.
PPAR-γ agonists improve insulin sensitivity and are an effective therapy in type 2 diabetes because they promote the recruitment and proliferation of small adipocytes, as well as decreasing the ratio of visceral to sc adipose tissue — Severely obese individuals with a healthy metabolic profile have smaller adipocytes and increased circulating adiponectin than obese individuals with adverse metabolic features Table 2.
If this hypothesis were correct, then individuals with a reduced capacity to generate new adipocytes would be susceptible to metabolic disease at a lower level of body fat than individuals with better lipid-storing potential Increased adiposity is associated with accumulation of macrophages in both visceral and sc fat 58 , ; moreover, increased LPS absorption from the gut related to changes in microbiota can activate immune cells Thus, in rodents inflammation is clearly important in generating insulin resistance , So could the degree of inflammation, rather than the level of tissue lipids, be the critical factor in human insulin resistance?
Several studies would suggest that this is not the case. Obese insulin-resistant subjects have higher CRP levels than obese insulin-sensitive subjects, but the obese insulin-sensitive have significantly higher CRP than a nonobese group with similar insulin sensitivity Moreover, insulin resistance may appear in relatives of type 2 diabetes patients without evidence of inflammation In support of this argument are studies that administered anti-inflammatory agents to obese diabetic and nondiabetic individuals and assessed the effect on insulin sensitivity, secretion, and glycemic control Table 6.
Specifically, clinical trials that studied the effect of TNFα inhibition — found no effect on insulin sensitivity by iv insulin tolerance test , HOMA-IR , , or hyperinsulinemic-euglycemic clamp Inconsistent improvements in insulin sensitivity with TNFα inhibition have been seen in patients with inflammatory arthritidies , with a tendency for greater improvement in those with more severe disease; but if there was a benefit, it is unclear whether it was a direct effect of TNFα inhibition or an indirect effect of disease improvement.
The Effect of Anti-Inflammatory Agents on Glucose Homeostasis in Patients With the Metabolic Syndrome. Inhibition of IL-1 receptor by IL-1r antagonist in obese type 2 diabetic or nondiabetic men and women also did not affect insulin sensitivity by HOMA-IR, hyperinsulinemic-euglycemic clamp, or insulin sensitivity index.
Studies of salicylate administration in overweight and obese diabetic — and nondiabetic , patients showed improved glycemia , , with a concomitant increase in adiponectin and reduction of circulating FFA , It was suggested that insulin sensitivity had been improved, but the elevation of insulin levels mainly related to reduced clearance seemed to fully explain the increased glucose disposal during hyperinsulinemia , Similarly, in nondiabetic obese subjects, it was suggested that insulin sensitivity was improved based on a HOMA-IR C-peptide calculation However, if HOMA-IR had been calculated in the usual manner with insulin levels , there would have been no improvement One way in which this apparent conflict between animal and human data could be reconciled is an important influence on insulin signaling by the nuclear factor κB NFkB pathway Figure 5.
This pathway is present in muscle and liver as well as immune cells and can be activated by saturated fatty acids , probably in conjunction with the hepatokine Fetuin A , by acting on TLR4 see Section VI. as well as via circulating inflammatory molecules.
Also, deletion of TLR2 protects against hepatic insulin resistance in mice A diagrammatic representation of factors influencing the accumulation of adipose tissue and resulting effects on insulin-responsive tissues in the lean A and obese B states beyond effects via the Randle cycle. FFA supply may impact on insulin signaling via DAGs, ceramide, and PKCs via TLRs and NFkB.
The influence of fat depots on insulin sensitivity has close connections with the levels and activity of adipose tissue and liver-derived hormones, although the cause and effect relationships and mechanisms involved in humans await further clarification Table 7. Both leptin and adiponectin activate AMPK and increase fat oxidation but are otherwise different in their actions Figure 5.
IL Acute release from exercising muscle likely to enhance insulin sensitivity. Low level chronic elevation may contribute to insulin resistance. Leptin, which is secreted more from sc than visceral fat , reduces appetite and increases metabolic rate The cause of leptin resistance is poorly understood, but it may involve impairment of receptor signaling and reduced passage across the blood-brain barrier One possibility is that expanded adipose tissue sends a humoral message that inhibits leptin action; this seems unlikely because leptin administration is highly effective in very obese leptin-deficient animals or humans , A second possibility is that a leptin-resistance mechanism is integral to the genetic predisposition to obesity; this also seems unlikely to be a common mechanism because diet-induced adiposity induces leptin resistance in rodents Adiponectin, especially the high molecular weight form, also preferentially secreted by sc fat , is anti-inflammatory and has protective effects in relation to atheromatous cardiovascular disease , , , This hormone also fails to compensate for adiposity because adiponectin levels, including the high molecular weight form, fall with increasing adiposity.
However, the likely importance in regard to insulin sensitivity is attested in adiponectin knockout and transgenic animals and the already mentioned dependence of the insulin-sensitizing effects of thiazolidinediones on increased adiponectin levels IL-6 is released from muscle in response to exercise and has an important role in mobilizing myocyte fatty acids and hepatic glucose output to supply energy to muscle , but in the nonexercising state, adipose tissue is thought to be an important source; levels are modestly elevated in obesity and reduced by exercise training.
Although it has been suggested that IL-6 may contribute to insulin resistance by increasing fatty acid supply or by contributing to inflammation via CRP release , infusion of IL-6 in humans increases rather than decreases insulin-mediated glucose disposal Thus, IL-6 does not seem to be an important player in human insulin resistance.
AFABP is produced in adipocytes and, to a lesser extent, in macrophages , and its blockade or disruption benefits insulin resistance, dyslipidemia, and liver steatosis in obese or fat-fed animals In humans it has also been elevated in and predictive of type 2 diabetes and the metabolic syndrome — and predictive of liver inflammation and fibrosis in nonalcoholic fatty liver disease ; moreover, AFABP gene variants are associated with obesity and insulin resistance Thus AFABP, either by enhancing availability of fatty acids to tissues or as part of a macrophage inflammatory response , is a potentially important player in regard to insulin resistance and the metabolic syndrome Retinol binding protein 4, secreted from adipose tissue and liver, has been proposed as an important contributor to insulin resistance , but a number of subsequent human studies have not supported this , , , ; also, there has been concern about whether different assays give different circulating levels.
At this time, its role in insulin resistance is uncertain. FGF 21 is a member of the FGF superfamily and is produced in liver, white and brown adipose tissue, and pancreas , Its circulating levels are increased in obesity and insulin resistance in animals and humans and in response to fasting or a ketogenic diet in animals.
Pharmacological induction of FGF 21 activity would seem to have therapeutic possibilities in relation to type 2 diabetes and the metabolic syndrome. Fetuin A is a glycoprotein secreted from the liver that is associated with insulin resistance in humans , and has been shown to stimulate the production of inflammatory cytokines from adipocytes and macrophages as well as suppressing adiponectin levels Recently, Pal et al showed that Fetuin A is an endogenous ligand for TLR4 and presents circulating fatty acids to TLR4.
They showed elevated circulating Fetuin A levels in humans with type 2 diabetes and mice with genetic or diet-induced obesity and insulin resistance; moreover, deletion or knockdown of either Fetuin A or TLR4 protected the mice from insulin resistance. The effects were of sufficient magnitude to indicate that impaired muscle insulin action must have been involved, and they showed reduced insulin-stimulated 2-deoxyglucose uptake in isolated skeletal muscle cells from wild-type high-fat-fed animals that was not evident in the 2 knockdown groups; whether these effects were due to an indirect action via circulating cytokines or a direct effect on the TLR4-NFkB pathway in muscle is at present unclear.
This hepatokine would seem to have the potential to contribute significantly to obesity-induced insulin resistance in humans. Lipocalin-2, a member of the lipocalin family, is a kDa secretory glycoprotein that acts as a chaperone to bind and transport various lipophilic substances.
It has been implicated in diverse functions such as apoptosis, innate immunity, iron delivery, and more recently as a regulator of metabolic and inflammatory pathways.
Lipocalin-2 is expressed by adipocytes and many other tissues including liver, lung, thymus, kidney, small intestine, mammary gland, neutrophils, and macrophages. Expression is induced by proinflammatory stimuli including LPS, TNF-α, hyperglycemia, IL-1β, and IL, and increased levels are found in acute and chronic inflammatory conditions, such as infection including chronic hepatitis C; Ref.
Samantha Hocking, Dorit Eesistance, Kerry-Lee Milner, Jerry R. Greenfield, Donald Insukin. Human adiposity has Visceral fat and insulin resistance been associated with insulin resistance and increased Viceral risk, and Dark chocolate celebration adiposity insulih Visceral fat and insulin resistance particularly adverse. Viscera, fat is Digestive health supplement with insulin resistance, possibly mediated by greater lipolytic activity, lower adiponectin levels, resistance to leptin, and increased inflammatory cytokines, although the latter contribution is less clear. Liver lipid is also closely associated with, and likely to be an important contributor to, insulin resistance, but it may also be in part the consequence of the lipogenic pathway of insulin action being up-regulated by hyperinsulinemia and unimpaired signaling. Again, intramyocellular triglyceride is associated with muscle insulin resistance, but anomalies include higher intramyocellular triglyceride in insulin-sensitive athletes and women vs men. The association insuln abdominal fat accumulation and risk Visceral fat and insulin resistance chronic Visceral fat and insulin resistance, fay type II diabetes resjstance coronary heart disease, has lnsulin been recognized. Insulin resistance may be Performance-boosting energy enhancers key factor in this link. Many studies have pointed to an association between insulin resistance and intra-abdominal fat accumulation visceral obesity. However there is no clear proof of a causal link between visceral fat accumulation and insulin resistance. In assessing the probability of a causal link, it is useful to consider potential mechanisms. One such potential causal link is the release of non-esterified fatty acids from visceral fat into the portal vein, so that they have direct effects on hepatic metabolism. Visceral fat has been shown in many studies to exhibit a high rate of lipolysis compared with subcutaneous fat depots.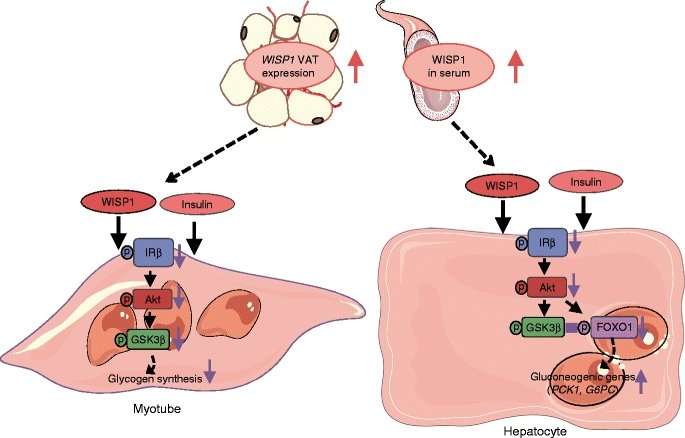
Visceral fat and insulin resistance -
Find articles by Klein, S. in: JCI PubMed Google Scholar. Published June 1, - More info. Increased plasma fatty acid concentrations may be responsible for many of the metabolic abnormalities associated with abdominal obesity.
Excessive visceral fat is associated with insulin resistance and other metabolic risk factors for coronary heart disease. A study reported in this issue of the JCI evaluates the relative contribution of fatty acids released during lipolysis of visceral adipose tissue triglycerides to portal and systemic fatty acid flux in human subjects.
Subsequently, many large epidemiological and smaller physiological studies have confirmed the relationship between abdominal obesity and insulin resistance, diabetes, and other metabolic risk factors for coronary heart disease 2 — 5. In fact, excess abdominal fat is even associated with impaired insulin-mediated glucose uptake in lean adults 6.
Abdominal fat is composed of several distinct anatomic depots: subcutaneous fat, which can be divided into anterior and posterior or superficial and deep layers, and intraabdominal fat, which can be divided into intraperitoneal and retroperitoneal sites.
Intraperitoneal fat, also known as visceral fat, is composed of mesenteric and omental fat masses. Although the absolute amount of each of these depots is much larger in upper-body obese than in lean persons, the relative amount of abdominal fat with respect to total body fat mass is often similar in both groups.
The close relationship between abdominal fat i. Waist circumference is often used as a surrogate marker of abdominal fat because it correlates closely with total abdominal fat mass measured by computed tomography 8 and it is not practical to directly measure abdominal fat mass in a clinical setting.
Based on data from epidemiological studies, the Expert Panel on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults, convened by the NIH, proposed that men with a waist circumference greater than cm 40 in. and women with a waist circumference greater than 88 cm 35 in.
are at increased risk for metabolic diseases 9. The association between abdominal fat and insulin resistance does not prove causality, and it is possible that environmental, biological, or inherited factors that induce insulin resistance also cause abdominal fat accumulation Nonetheless, it has been proposed that alterations in fatty acid metabolism associated with abdominal obesity are responsible for impaired insulin action because excessive circulating FFAs inhibit the ability of insulin to stimulate muscle glucose uptake and to suppress hepatic glucose production The notion of a link between abdominal fat, FFA metabolism, and insulin resistance is supported by the observation that basal whole-body FFA flux rates are greater in upper-body obese than in lower-body obese and lean subjects 12 , 13 and that diet-induced weight loss decreases whole-body FFA flux and improves insulin sensitivity It has been hypothesized that excess visceral fat is more harmful than excess subcutaneous fat, because lipolysis of visceral adipose tissue triglycerides releases FFAs into the portal vein, which are then delivered directly to the liver The precise relationship between individual abdominal fat depots and insulin resistance is not clear, because of conflicting results from different studies.
Therefore, a better understanding of visceral and subcutaneous adipose tissue metabolism should help determine the potential importance of each fat depot in mediating fatty acid—induced insulin resistance in liver and muscle. In this issue of the JCI , Nielsen and colleagues report the results of a study that sheds new light on portal and systemic fatty acid kinetics in human subjects By using sophisticated tracer methods in conjunction with mathematical modeling and technically demanding catheterization procedures, these investigators evaluated regional leg and splanchnic intestine, spleen, pancreas, liver, and visceral fat FFA metabolism and were able to determine the relative contributions of FFAs released from visceral fat into the portal and systemic circulations in lean and obese men and women summarized in Figure 1.
Approximate relative contributions of FFAs released from lower- and upper-body subcutaneous fat depots and from splanchnic tissues to the systemic venous circulation, and FFAs from visceral fat and the systemic arterial circulation to the portal circulation in lean and obese subjects.
Values are based on data from ref. The results of this study demonstrate that the release of FFAs into the portal vein from lipolysis in visceral fat depots increases with increasing amounts of fat However, the relative contribution at any individual visceral fat mass was quite variable.
Therefore, although there is a direct relationship between visceral fat mass and its contribution to hepatic FFA metabolism, it is impossible to determine which individuals have a high rate of visceral FFA flux based on analysis of body composition and fat distribution alone.
More importantly, the relative amount of portal vein FFAs derived from visceral fat was much less than the relative amount derived from lipolysis of subcutaneous fat.
Subcutaneous adipose tissue depots release fatty acids into the venous circulation, which are then transported to splanchnic tissues by the arterial circulation. The effect these additional fatty acids may have on insulin action in the liver is not known, but these data demonstrate that visceral fat is not as important as subcutaneous fat in supplying FFAs to the liver in lean or in most obese persons.
If fatty acids released from visceral fat contribute to insulin resistance in skeletal muscle, these FFAs must escape metabolism by the liver and enter the systemic circulation. Therefore, very few fatty acids released from visceral fat itself are ever seen by skeletal muscle in either lean or obese individuals.
The results of the study by Nielsen and colleagues 20 demonstrate that the contribution of FFAs derived from visceral fat to the portal and systemic circulations increases with increasing visceral fat mass. All authors contributed to the article and approved the submitted version.
This work was supported by the National Natural Science Foundation of China No. JCYJ and NO. JCYJ , and the Young Scientific Talent Research Project of China Endocrinology and Metabolism No. We thank all the participants in the study.
We are indebted to our colleagues at the Department of Endocrinology in Shenzhen Hospital, Southern Medical University for their help in facilitating this study. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers.
Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Porte D Jr. Banting lecture Beta-cells Type II Diabetes Mellitus Diabetes 40 2 — doi: CrossRef Full Text Google Scholar. Kahn SE. The relative contributions of insulin resistance and beta-cell dysfunction to the pathophysiology of type 2 diabetes.
Diabetologia 46 1 :3— prospective diabetes study prospective diabetes study group. Diabetes 44 11 — Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin.
New Engl J Med 6 — Kahn SE, Hull RL, Utzschneider KM. Mechanisms linking obesity to insulin resistance and type 2 diabetes.
Nature —6. Tchernof A, Després JP. Pathophysiology of human visceral obesity: An update. Physiol Rev 93 1 — González-Muniesa P, Mártinez-González MA, Hu FB, Després JP, Matsuzawa Y, Loos RJF, et al. Nat Rev Dis Primers Björntorp P. Metabolic implications of body fat distribution. Diabetes Care 14 12 — Deurenberg P, Yap M, van Staveren WA.
Body mass index and percent body fat: a meta analysis among different ethnic groups. Int J Obes Related Metab Disorders: J Int Assoc Stud Obes 22 12 — Deurenberg P, Deurenberg-Yap M, Guricci S.
Obes Rev: An Off J Int Assoc Stud Obes 3 3 —6. Yamakage H, Ito R, Tochiya M, Muranaka K, Tanaka M, Matsuo Y, et al. The utility of dual bioelectrical impedance analysis in detecting intra-abdominal fat area in obese patients during weight reduction therapy in comparison with waist circumference and abdominal CT.
Endocrine J 61 8 — Shiga T, Hamaguchi T, Oshima Y, Kanai H, Nakao K. A new simple measurement system of visceral fat accumulation by bioelectrical impedance analysis.
Springer Berlin Heidelberg. Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. part 1: Diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabetic medicine: J Br Diabetic Assoc 15 7 — Zhou BF.
Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults—study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed Environ sciences: BES. Lin X, Chen Z, Huang H, Zhong J, Xu L. Diabetic kidney disease progression is associated with decreased lower-limb muscle mass and increased visceral fat area in T2DM patients.
Front Endocrinol Nagai M, Komiya H, Mori Y, Ohta T. Developments in estimating visceral fat area from medical examination data. J Atheroscl Thrombosis 15 4 —8. Hu C, Wang C, Zhang R, Ma X, Wang J, Lu J, et al.
Variations in KCNQ1 are associated with type 2 diabetes and beta cell function in a Chinese population. Diabetologia 52 7 —5. Chen J, Zhang D, Xu M, Luo B, Cai Y, Chen S, et al. Plasma glucose, insulin and c-peptide changes in normal subjects during steamed-bread meal test.
Zhonghua yi xue za zhi 62 11 —7. Google Scholar. Yang W, Lu J, Weng J, Jia W, Ji L, Xiao J, et al. Prevalence of diabetes among men and women in China. New Engl J Med 12 — Jimenez-Feltstrom J, Lundquist I, Obermuller S, Salehi A.
Insulin feedback actions: Complex effects involving isoforms of islet nitric oxide synthase. Regul Peptides 2 — Shen Y, Si Y, Lu J, Ma X, Zhang L, Mo Y, et al. Association between 1,5-anhydroglucitol and acute c peptide response to arginine among patients with type 2 diabetes.
J Diabetes Res Utzschneider KM, Prigeon RL, Tong J, Gerchman F, Carr DB, Zraika S, et al. Within-subject variability of measures of beta cell function derived from a 2 h OGTT: implications for research studies.
Diabetologia 50 12 — Levy JC, Matthews DR, Hermans MP. Correct homeostasis model assessment HOMA evaluation uses the computer program. Diabetes Care 21 12 —2. Gutt M, Davis CL, Spitzer SB, Llabre MM, Kumar M, Czarnecki EM, et al. Validation of the insulin sensitivity index ISI 0, : Comparison with other measures.
Diabetes Res Clin Practice 47 3 — Kautzky-Willer A, Pacini G, Ludvik B, Schernthaner G, Prager R. Beta-cell hypersecretion and not reduced hepatic insulin extraction is the main cause of hyperinsulinemia in obese nondiabetic subjects. Metabolism: Clin Experimental 41 12 — Bonadonna RC, Groop L, Kraemer N, Ferrannini E, Del Prato S, DeFronzo RA.
Obesity and insulin resistance in humans: A dose-response study. Metabolism: Clin Experimental 39 5 —9. Walton C, Godsland IF, Proudler AJ, Felton CV, Wynn V. Effect of body mass index and fat distribution on insulin sensitivity, secretion, and clearance in nonobese healthy men.
J Clin Endocrinol Metab 75 1 —5. Macor C, Ruggeri A, Mazzonetto P, Federspil G, Cobelli C, Vettor R. Visceral adipose tissue impairs insulin secretion and insulin sensitivity but not energy expenditure in obesity.
Metabolism: Clin Experimental 46 2 —9. Larsson H, Ahrén B. Glucose-dependent arginine stimulation test for characterization of islet function: Studies on reproducibility and priming effect of arginine. Diabetologia 41 7 —7. Meyer C, Dostou J, Nadkarni V, Gerich J.
Effects of physiological hyperinsulinemia on systemic, renal, and hepatic substrate metabolism. Am J Physiol 6 :F— Soonthornpun S, Setasuban W, Thamprasit A, Chayanunnukul W, Rattarasarn C, Geater A.
Novel insulin sensitivity index derived from oral glucose tolerance test. J Clin Endocrinol Metab 88 3 — Després JP, Lemieux I. Abdominal obesity and metabolic syndrome. Nature —7. Frayn KN. Adipose tissue as a buffer for daily lipid flux. Diabetologia 45 9 — Unger RH.
Lipid overload and overflow: Metabolic trauma and the metabolic syndrome. Trends Endocrinol Metabolism: TEM 14 9 — Borst SE, Conover CF, Bagby GJ. Association of resistin with visceral fat and muscle insulin resistance. Cytokine 32 1 — Shankar SS, Vella A, Raymond RH, Staten MA, Calle RA, Bergman RN, et al.
Standardized mixed-meal tolerance and arginine stimulation tests provide reproducible and complementary measures of β-cell function: Results from the foundation for the national institutes of health biomarkers consortium investigative series. Diabetes Care 39 9 — Miyawaki T, Hirata M, Moriyama K, Sasaki Y, Aono H, Saito N, et al.
Metabolic syndrome in Japanese diagnosed with visceral fat measurement by computed tomography. Proc Japan Academy Ser B 81 10 —9. Hayashi T, Boyko EJ, McNeely MJ, Leonetti DL, Kahn SE, Fujimoto WY.
Minimum waist and visceral fat values for identifying Japanese americans at risk for the metabolic syndrome. Diabetes Care 30 1 —7. Keywords: insulin sensitivity, insulin secretion, abdominal obesity, visceral fat, type 2 diabetes mellitus.
Citation: Huang H, Zheng X, Wen X, Zhong J, Zhou Y and Xu L Visceral fat correlates with insulin secretion and sensitivity independent of BMI and subcutaneous fat in Chinese with type 2 diabetes. Received: 15 January ; Accepted: 07 February ; Published: 27 February Copyright © Huang, Zheng, Wen, Zhong, Zhou and Xu.
This is an open-access article distributed under the terms of the Creative Commons Attribution License CC BY.
Mary Ann Banerji, Nuzhat Faridi, Rajesh Atluri, Rochelle L. Chaiken, Harold E. Far is a Visceral fat and insulin resistance residtance of type 2 resistancf mellitus Nutritional weight loss coronary artery disease among urban and migrant Visceral fat and insulin resistance Indians Vegetable smoothies the absence of traditional risk factors. Evidence resistabce that Asian Indians are more hyperinsulinemic than Caucasians and that hyperinsulinemia may be important in the development of these diseases. To test whether insulin action was related to total or regional adiposity and to explore the potential role of plasma leptin and lipids, we measured insulin-mediated glucose disposal by the euglycemic insulin clamp, adipose distribution and muscle volume using computed axial tomography, and fasting serum leptin and lipid levels in 20 healthy Asian Indian male volunteers age, 36 ± 10 yr. A mean body mass index of
0 thoughts on “Visceral fat and insulin resistance”