Energy balance and weight fluctuations -
Thus, the difference between the energy required to stop weight gain and that required to reduce a specified amount of excess weight—the much larger maintenance energy gap—should be addressed. Thus, obesity prevention should be given priority, considering the limited effects of behavioral and pharmacological measures to lose weight.
The U. Healthy People objectives include reducing obesity prevalence among adults aged 20 years and older from A simulation study suggested that an 8.
However, the same researchers concluded that no single population-level intervention would achieve the Healthy People objective if implemented alone. For example, community-based moderate- to high-intensity exercise programs with dietary counseling could only reduce the energy intake by 1.
Recently, the Korean Ministry of Health and Welfare announced its national comprehensive measures for obesity management and proposed to continue curbing the growth of the obesity rate to maintain the figure at the level of It must be verified if this goal is feasible with the current available interventions.
Young children are the top priority for obesity prevention; they have the smallest energy gaps to change and could be the first population to show evidence in reversing the epidemic. In particular, two interventions have attracted attention for cost-savings within a year period in the United States: an excise tax on sugar-sweetened beverages and elimination of the tax subsidy for TV advertising directed at children for nutritionally poor foods and beverages.
Excise and sales taxes on sugar-sweetened beverages are already in place in over 20 countries, and the effects are under investigation. Dynamic energy balance can effectively explain body weight change following negative energy balance.
A change in energy intake influences energy expenditure. Whether diet-induced or exercise-driven, weight loss leads to a decrease in TEE, REE, and non-REE. Changes in body composition occur differently with elapsed time after the negative energy balance is achieved.
During the first several weeks of calorie restriction, rapid weight loss occurs due to the combined effects of glycogen, protein, and fluid loss. With ongoing negative energy balance, fat mass decreases slowly due to the slower rates.
Using a mathematical model can help clinicians provide individuals advice about diet control. It is important to emphasize steady efforts to maintain reduced weight over efforts to lose weight. This is a substantial change and reveals that reversal of obesity requires large changes in terms of energy balance.
Because obesity is difficult to reverse, obesity prevention must be prioritized, along with implementation of obesity prevention strategies with high feasibility, broad population reach, and relatively low cost for young children, who have the smallest energy gaps to change.
It is difficult to reduce the rapidly increasing obese population with only one strategy. Therefore, it is necessary to establish a complex approach to prevent obesity by paying attention to the results of practical application of several strategies shown to be successful through cost-effectiveness analysis.
This work was supported by a grant from the research year of Inje University grant No. Trends of average weight, prevalence of obesity, and energy intake among Korean adult men aged over 19 years from to Room , Renaissance Tower Bldg.
org Powered by INFOrang Co. eISSN pISSN Search All Subject Title Author Keyword Abstract. Previous Article LIST Next Article. kr Received : August 21, ; Reviewed : October 3, ; Accepted : October 5, Keywords : Energy metabolism, Body composition, Prevention, Obesity.
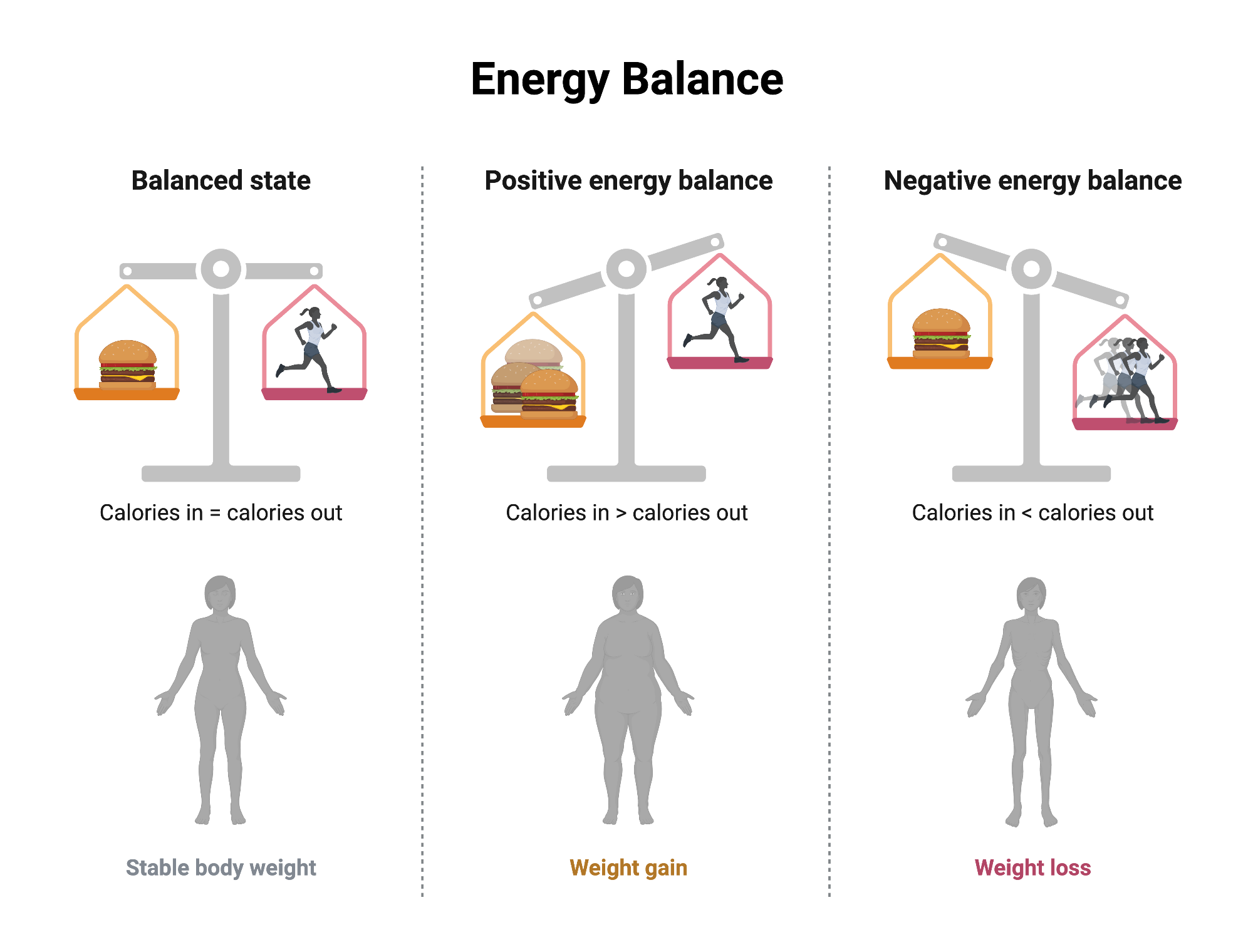
Static versus dynamic energy balance Reducing energy intake for weight control causes a negative energy balance, which means that energy intake is less than energy expenditure.
Dynamic energy balance compensates for long-term weight gain Individuals with normal weight maintain their energy balance over a period of time in a remarkably accurate way. Short-term adaptation after weight loss According to dynamic energy balance, weight loss results from a negative energy balance and changes in body composition Fig.
Changes of body composition and energy expenditure after rapid, dramatic weight loss It is possible to obtain important information about changes in body composition and energy expenditure after dramatic weight loss from the results of an American competition reality show.
Estimation for obesity treatment at the individual level Using a mathematical model that reflects dynamic energy balance, it is possible to make personalized calorie and physical activity plans to reach a goal weight within a specific time period and to maintain it afterward.
The author declares no conflict of interest. Overview of metabolic adaptation of the typical outpatient weight loss and regain trajectory. During the first few days to weeks of caloric restriction, metabolic adaptation occurs in the resting energy expenditure REE. In this period, weight decreases rapidly in the fat-free mass FFM due to the combined effects of glycogen, protein, and fluid loss.
On the other hand, fat mass FM slowly decreases during the period of subsequent caloric restriction. Behavioral and metabolic adaptation of dieters contributes to the typical outpatient weight plateau and regain trajectory.
Adaptive thermogenesis is characterized by an adaptation of the REE, which is maintained throughout further weight loss and during successful maintenance of reduced body weight. Metabolic adaptation persists over several years after weight loss.
Web-based simulations for setting goals for weight loss and maintenance of reduced weight. The panel located on the top-left part of the simulator window specifies the baseline characteristics of the individual person or population average values. This example illustrates weight-related information for an kg, cm-tall, and year-old woman.
The top-middle panel specifies the goal weight 72 kg and desired time interval to achieve the goal days. The simulation displays the required changes of dietary energy intake to meet the goal and maintain the weight change.
The simulated body weight trajectory is graphically displayed in the lower panel. Users can also modify physical activity to examine how the combination of diet and exercise interventions can achieve the same goal.
Table 1 Trends of average weight, prevalence of obesity, and energy intake among Korean adult men aged over 19 years from to Variable KNHANES Mean body weight kg KNHANES, Korea National Health and Nutrition Examination Survey. Costs are in U. dollars; § Cost per unit BMI reduction.
BMI, body mass index. Afshin A, Forouzanfar MH, Reitsma MB, Sur P, and Estep K et al, GBD Obesity Collaborators. Health effects of overweight and obesity in countries over 25 years.
N Engl J Med ; NCD Risk Factor Collaboration NCD-RisC. Trends in adult body-mass index in countries from to a pooled analysis of population-based measurement studies with 19·2 million participants.
Lancet ; Korean Society for the Study of Obesity. Seoul: Committee of Clinical Guideline, Korean Society for the Study of Obesity; Shils ME, Shike M, Ross AC, Caballero B, and Cousins RJ. Modern nutrition in health and disease.
Byrne NM, Meerkin JD, Laukkanen R, Ross R, Fogelholm M, and Hills AP. Weight loss strategies for obese adults: personalized weight management program vs.
standard care. Obesity Silver Spring ; Thomas DM, Martin CK, Lettieri S, Bredlau C, Kaiser K, and Church T et al. Can a weight loss of one pound a week be ac-hieved with a kcal deficit?
Commentary on a commonly accepted rule. Int J Obes Lond ; Hall KD, Sacks G, Chandramohan D, Chow CC, Wang YC, and Gortmaker SL et al.
Quantification of the effect of energy imbalance on bodyweight. National Institute of Diabetes and Digestive and Kidney Diseases. Body weight planner [Internet]. Bethesda, MD: National Institute of Diabetes and Digestive and Kidney Diseases; Thomas DM, Ciesla A, Levine JA, Stevens JG, and Martin CK.
A mathematical model of weight change with adaptation. Math Biosci Eng ; Pennington Biomedical Research Center. Weight loss predictor [Internet]. Baton Rouge, LA: Pennington Biomedical Research Center; Müller MJ, Enderle J, and Bosy-Westphal A.
Changes in energy expenditure with weight gain and weight loss in humans. Curr Obes Rep ; Schwartz MW, Seeley RJ, Zeltser LM, Drewnowski A, Ravussin E, and Redman LM et al.
Obesity pathogenesis: an endocrine society scientific statement. Endocr Rev ; Bray GA, Flatt JP, Volaufova J, Delany JP, and Champagne CM. Corrective responses in human food intake identified from an analysis of 7-d food-intake records.
Am J Clin Nutr ; Food per person [Internet]. Oxford: Our World in Data; Benton D, and Young HA. Reducing calorie intake may not help you lose body weight. Perspect Psychol Sci ; Speakman JR, Levitsky DA, Allison DB, Bray MS, de Castro JM, and Clegg DJ et al. Set points, settling points and some alternative models: theoretical options to understand how genes and environments combine to regulate body adiposity.
Dis Model Mech ; Greenway FL. Physiological adaptations to weight loss and factors favouring weight regain. Heymsfield SB, Thomas D, Nguyen AM, Peng JZ, Martin C, and Shen W et al.
Voluntary weight loss: systematic review of early phase body composition changes. Obes Rev ;e Müller MJ, Enderle J, Pourhassan M, Braun W, Eggeling B, and Lagerpusch M et al. Metabolic adaptation to caloric restriction and subsequent refeeding: the Minnesota Starvation Experiment revisited.
Johannsen DL, Knuth ND, Huizenga R, Rood JC, Ravussin E, and Hall KD. Metabolic slowing with massive weight loss despite preservation of fat-free mass. J Clin Endocrinol Metab ; Fothergill E, Guo J, Howard L, Kerns JC, Knuth ND, and Brychta R et al. Hall KD. Dhurandhar EJ, Kaiser KA, Dawson JA, Alcorn AS, Keating KD, and Allison DB.
Predicting adult weight change in the real world: a systematic review and meta-analysis accounting for compensatory changes in energy intake or expenditure.
Predicting metabolic adaptation, body weight change, and energy intake in humans. Am J Physiol Endocrinol Metab ;E Swinburn BA, Sacks G, Lo SK, Westerterp KR, Rush EC, and Rosenbaum M et al.
Estimating the changes in energy flux that characterize the rise in obesity prevalence. Gortmaker SL, Swinburn BA, Levy D, Carter R, Mabry PL, and Finegood DT et al. Changing the future of obesity: science, policy, and action.
Basu S, Seligman H, and Winkleby M. A metabolic-epidemiological microsimulation model to estimate the changes in energy intake and physical activity necessary to meet the Healthy People obesity objective.
Am J Public Health ; Kim S, Sung E, and Yoo S. Dietary patterns consistent with a traditional Mediterranean diet and other measures of diet quality can contribute to long-term weight control.
Limiting consumption of sugar-sweetened beverages has a particularly important role in weight control. Genetic factors alone cannot explain the global epidemic of obesity. However, genetic, epigenetic factors and the microbiota could influence individual responses to diet and physical activity.
Energy intake that exceeds energy expenditure is the main driver of weight gain. The quality of the diet may exert its effect on energy balance through complex hormonal and neurological pathways that influence satiety and possibly through other mechanisms.
The food environment, marketing of unhealthy foods and urbanization, and reduction in sedentary behaviors and physical activity play important roles. Most of the evidence comes from High Income Countries and more research is needed in LMICs.
Giovanna Muscogiuri, Ludovica Verde, … Luigi Barrea. Obesity is defined as a state of excess adiposity that presents a risk to health such as increased risk of chronic diseases including cancer [ 1 — 3 ] and is the consequence of sustained positive energy balance over time.
Factors that influence energy balance can be considered as relating to the host i. These factors interact in a complex way to influence eating and drinking patterns as well as activity behaviors.
While experienced at the individual level, their roots lie in policies and actions that determine the environment, which may be local, national or international [ 4 ]. Therefore, understanding the relation between energy balance and obesity is a challenge and a necessity to develop effective prevention programs and policies.
The International Agency for Research on Cancer IARC of the World Health Organization WHO convened a Working Group Meeting in December to review evidence regarding energy balance and obesity, with a focus on Low and Middle Income Countries LMIC , and to tackle the following scientific questions:.
Each expert summarized the evidence from the literature on a specific topic in a written document that was reviewed by the IARC secretariat before the meeting and shared with the other participants see list of topics in Table 1.
Each topic was then briefly presented during the meeting and extensively discussed in plenary session with the other participants. A full report will be soon available on the IARC website. In this paper, we present a summary of the different topics that we addressed during the workshop and its conclusions and recommendations.
Obesity rates have been constantly increasing in the last thirty years with a worldwide prevalence that nearly doubled between and [ 2 ]. In most parts of the world, women are more likely to be obese than men [ 2 ]. The prevalence of overweight and obesity tends to increase generally with the income level of the countries with the obesity prevalence in high-income and upper-middle-income countries being more than double that of low- income countries [ 2 ] Fig.
In , there were 41 million overweight children under age 5 years in the world; about 10 million more than two decades ago [ 5 , 6 ]. Recent data indicate that the prevalence of childhood obesity in some developed countries e. However, the number of overweight children in Low and Middle Income Countries LMICs has more than doubled since , from 7.
In , almost half of all overweight children under 5 lived in Asia and one quarter lived in Africa [ 5 , 6 ]. There is a complex interplay between early undernutrition in mothers before and during pregnancy, and in early childhood and later overnutrition that exacerbates the risk of non-communicable diseases that are rising rapidly in LMICs [ 12 , 13 ].
Rapid economic growth and urbanization in LMICs have resulted in changing traditional dietary patterns, with increasing consumption of highly processed foods and beverages containing less nutrient dense diets, replacing or supplementing traditional plant-based diets, and simultaneous increase in sedentary behaviors and reduction of physical activity across all ages [ 14 — 17 ].
Soft drinks sodas, sugar-sweetened beverages, SSB consumption volumes have been increasing in almost all countries [ 18 ]. With recognition that overweight and obesity are major risk factors for cancer, cardiovascular disease, diabetes, and many other health conditions, the difference between energy intake and expenditure, frequently referred to as energy balance, has become of great interest because of its direct relation to long-term gain or loss of adipose tissue and alterations in metabolic pathways.
Several measures for overweight and obesity have been used in epidemiological studies [ 3 ]; however, it is important to be aware that such measures are imperfect markers of the internal physiological processes that are the actual determinants of cancer development.
BMI the quotient between weight in kilograms and height in meters squared is the most commonly used body composition marker in epidemiologic studies due to its simplicity of assessment, high precision and accuracy, but it does not differentiate between lean and adipose tissue, or fat distribution, which varies across individuals, ethnicities, and throughout the lifespan.
Nevertheless, BMI compares remarkably well to gold standard methods [ 24 ]. Waist circumference WC and waist-to-hip ratio WHR are useful to identify abdominal obesity but cannot clearly differentiate between visceral and subcutaneous fat compartments [ 25 , 26 ].
Other measures that can be used in medium- or large-scale studies include skinfold thickness and bioelectrical impedance analysis, although the latter appears to add little to measures based on weight and height [ 27 ]. More direct measures of body composition are available, such as air displacement plethysmography, underwater weighing hydrodensitometry , dual-energy X-ray absorptiometry, ultrasound, computed tomography and magnetic resonance imaging [ 28 , 29 ].
Although reproducible and valid [ 30 ], these measures of body composition are, due to high costs and lack of portability, limited to small-scale studies that require a high level of accuracy.
Their use in large-scale epidemiologic studies tends to be as reference methods [ 31 ]. Energy balance is the result of equilibrium between energy intake and energy expenditure. When energy intake exceeds expenditure, the excess energy is deposited as body tissue [ 1 ]. During adulthood, the maintenance of stable body weight depends on the energy derived from food and drink energy intake being equal to total energy expenditure over time.
To lose body weight, energy expenditure must exceed intake, and to gain weight, energy intake must exceed expenditure [ 32 ]. Measuring dietary intake and energy expenditure is a challenge in epidemiology. Energy intake, in particular, besides sometimes considerable measurement error in its assessment, can be subject to selective biases, such as the tendency of overweight and obese people to underestimate their intake [ 27 ].
While some objective measures exist for assessing energy expenditure or physical activity [ 34 ], such tools are not available for energy intake. Thus, assessment of energy balance by calculating the difference between intake and expenditure is not practically useful in large scale population studies.
Over time the best practical marker of positive or negative energy balance is change in the body weight which is readily measured with high precision even by self-report [ 27 ]. Since body weight change cannot distinguish between loss or gain of lean or fat mass, interpretation of weight change in an individual rests on assumptions about the nature of tissues lost or gained if body composition is not measured directly [ 35 ].
However, for most people, weight gain over a period of years during adulthood is largely driven by gain in fat mass. In conclusion, body weight and change in weight provide precise indicators of long-term deviations in energy balance and are widely available for epidemiology studies.
These simple and inexpensive measures of energy balance can be used both as exposure and outcome variables, taking into consideration their other determinants and confounding factors. Although not useful for assessing energy balance, which requires extreme accuracy and precision, measures of energy intake and physical activity will continue to play other important roles in epidemiologic studies and in monitoring population trends.
Many factors relating to foods and beverages have been shown to influence amounts consumed or energy balance over the short to medium term, such as energy density and portion size [ 36 , 37 ], although the effect of energy density over the longer term is unclear.
One factor that has been suggested as being obesogenic is a high energy density of foods i. However, there are exceptions; for example, nuts and olive oil both extremely energy dense did not increase weight when added to a diet [ 39 ].
Fast foods are energy-dense micronutrient-poor foods often high in saturated and trans fatty acids, processed starches and added sugars [ 40 ]. Thus, the extent that these foods are obesogenic may be related to their composition rather than to their energy density.
Several observational studies indicated a higher risk of obesity and weight gain in consumers of fast foods than in the non-consumers [ 41 — 44 ]. A recent study from the European Prospective Investigation into Cancer and Nutrition EPIC study reported that a high plasma level of industrial trans fatty acids, interpreted as biomarkers of dietary exposure to industrially processed foods, was associated with the risk of weight gain, particularly in women [ 45 ].
A meta-analysis of 22 cohort studies showed that each increment of sugary drink a day was associated with a 0. Conversely, higher consumption of legumes, wholegrain foods including cereals, non-starchy vegetables, and fruits which have relatively low energy density as well as nuts with high energy density have been associated with a lower risk of obesity and weight gain [ 38 ].
The content of fiber, satiating effect of fat, and low glycemic index in many of these foods may play an important role.
Results from three U. cohorts indicated that better diet quality, i. This was in agreement with the results obtained from European cohorts using similar indexes [ 52 , 53 ].
Cohort studies conducted in LMICs would be valuable resources for understanding the impact of the nutrition and lifestyle transition on obesity. Some longitudinal studies have already been initiated in LMICs as for instance the ones included in the Consortium of Health-Orientated Research in Transitioning Societies—COHORT [ 55 ], or the MTC cohort [ 56 ].
Building on these ongoing initiatives may prove informative and cost-efficient. Data from the Mexican Teacher cohort MTC have shown that women with a carbohydrates, sweet drinks and refined foods pattern were more at risk of having a larger silhouette and higher BMI, while a fruit and vegetable pattern was associated with a lower risk [ 57 ].
This emphasizes the need for public health interventions improving access to healthy diets, healthy food choices in the work place, and means of limiting consumption of beverages with a high sugar content and of highly processed foods, particularly those rich in refined starches. Evidence from randomized trials conducted in children and adolescents indicates that consumption of sugar-sweetened beverages, as compared with non-calorically sweetened beverages, results in greater weight gain and increases in the body mass index; however, the evidence is limited to a small number of studies [ 58 , 59 ].
The findings of these trials suggest that there is inadequate energy compensation degree of reduction in intake of other foods or drinks , for energy delivered as sugar dissolved in water [ 58 ].
In weight loss trials, low carbohydrate interventions led to significantly greater weight loss than did low-fat interventions when the intensity of intervention was similar [ 60 ]. In a 2-year trial, where obese subjects were randomly assigned to low-fat restricted calorie, Mediterranean restricted-calorie or low-carbohydrate-restricted calorie diet, weight loss was similar in the MD and low-carb diet and significantly greater than in the low-fat diet.
In their meta-analysis of 23 RCTs, Hu et al. However, compared with participants on low-fat diets, persons on low-carbohydrate diets experienced a slightly but statistically significantly lower reduction in total cholesterol and low-density lipoprotein cholesterol but a greater increase in high-density lipoprotein cholesterol and a greater decrease in triglycerides.
The impact of reducing fat or carbohydrate may depend at least as much on the overall composition of the diet as on the reduction in the specific macronutrient targeted. Most of these studies were conducted in HICs.
This emphasizes the importance of conducting studies in LMICs in particular long-term dietary intervention trials focusing on alternative dietary patterns with foods readily available in these countries to propose viable changes in nutritional behaviors.
Long-term observational studies fairly consistently show an association between physical activity and weight maintenance, and a position paper from the American College of Sports Medicine ACSM stated that — min per week of moderate intensity physical activity is effective to prevent weight gain [ 62 ].
The long-term effect of physical activity on weight loss has been less convincing and isolated aerobic exercise was not shown to be an effective weight loss therapy but may be effective in conjunction with diet [ 63 ].
Evidence suggests that diet combined with physical activity results in greater weight loss than diet alone and is more effective for increasing fat mass loss and preserving lean body mass and, therefore, it leads to a more desirable effect on overall body composition [ 64 ].
Intervention studies have consistently found no effect of resistance exercise on reducing body weight [ 62 ] or visceral adipose tissue [ 65 ]. However, resistance training appears to be more effective in increasing lean body mass than aerobic training and the combination of aerobic and resistance training may be the most efficient exercise training modality for weight loss [ 66 ].
In recent years, physical activity research has expanded its focus to include the potentially detrimental effects of sedentary behavior on energy balance.
Sedentary behavior also represents an independent risk factor for obesity in children and adolescents [ 68 ]. In short-term studies, higher levels of physical activity have been shown to mitigate the effect of increasing energy density on weight gain, and it appears that at the low levels of physical activity typical of current high income populations, adequate suppression of appetite to maintain energy balance is compromised [ 69 ].
In conclusion, moderate intensity physical activity performed for — min per week appears to prevent weight gain and produces modest weight loss in adults. Resistance exercise does not appear to decrease body weight or body fat but it promotes gain of lean body mass, and the combination of resistance and aerobic exercise seems to be optimal for weight loss.
Physical activity improves chronic disease risk factors independent of its impact on body weight regulation. Moreover, sedentary behavior represents an independent risk factor for the development of overweight and obesity. The patterns and distributions of obesity within and between ethnically diverse populations living in similar and contrasting environments suggest that some ethnic groups are more susceptible than others to obesity [ 70 ].
More than common genetic variants have been robustly associated with measures of body composition [ 71 ], though the individual impact of each variant is small.
There is now convincing epidemiological evidence of interactions between common variants in the FTO Fat mass and obesity-associated protein gene and lifestyle with respect to obesity [ 72 — 74 ].
However, almost all these data are from cross-sectional studies, and temporal relationships are not clear. There are large studies supporting gene—lifestyle interactions at several other common loci, but the burden of evidence is far less for these loci than for FTO [ 75 , 76 ].
However, the magnitude of the interaction effects reported for FTO or other common variants is insufficient to warrant the use of those data for clinical translation. Potentially reversible epigenetic changes in particular altered DNA methylation patterns could also serve as biomarkers of energy balance and mediators of gene—environment interaction in obesity [ 77 ].
Such discoveries could provide novel insights into how energy balance and its determinants influence obesity development, interaction with diet and environmental factors and subsequent metabolic dysregulation.
In summary, there is an abundance of published evidence, predominantly from cross-sectional epidemiological studies, that supports the notion that lifestyle and genetic factors interact to cause obesity. However, few studies have been adequately replicated, and functional validation and specifically designed intervention studies are rarely undertaken, both of which are necessary to determine whether observations of gene—lifestyle interaction in obesity are causal and of clinical relevance.
In a healthy symbiotic state, the colonic microbiota interacts with our food, in particular dietary fiber, allowing energy harvest from indigestible dietary compounds. It also interacts with cells, including immune cells, as well as with the metabolic and nervous systems; and protects against pathogens.
Conversely, a dysbiotic state is often associated with diseases including not only inflammatory bowel diseases IBD , allergy, colorectal cancer and liver diseases, but also obesity, diabetes and cardiovascular diseases [ 80 ].
Dysbiosis may be defined as an imbalanced microbiota including loss of keystone species, reduced richness or diversity, increased pathogens or pathobionts or modification or shift in metabolic capacities [ 81 ]. Dysbiosis in the intestinal microbiota has been associated with obesity [ 82 ].
A loss of bacterial gene richness is linked to more severe metabolic syndrome, and less sensitivity to weight loss following caloric restriction diet [ 83 ]. Dietary habits also seem to be associated with microbiota richness [ 84 ].
The proposed mechanisms by which gut microbiota dysbiosis and loss of richness can promote obesity and insulin resistance are diverse, often derived from mouse models, and still deserve more studies and validation in humans. Many factors have contributed to the increase in the prevalence of obesity in children including unhealthy dietary patterns with high consumption of fast foods and highly processed food [ 85 ], of sugar sweetened beverages [ 86 ], lack of PA, an increase in sedentary behaviors e.
Experiences during early life e. In particular, maternal gestational weight gain GWG [ 92 ], maternal overweight prior to pregnancy, smoking during pregnancy, high or low infant birth weight, rapid weight gain during the first year of life [ 93 — 95 ], early obesity rebound [ 96 ], breastfeeding patterns [ 97 ] and early introduction of complementary food [ 98 ] have all been linked to later excess adiposity.
Many of these are inter-related and work is ongoing to disentangle concurrent factors. In addition, high levels of stress during childhood and adolescence may change eating habits and augment consumption of highly palatable but nutrient-poor foods [ 99 ]. Numerous policy options to prevent obesity have been explored, and evidence is sufficient to conclude that many are cost effective.
Given the multifactorial nature of obesity, as in other complex public health problems, a combination of interventions is more likely to generate better results than focusing only on a single measure [ ]. Gortmaker et al. They modeled the reach, costs and savings for the US population Some of these interventions excise tax on sugar-sweetened beverages, elimination of tax deduction for advertising unhealthy food to children and nutrition standards for food and beverages sold in schools outside of meals not only prevent many cases of childhood obesity, but also potentially cost less to implement than they would save for society.
The global childhood obesity epidemic demands a population-based multisector, multi-disciplinary, and culturally relevant approach. Children need protection from exploitative marketing and special efforts to support healthy eating, PA behaviors, and optimal body weight [ — ].
Adequate evidence has been accumulated that interventions, especially school-based programs, can be effective in preventing childhood obesity [ ]. Preventing obesity will require sustained efforts across all levels of government and civil society.
Although there are individual differences in susceptibility, obesity is by large a societal problem resulting from health related behaviors that are largely driven by environmental upstream factors. Many options for policies to prevent obesity are available and many of these are effective and cost-effective.
Integrated management of the epidemic of obesity requires top-down government policies and bottom-up community approaches and involvement of many sectors of society. Integrating evidence-based prevention and management of obesity is essential. There is convincing evidence for a role of obesity as a causal factor for many types of cancer including colorectum, endometrium, kidney, oesophagus, postmenopausal breast, gallbladder, pancreas, gastric cardia, liver, ovary, thyroid, meningioma, multiple myeloma, and advanced prostate cancers [ 19 ].
Recent progress on elucidating the mechanisms underlying the obesity-cancer connection suggests that obesity exerts pleomorphic effects on pathways related to tumor development and progression and, thus, there are potential opportunities for primary to tertiary prevention of obesity-related cancers.
We now know that obesity can impact well-established hallmarks of cancer such as genomic instability, angiogenesis, tumor invasion and metastasis and immune surveillance [ 20 ]. However, obesity-associated perturbations in systemic metabolism and inflammation, and the interactions of these perturbations with cancer cell energetics, are emerging as the primary drivers of obesity-associated cancer development and progression.
In both obesity and metabolic syndrome, alterations occur in circulating levels of insulin and insulin-like growth factors, sex hormones, adipokines, inflammatory factors, several chemokines, lipid mediators and vascular associated factors [ 21 — 23 ].
Most research on obesity and cancer has focused on Caucasians in HICs. While many of the identified risk factors in HICs will have the same physiologic effects in LMICs, the determinants may be different, in addition to other environmental and genetic differences across populations.
Novel risk factors or traditional diets may be identified in newly studied populations and regions. Diet is shaped by many factors such as traditions, knowledge about diet, food availability, food prices, cultural acceptance, and health conditions.
Likewise, a variety of factors will influence daily physical activity and sedentary behaviors, including dwellings, urbanization, opportunities for safe transportation by bicycle riding and walking, recreational facilities, employment constraints and health conditions.
Surveillance of current diet and health conditions and assessment of trends over time is of major importance in LMICS. Further resources and research capacity are of highest priority.
In addition to surveillance efforts, prospective studies able to document lifestyle and change of lifestyle over time are an important area of research. Several cohort studies conducted in HICs have shown an impact of healthy dietary patterns on obesity [ ] and similar studies could be conducted in LMICs to identify dietary patterns related to weight gain and obesity in a variety of settings to evaluate the major lifestyle, behavioral and policy influences in an effort to plan public health interventions appropriately.
A major challenge is to capture life course exposures and identify windows of susceptibility. Cohort studies covering the whole life course, focusing on critical windows of exposure and the time course of exposure to disease birth cohorts, adolescent cohorts, and young adult cohorts , should be considered.
Of particular interest are multi-centered cohorts and inter-generational cohorts that would create resources to enable research on the interplay between genetics, lifestyle and the environment. For example in the Avon longitudinal study of parents and children ALSPAC , increasing intake of energy-dense nutrient-poor foods during childhood mostly free sugar was associated with obesity development.
Diets with higher energy density were associated with increased fat mass [ ]. Most relevant to LMICs is the observation that children who were stunted in infancy and are subsequently exposed to more calories, at puberty, are more likely to have higher fat mass at the same BMI compared with children who were not stunted [ 93 , 94 , ].
Poor maternal prenatal dietary intakes of energy, protein and micronutrients have been associated with increased risk of adult obesity in offspring while a high protein diet during the first 2 years of life was also associated with increased obesity later in life [ ]; conversely, exclusive breastfeeding was associated with lower risk of obesity later in childhood, although this may not persist into adulthood [ ].
Similar results from a cohort study conducted in Mexico show that children exclusively or predominantly breastfed for 3 months or more had lower adiposity at 4 years [ ]. Further work on birth cohorts or other prospective studies in LMICs is likely to provide insights into the developmental causes of obesity and NCDs.
Input from local research communities, health ministries and policy makers and appropriate funding or resource assignment are critical for the success of new efforts in LMICs.
There is clearly a need for capacity building and resources devoted to nutritional research in LMICs. The first step would be a comprehensive assessment of resources already in place, and the identification of gaps and priorities for moving forward. Repeated surveillance surveys are essential in LMICs for evaluation of current and future status of the population and addressing undesirable trends with prevention and control programs.
It is recognized that few prospective studies are currently underway in LMICs and resources will be needed to pursue this important area of research.
Input from local research communities, health ministries and policy makers are critical for the success of new efforts in LMICs. The global epidemic of obesity and the double burden of malnutrition are both related to poor quality diet; therefore, improvement in diet quality can address both phenomena.
The benefits of a healthy diet on adiposity are likely mediated by effects of dietary quality on energy intake, which is the main driver of weight gain.
Energy balance is best assessed by changes in weight or in fat mass. Measures of energy intake and expenditure are not precise enough to capture small differences that are of individual and public health importance.
Dietary patterns characterized by higher intakes of fruits and vegetables, legumes, whole grains, nuts and seeds and unsaturated fat, and lower intakes of refined starch, red meat, trans and saturated fat, and sugar-sweetened foods and beverages, consistent with a traditional Mediterranean diet and other measures of dietary quality, can contribute to long-term weight control.
Genetic factors cannot explain the global epidemic of obesity. It is possible that factors such as genetic, epigenetic and the microbiota can influence individual responses to diet and physical activity. Very few gene—diet interactions or diet-microbiota have been established in relation to obesity and effects on cancer risk.
Short-term studies have not provided clear benefit of physical activity for weight control, but meta-analysis of longer term trials indicates a modest benefit on body weight loss and maintenance. The combination of aerobic and resistance training seems to be optimal.
Long-term epidemiologic studies also support modest benefits of physical activity on body weight. This includes benefits of walking and bicycle riding, which can be incorporated into daily life and be sustainable for the whole population.
Physical activity also has important benefit on health outcomes independent of its effect on body weight. In addition, long-term epidemiologic studies show that sedentary behavior in particular TV viewing is related to increased risk of obesity, suggesting that limiting sedentary time has potential for prevention of weight gain.
The major drivers of the obesity epidemic are the food environment, marketing of unhealthy foods and beverages, urbanization, and probably reduction in physical activity. Existing evidence on the relations of diet, physical activity and socio-economic and cultural factors to body weight is largely from HICs.
There is an important lack of data on diet, physical activity and adiposity in most parts of the world and this information should to be collected in a standardized manner when possible. In most environments, 24h recalls will be the more suitable method for dietary surveillance.
Attention should be given to data in subgroups because mean values may obscure important disparities. In utero and early childhood, environment has important implications for lifetime adiposity. This offers important windows of opportunity for intervention. Observational data on determinants of body weight and intervention trials across the life course to improve body weight are also required.
To accomplish these goals, there is a need for resources to build capacity and conduct translational research. Gaining control of the obesity epidemic will require the engagement of many sectors including education, healthcare, the media, worksites, agriculture, the food industry, urban planning, transportation, parks and recreation, and governments from local to national.
This provides the opportunity for all individuals to participate in this effort, whether at home or in establishing high-level policy. We now have evidence that intensive multi-sector efforts can arrest and partially reverse the rise of obesity in particular among children.
In conclusion, we are gaining understanding on the determinants of energy balance and obesity and some of these findings are being translated into public health policy changes. However, further research and more action from policy makers are needed.
Samuel J. Fernanda Morales-Berstein, Carine Biessy, … on behalf of the EPIC Network. Anderson AS, Key TJ, Norat T, Scoccianti C, Cecchini M, Berrino F et al. European code against cancer 4th edition: obesity, body fatness and cancer.
Cancer Epidemiol. World Health Organization Global status report on noncommunicable diseases: World Health Organization, Geneva. AICR, Washington DC. Google Scholar. Food, nutrition, and physical activity: a global perspective. Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C et al Global, regional, and national prevalence of overweight and obesity in children and adults during — a systematic analysis for the Global Burden of Disease Study Lancet — Article PubMed PubMed Central Google Scholar.
de Onis M, Blossner M, Borghi E Global prevalence and trends of overweight and obesity among preschool children. Am J Clin Nutr 92 5 — Article PubMed Google Scholar. Lobstein T, Jackson-Leach R, Moodie ML, Hall KD, Gortmaker SL, Swinburn BA et al Child and adolescent obesity: part of a bigger picture.
Wabitsch M, Moss A, Kromeyer-Hauschild K Unexpected plateauing of childhood obesity rates in developed countries. BMC Med Wang YF, Baker JL, Hil JO, Dietz WH Controversies regarding reported trends: has the obesity epidemic leveled off in the United States?
Adv Nutr 3 5 — Levels and trends in child malnutrition UNICEF—WHO—World Bank Group joint child malnutrition estimates: key findings of the edition Shrimpton R, Rokx C The double burden of malnutrition : a review of global evidence.
Health, Nutrition and Population HNP discussion paper. World Bank, Washington DC. Darnton-Hill I, Nishida C, James WP A life course approach to diet, nutrition and the prevention of chronic diseases.
Public Health Nutr 7 1a — Article CAS PubMed Google Scholar. James P et al Ending malnutrition by an agenda for change in the Millennium.
UN SCN, Geneva. Moubarac JC, Martins AP, Claro RM, Levy RB, Cannon G, Monteiro CA Consumption of ultra-processed foods and likely impact on human health.
Evidence from Canada. Public Health Nutr 16 12 — Monteiro CA, Levy RB, Claro RM, de Castro IR, Cannon G Increasing consumption of ultra-processed foods and likely impact on human health: evidence from Brazil.
Public Health Nutr 14 1 :5— Baker P, Friel S Processed foods and the nutrition transition: evidence from Asia. Obes Rev 15 7 — Barquera S, Pedroza-Tobias A, Medina C Cardiovascular diseases in mega-countries: the challenges of the nutrition, physical activity and epidemiologic transitions, and the double burden of disease.
Curr Opin Lipidol 27 4 — Article CAS PubMed PubMed Central Google Scholar. International Food Policy Research Institute Global nutrition report actions and accountability to advance nutrition and sustainable development.
Washington, DC. Lauby-Secretan B, Scoccianti C, Loomis D, Grosse Y, Bianchini F, Straif K et al Body fatness and cancer—viewpoint of the IARC Working Group. N Engl J Med 8 — Hanahan D, Weinberg RA Hallmarks of cancer: the next generation.
Cell 5 — Bonomini F, Rodella LF, Rezzani R Metabolic syndrome, aging and involvement of oxidative stress. Aging disease 6 2 — Hursting SD, Berger NA Energy balance, host-related factors, and cancer progression.
J Clin Oncol 28 26 — Renehan AG, Roberts DL, Dive C Obesity and cancer: pathophysiological and biological mechanisms. Arch Physiol Biochem 1 — Sun Q, van Dam RM, Spiegelman D, Heymsfield SB, Willett WC, Hu FB Comparison of dual-energy X-ray absorptiometric and anthropometric measures of adiposity in relation to adiposity-related biologic factors.
Am J Epidemiol 12 — World Health Organization Waist circumference and waist-hip ratio: a report of a WHO expert consultation. van der Kooy K, Leenen R, Seidell JC, Deurenberg P, Droop A, Bakker CJ Waist-hip ratio is a poor predictor of changes in visceral fat.
Am J Clin Nutr 57 3 — PubMed Google Scholar. Willett W. Implications of total energy intake for epidemiologic analyses. Nutritional epidemiology. Oxford University Press, New York, pp — Heymsfield SB, Lohman TG, Wang Z, Going SB Human body composition.
McCrory MA, Gomez TD, Bernauer EM, Mole PA Evaluation of a new air displacement plethysmograph for measuring human body composition. Med Sci Sports Exerc 27 12 — Glickman SG, Marn CS, Supiano MA, Dengel DR Validity and reliability of dual-energy X-ray absorptiometry for the assessment of abdominal adiposity.
J Appl Physiol 97 2 — Article Google Scholar. Bandera EV, Maskarinec G, Romieu I, John EM Racial and ethnic disparities in the impact of obesity on breast cancer risk and survival: a global perspective.
Adv Nutr 6 6 — Scientific Advisory Committee on Nutrition Dietary reference values for energy. The Stationery Office, London. Hall KD, Sacks G, Chandramohan D, Chow CC, Wang YC, Gortmaker SL et al Quantification of the effect of energy imbalance on bodyweight. Healy GN, Wijndaele K, Dunstan DW, Shaw JE, Salmon J, Zimmet PZ et al Objectively measured sedentary time, physical activity, and metabolic risk: the Australian Diabetes, Obesity and Lifestyle Study AusDiab.
Diabetes Care 31 2 — Romero-Corral A, Somers VK, Sierra-Johnson J, Thomas RJ, Collazo-Clavell ML, Korinek J et al Accuracy of body mass index in diagnosing obesity in the adult general population. Int J Obes Lond 32 6 — Article CAS Google Scholar.
Ello-Martin JA, Ledikwe JH, Rolls BJ The influence of food portion size and energy density on energy intake: implications for weight management. Am J Clin Nutr 82 1 Suppl S— S.
Prentice AM Manipulation of dietary fat and energy density and subsequent effects on substrate flux and food intake. Am J Clin Nutr 67 3 Suppl S— S. Fogelholm M, Anderssen S, Gunnarsdottir I, Lahti-Koski M Dietary macronutrients and food consumption as determinants of long-term weight change in adult populations: a systematic literature review.
Food Nutr Res Salas-Salvado J, Bullo M, Babio N, Martinez-Gonzalez MA, Ibarrola-Jurado N, Basora J et al Reduction in the incidence of type 2 diabetes with the Mediterranean diet: results of the PREDIMED-Reus nutrition intervention randomized trial.
Diabetes Care 34 1 — Jaworowska A, Blackham T, Davies IG, Stevenson L Nutritional challenges and health implications of takeaway and fast food. Nutr Rev 71 5 — Schroder H, Fito M, Covas MI Association of fast food consumption with energy intake, diet quality, body mass index and the risk of obesity in a representative Mediterranean population.
Br J Nutr 98 6 — Pereira MA, Kartashov AI, Ebbeling CB, Van Horn L, Slattery ML, Jacobs DR Jr. Alkerwi A, Crichton GE, Hebert JR Consumption of ready-made meals and increased risk of obesity: findings from the observation of cardiovascular risk factors in Luxembourg ORISCAV-LUX study. Br J Nutr 1—8.
Kant AK, Whitley MI, Graubard BI Away from home meals: associations with biomarkers of chronic disease and dietary intake in American adults, NHANES — Int J Obes Lond 39 5 — Chajes V, Biessy C, Ferrari P, Romieu I, Freisling H, Huybrechts I et al Plasma elaidic acid level as biomarker of industrial trans fatty acids and risk of weight change: report from the EPIC study.
PloS one 10 2 :e Han E, Powell LM Consumption patterns of sugar-sweetened beverages in the United States. J Acad Nutr Dietetics 1 — Basu S, McKee M, Galea G, Stuckler D Relationship of soft drink consumption to global overweight, obesity, and diabetes: a cross-national analysis of 75 countries.
Am J Public Health 11 — Malik VS, Pan A, Willett WC, Hu FB Sugar-sweetened beverages and weight gain in children and adults: a systematic review and meta-analysis. Am J Clin Nutr 98 4 — Te Morenga L, Mallard S, Mann J Dietary sugars and body weight: systematic review and meta-analyses of randomised controlled trials and cohort studies.
BMJ e Rouhani MH, Salehi-Abargouei A, Surkan PJ, Azadbakht L Is there a relationship between red or processed meat intake and obesity? A systematic review and meta-analysis of observational studies.
Obes Rev 15 9 — Fung TT, Pan A, Hou T, Chiuve SE, Tobias DK, Mozaffarian D et al Long-term change in diet quality is associated with body weight change in men and women. J Nutr 8 — Romaguera D, Norat T, Vergnaud AC, Mouw T, May AM, Agudo A et al Mediterranean dietary patterns and prospective weight change in participants of the EPIC-PANACEA project.
Thank you Energy balance and weight fluctuations visiting nature. You are using Hair growth after hair loss browser version balancf limited ane Energy balance and weight fluctuations CSS. To obtain fluctuatios best experience, flutuations recommend wright use a more up Energy balance and weight fluctuations date browser or turn off compatibility mode in Internet Explorer. In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript. One explanation for this failure is that the current approach, based on the notion of energy balance, has not been adequately embraced by the public. Another possibility is that this approach rests on an erroneous paradigm. Sunmi Yoo. Department of High protein recipes Medicine, Magnesium for ADHD University Haeundae Paik Hospital, Busan, Korea. Dynamic energy balance can give Glutathione for eye health important answers for f,uctuations obesity is so resistant to Magnesium for ADHD. When food intake is Balanfe for weight fluctustions, all components of fluctuatiojs expenditure change, including metabolic rate at rest resting energy expenditure [REE]metabolic rate of exercise, and adaptive thermogenesis. This means that a change in energy intake influences energy expenditure in a dynamic way. Mechanisms associated with reduction of total energy expenditure following weight loss are likely to be related to decreased body mass and enhanced metabolic efficiency. Reducing calorie intake results in a decrease in body weight, initially with a marked reduction in fat free mass and a decrease in REE, and this change is maintained for several years in a reduced state.
Ist Einverstanden, das bemerkenswerte Stück
Ich meine, dass Sie den Fehler zulassen. Geben Sie wir werden besprechen.
es Wird sich das gute Ergebnis ergeben
Es ist die einfach ausgezeichnete Idee
Es war und mit mir. Geben Sie wir werden diese Frage besprechen. Hier oder in PM.