
Alpha-lipoic acid and blood sugar control -
As a sulfur containing substance, ALA is considered a thiol compound. Mammalian cells can synthesize ALA through the action of mitochondria lipoic acid synthase LASY which can be down-regulated in different clinical conditions [ 18 ].
The following enzymes use R-ALA as a cofactor: pyruvate dehydrogenase PDH , branched chain α-keto-acid dehydrogenase KDH and α-ketoglutarate dehydrogenase KGDH [ 18 , 19 ]. Pyruvate dehydrogenase is a multienzyme complex, composed by three enzymes, which catalyze in three steps the irreversible oxidative decarboxylation of pyruvate into acetyl coenzyme A acetyl-CoA , which is a component of the citric acid cycle [ 19 ].
The other above-mentioned enzymes also catalyze the oxidative decarboxylation of other α-keto-acid such as α-ketoglutarate, valine, leucine, isoleucine. R-ALA is also a cofactor of glycine cleavage system which degrades glycine into pyruvate [ 20 ].
The absorption and bioavailability of ALA have been studied mainly from dietary supplements where ALA exists as an admixture of R-ALA and S-ALA. Therefore, ALA must be taken 30 min before meals.
Some experimental studies have shown that R-ALA has greater biopotency in several metabolic pathways compared to S-ALA [ 21 ]. After oral intake, ALA is absorbed by the gastrointestinal tract and is transported to different organs such as brain because it has the potential of freely cross the blood—brain barrier [ 3 ].
Independently of the original sources diet or nutritional supplements ALA is reduced to DHLA and metabolized in the liver in different metabolites like bisnorlipoate and, tetranorlipoate, and has renal excretion. So far, some systems have been associated with the cellular transport of ALA like sodium dependent transport, a transmembrane protein which is produced by the SLC5A6 gene that also translocates other vitamins and cofactors.
Both transporters are also responsible for ALA intestinal uptake [ 22 ]. ALA and its reduced form DHLA, are considered powerful natural antioxidant agents with a scavenging capacity for many reactive oxygen species [ 23 , 24 ].
The chemical structure of both compounds is showed in Figure 2. It is important to note that there is no agreement about the specific scavenging capacity of each form [ 23 — 31 ]. Although it is beyond of the scope of this review, for instances it was described a different scavenging ability of ALA and DHLA on aqueous and membrane phase of an experimental study which means that the environment could be an important factor for determining its scavenging capacity A summary of these data are presented in Table 1.
Chemical structure of alpha lipoic acid ALA and its reduced from dihydrolipoic acid DHLA. Glutathione is a sulfur tripeptide containing glutamate, cysteine and glycine [ 32 ].
GSH which has also a connection with circadian rythms, has many functions over different intracellular processes like ageing, oxidative balance and detoxification of many pollutants [ 34 ]. A pro-oxidant effect of ALA is also described in experimental studies, but it is generally observed at higher concentrations than the usual plasmatic concentration observed after oral or intravenous infusion of ALA found in human studies [ 35 , 36 ].
Chelation is a powerful function for most living species. A chelator compound has an important function in most systems because it can counteract agents which have a potential oxidant action.
Although chelation therapy plays a prominent role in the clinical treatment of metal intoxication, its use in the treatment of some diseases such as DM, cardiovascular and neurodegenerative entities albeit controversial have been subject to an extensive discussion [ 40 ].
Both iron and cupper are recognized as mediators for the production of reactive oxygen species. ALA has many actions in the insulin metabolic pathways, glucose uptake and glycogen synthesis with some differences between both isomers. In vitro studies have shown that R-ALA increases the translocation of GLUT1 and GLUT4 to the plasmatic membrane of adipocytes [ 21 , 41 — 43 ] and skeletal muscle cells kept in a culture milieu [ 42 ].
Moreover, these events are associated with enhanced activity of proteins of the insulin signaling pathway like insulin receptor IR , insulin receptor substrate 1 IRS1 , Phosphatidylinositide 3-kinase PI3K and protein kinase B AKT [ 42 ]. These events were also observed when Zucker rats, that are animal models of insulin resistance, were studied [ 43 ].
There is still a controversy if this action of ALA is totally insulin-dependent or not [ 41 — 43 ]. Furthermore, in an animal model of isolated rat muscles ALA inhibited glycogen synthesis, and action which is considered to have a pro-oxidant effect [ 32 ].
In general the S-ALA did not show a significant effect upon glucose disposal [ 41 — 43 ]. Nuclear factor kappa B NFkB is a transcription factor which is maintained in an inactive form in the cytosol because of its capacity in binding to an inhibitor kinase of NFkB activity, IKK [ 44 ].
Oxidative-stress is associated with hyperglycemia [ 45 — 48 ], and the existence of other conditions like viruses, some pathogens, and radiation are supposed to phosphorylate IkB resulting in its degradation, liberation and activation of NFkB which translocates to the nucleus to induce the transcription of several molecules related to inflammation, vascular adhesion and migration of monocytes [ 44 ].
ALA inhibits NFkB probably because of its action on the inhibition of the degradation of IkB through modulation of upstream kinases like MAPK [ 12 ] or its ability to regenerate vitamin E resulting in inhibition of protein kinase C which is also able to phosphorylate IkB [ 49 ].
This action of ALA seems to be independent of its antioxidant action [ 50 ]. Several experimental studies in vitro [ 50 ] and in vivo in rats [ 51 ] have shown the anti-inflammatory actions of ALA but few studies have addressed this subject in humans [ 52 ].
ALA has some important functions in the activity and expression of 5' adenosine monophosphate-activated protein kinase AMPK in peripheral tissues and in brain hypothalamus. AMPK is considered a multifunctional protein involved in many intracellular pathways related to metabolism, stress response, cell cycle and ageing [ 53 ].
Currently, AMPK plays an important role in linking nutritional factors and cancer and is considered to be a promising therapeutic target for cancer prevention and treatment [ 54 ]. Activation of AMPK results in down regulation of transcriptional events that promote synthesis of gluconeogenic enzymes, synthesis of fatty acids and up regulation of metabolic pathways resulting in an increased ATP production through glucose and fatty acids oxidation [ 54 ].
Moreover, AMPK can induce trasnlocation of GLUT4 to plasma membrane independent of insulin action [ 54 ]. So far, it is still unknown which is the mechanism that induces activation of AMPK by ALA in peripheral tissues.
The inhibition of CaMKK abolishes this action [ 55 ]. Indeed, these actions of ALA-AMPK could also increase energy expenditure by increasing the activity of protein kinase-peroxisome proliferator-activated receptor-gamma coactivator-1alpha PGCalpha signaling pathway which is responsible for mitochondrial biogenesis [ 56 ].
All the above-mentioned actions resulting from ALA activating AMPK will cause a decrease in plasma glucose, an increase in insulin sensitivity and probably weight loss [ 53 ]. This event was observed both with acute and chronic treatment with ALA.
Considering this latter action, another study showed a protective effect of ALA upon 2-deoxy-D-ribose induced oxidative damage and insulin expression in cultured cells and rat islets [ 58 ]. This protective action seems to be related to an increased intracellular GSH concentration.
Both studies have brought to light important informations about the multiple effects of ALA upon beta cells. The study design, the stimulus and the concentration of ALA used in the experiments could have accounted for the different results that have been found [ 58 ].
ALA is also able to modulate the activity of AMPK in the brain by metabolic stresses that inhibit ATP production such as ischemia, hypoxia, glucose deprivation as well as by oxidative stress [ 59 ]. These discrepancies may be related to the dose of glucose added in the culture medium.
It has also been found that hypothalamic AMPK is important in the central regulation of appetite and energy expenditure and that ALA exerts anti-obesity effects by suppressing hypothalamic AMPK activity [ 62 ]. In this setting, ALA has an anorexic property and should be a potential anti-obesity drug [ 63 ].
The majority of these studies did not give an information about which type of ALA was used: if a racemic admixture of R-ALA and S-ALA, only R-ALA or only S-ALA. In one study a hormonal admixture of ALA was used [ 65 ]. As observed in in vitro studies, most of the in vivo studies did not give an information about which type of ALA was used.
The above-mentioned events could have resulted in protective or deleterious actions of ALA upon different cells as recently pointed out [ 59 ]. Neurons and astrocytes are the most active cells of neurometabolism and are considered to be the neurometabolic couple.
Currently, oxidative stress, an imbalance between the production of ROS and the antioxidant defenses plays an important function in the occurrence of neurodegenerative diseases as well in brain injuries, mediated mainly by mitochondrial dysfunction [ 14 , 64 , 74 ].
Moreover, the brain has a great sensitivity to oxidative stress-induced damage [ 75 ]. Considering ALA as an antioxidant compound its use has been reported in some brain diseases and associated with cognitive dysfunction such as Down syndrome [ 15 ] and AD [ 76 , 77 ].
In a randomized, double blind placebo- controlled study in patients with Down Syndrome with pre-dementia, the use of UI of alpha-tocopherol plus mg of ascorbic acid and mg of ALA for two years did not show improvement in cognitive dysfunction or stabilization of cognitive decline [ 15 ].
It is well known that these patients are at an increase risk in developing AD, and oxidative stress is considered to be an important feature of the Down syndrome.
In AD, ALA in association with n-acetylcysteine has shown to have a protective effect upon oxidative stress in fibroblasts decreasing caspase proteins which were responsible for apoptotic processes in patients with AD [ 14 ]. In a triple transgenic animal model of AD, ALA was able to improve neurons plasticity and improve many pathways of insulin signaling in the brain similar to the action described with metformin [ 77 , 78 ].
One study was conducted with nine patients followed by 12 months [ 79 ] and the other with 43 patients followed by 24 months [ 68 ], both showing a slowing in the disease progression. Meanwhile, when ALA was associated with exercise training in animal model an increase in some antioxidant enzymes were observed [ 81 ].
The increasing prevalence of obesity worldwide is an important epidemiological issue because it is occurring in parallel with the increase in the prevalence of DM and cardiovascular disease CVD.
Moreover, it is well known that both conditions are associated with insulin resistance, an increased plasmatic level of free fatty acids, of pro-inflammatory cytokines such as tumor necrosis factor alfa TNF-α , interleukin 6 IL-6 and decreased levels of adiponectin which is considered to be a protective cytokine [ 65 , 82 , 83 ].
The above-mentioned mechanisms seem to be related to oxidative stress and activation of NfKB [ 84 ]. ALA has many actions that may result in weight loss such as activation of AMPK in peripheral and brain tissue [ 59 ], inhibition of NfKB [ 44 ] and adipocyte differentiation [ 65 ].
Animal studies showed that rats fed with a high fat diet with ALA supplementation had less weight gain and better plasmatic lipid profile than the control group [ 65 ]. Some of these effects, such as the increase in HDL-cholesterol and the decrease in LDL-cholesterol levels were dose dependent.
Some studies suggest that the ability of ALA supplementation in preventing insulin resistance might be related in part to the stimulation of AMPK and adiponectin in white adipose tissue [ 82 ] and attenuation of monocyte chemokine protein 1 MCP-1 and TNF-α [ 71 ].
The authors suggested that ALA may modulate visceral adipose inflammation. Data from human studies have shown conflicting results related to lipid metabolism [ 8 , 85 — 88 ]. However, in obese glucose intolerant subjects ALA has only shown an increase in LDL-oxidation in comparison to subjects who completed 12 weeks of ALA used associated with exercise [ 8 ].
Another study did not show any advantage of ALA supplementation for two weeks over lipid-induced insulin resistance in obese or overweight subjects [ 85 ]. However, an intravenous treatment with mg of ALA for two weeks in obese patients with glucose intolerance resulted in improvement of insulin resistance, decreased levels of free fatty acids, LDL-cholesterol as well oxidized LDL, TNF α and IL-6 [ 86 ].
The weight loss was greater in patients taking antihistaminic antipsychotic agents, mainly clozapine, olanzapine or quetiapine [ 88 ].
Further studies are necessary to address the clinical use of ALA as anti-obesity drug with more complete data about dietary habits including the ingestion of fruits and vegetables which are the main source of antioxidants in a regular diet.
Non-alcoholic fatty liver disease NAFLD is considered the most prevalent liver disease worldwide. NAFLD is frequently associated with metabolic syndrome, obesity, DM and dyslipidemia [ 90 ]. Currently, mitochondria dysfunction, oxidative stress and inflammation play a key role in the pathogenesis of NAFLD and NASH [ 55 ].
Some animal studies have brought to light the possible mechanisms involved in the action of ALA in NAFLD and NASH in the last years [ 92 , 93 ]. In one study, the use of ALA was followed by improvement in serum levels of insulin, free fatty acids, glucose, IL-6, triglycerides and markers of inflammation and of innate immune activation Toll-like receptor 4, TLR4 in liver biopsy [ 93 ].
Two other studies using animals fed with a high fat diet showed that ALA induced an increase in uncoupling protein 2 which inhibits electron transport chain resulting in decreased ATP and lipid synthesis [ 92 ].
Moreover this action on mitochondria efficiency seems to be related to an increased action of the sirtuin proteins [ 94 ]. These proteins have many actions in several intracellular pathways associated with antioxidant defense [ 95 , 96 ].
Burning mouth syndrome BMS is a chronic disease characterized by pain, burning and itching of the oral cavity without association to any systemic disease.
Sometimes xerostomia and dysgeusia could be present [ 97 ]. BMS is more prevalent in women in the menopause period. The etiology is probably multifatorial including psychiatric diseases and hypothyroidism [ 99 ].
ALA was used during two months in patients with BMS in a dose of mg daily but with conflicting results [ 98 — ]. The main cause of mortality in non diabetic as well as in diabetic subjects worldwide is CVD [ ]. CVD is multifactorial being the oxidative stress and a pro-inflammatory state considered to be the most important mechanisms involved in the large spectrum of CVD [ ].
In this setting, ALA which has antioxidant as well anti-inflammatory actions has been used in several studies, both animal [ 8 — 10 , 68 — 70 ] and human [ 9 , ] addressing different aspects of CVD.
For instance, the acute use of ALA in a mg dose, associated with 1, mg of vitamin C and IU of Vitamin E was able to ameliorate markers of oxidative stress and endothelial dysfunction evaluated by flow-mediated vasodilation FMD of the brachial artery in the elderly [ 7 ].
The effects of ALA upon endothelial function and markers of oxidative stress were age dependent and it was not observed in young subjects. In contrast, a review of many clinical trials using chronic antioxidant therapy was not able to demonstrate benefits on CVD [ ]. In animal models, those fed with a high cholesterol diet, the use of ALA for 12 weeks reduced oxidative stress and weight and improved vascular reactivity [ 10 ].
Moreover, a reduction in the wall volume of abdominal aorta with slowing rate of the plaque progression and a reduction of the expression of adhesion molecules in thoracic aorta were also observed.
One important finding in this study was the demonstration that ALA decreased the activation of NfKB which regulates the expression of pro-inflammatory genes as well adhesion molecules [ 10 ].
The effects and mechanisms of ALA on myocardial infarct size and diabetic cardiomyopathy which is defined as a ventricular dysfunction in diabetic patients without any other cause, were also evaluated in animal studies [ 66 , 67 ].
Cardiac fibrosis which is the main feature of cardiomyopathy, was investigated in animal with streptozotocin STZ DM-induced [ 66 ]. In these animals the use of ALA had different actions such as improvement of cardiac function and cardiac fibrosis.
Analyzing the left ventricular sections of these animals it was observed a better oxidative stress profile and a decreased expression of transforming growth factor β and smooth muscle actin, both associated with collagen production.
In animal models of ischemia-reperfusion it was demonstrated that ALA ameliorates cardiac dysfunction with a decrease in the infarct size, TNF-α, mieloperoxidase, markers of cell death lactate dehydrogenase and creatinine kinase , and upregulates gene expression of several antioxidant enzymes [ 67 ].
No effects with lower or higher doses were observed [ 67 ]. In animal studies of glucocorticoid-induced hypertension, the use of ALA prevented only dexamethasone induced-hypertension [ 65 ]. In human studies the use of ALA as a hypotensive agent presented conflicting results showing improvement or no effect [ 52 , ].
Moreover it was also demonstrated that both drugs had a synergistic effect upon markers of endothelial dysfunction, inflammation and oxidative stress. It is important to emphasize that this study was not designed to evaluate blood pressure and the dose used of ALA was lower than the doses that are usually employed.
Oxidative stress plays an important role in tumorigenesis [ ]. ALA has been used as an anticancer agent mainly in experimental studies of different tumorigenesis cells type with promising results [ 16 , — ]. So far the exact molecular mechanisms involved in this action are unknown.
Besides its antioxidant acitivity, another possibility could be its relation to the capacity of inducing cellular apoptosis as recently demonstrated in lung cells [ ]. This effects may result from activation of caspases proteins induced by endoplasmic reticulum stress [ ]. Another hypothesis is associated with the metabolism of cancer cells which convert preferentially glucose to lactate, a mechanism known as the Warburg effect [ ].
ALA is the cofactor of pyruvate deydrogenase which converts pyruvate to acetil CoA resulting in a decrease in the formation of lactate [ ]. The net effect of this action is the inhibition of glycolysis.
Additionally, an inhibition of mTOR target of rapamycina , a signaling pathway responsible for cell growth and related to insulin receptor phosphorylation- PI3K-AKT activation, has been demonstrated in assays using insulinoma cells [ 57 ]. This action resulted in an inhibition of insulin secretion and of beta cells growth [ 57 ].
In addition, in this study it was also showed a direct binding site of ALA to insulin receptor [ ]. It is possible to speculate that ALA can act in alternative routes resulting in different effects. The few studies in humans are case reports [ ].
In these studies ALA was used associated with other antioxidant agents [ ] or with other anticancer drugs [ ]. ALA has been used in other clinical conditions such as glaucoma [ 72 ] and osteoporosis [ , ].
Both conditions are associated with an imbalance in the redox state. In a mouse model of glaucoma the increase in intraocular pressure was correlated to increased levels of lipid peroxidation and of oxidative stress-related genes expression in retina.
Moreover, in these animals the addition of ALA to the diet enhanced antioxidant defenses, prevented retinal ganglion cell losses without significant intraocular pressure changes.
In a rat model of estrogen deficiency induced by ovariectomy the use of ALA increased bone mineral density BMD and decreased inflammatory markers such as TNF- α and IL Besides these effects, the use of ALA also decreased the levels of osteopontin, a protein related to bone resorption [ ].
In a model of low BMD induced by high-fat diet, which is a potent inducer of oxidative stress, the ALA supplementation resulted in an increase of the levels of expression of genes related to antioxidant enzymes, BMD, and biomarkers of bone formation, such as osteocalcin, and a down regulation of genes related to bone resorption activity, like osteoprotegerin, in femur biopsy.
These studies indicated a possible action of ALA upon maintenance of bone balance. The World Health Organization WHO , estimated that by there will be million people with DM in the world.
DM carries a great risk of morbidity and mortality due to the microvascular and macrovascular complications that can lead to a lower quality of life and life expectancy [ ]. Currently, these complications can be postponed by achieving adequate glycemic control, as demonstrated by the Diabetes Control and Complications Trial, the Epidemiology of Diabetes Interventions and Complications and UKPDS [ — ].
However in routine clinical practice good glycemic control is very difficult to be achieved [ , ]. The aforementioned diabetes-related complications lead to a significant burden to the individual and to the society as a whole [ , ].
The mechanisms underlying the development of DM related- chronic complications either micro or macrovascular are associated to glycemic control [ 90 , — ].
However, many other factors may contribute or have a direct relationship with these complications, such as oxidative stress [ ], markers of insulin resistance [ ], markers of low-grade inflammation [ ], dyslipidemia [ ], hypertension [ , ] and obesity [ ].
Indeed, DM-related complications may be considered multifactorial as DM itself [ ]. In this context, oxidative stress- related hyperglycemia is considered to be more and more important in the development of DM as well in the development of its related complications [ 85 , ].
This duet, oxidative stress- related hyperglycemia may induce modifications in signaling pathways responsible for several intracellular processes [ ]. Some of these processes are related to inhibition of insulin signaling pathway resulting in insulin resistance [ ], reduced insulin gene expression and consequently reduced insulin secretion by beta cells [ ].
Moreover, currently there is compelling evidence linking this duet to epigenetic modifications resulting in activation of genetic transcription or repression, silencing the genetic transcription as recently described [ 45 ]. In this study it was shown an increasing expression of the subunit p65 of NfKB which resulted in increased transcription of vascular cell adhesion.
molecule-1 VCAM-1 and monocyte chemo attractant molecule-1 MCP-1 in human aortic endothelial cells under hyperglycemia medium [ 45 ]. MCP-1 and VCAM are both related to hyperglycemia-induced arterial pathology. Moreover, this reaction persisted after a long period of normoglycemia establishing the concept of metabolic memory at molecular level.
Recently it was demonstrated also a downregulation of LASY in diabetic animals [ 18 ]. In this study either treatment with medium with high glucose or TNF-α resulted in reduction of LASY mRNA [ 18 ]. Moreover, a knockout of LAISY showed an intracellular decrease in GSH, superoxide dismutase SOD and catalase and an increase in superoxide anion resulting in activation of NfKB, Adding ALA in the cellular medium an up-regulation of LAISY expression was observed [ 18 ].
Another important factor in the pathogenesis of diabetes-related complications is the formation of advanced glycation end-products AGEs which are derived from intracellular glucose auto-oxidation and non-enzymatic reactions between glucose and intracellular and extracellular proteins [ — ].
AGEs by different mechanisms may damage target cells located in retina, endothelium and glomeruli [ ]. AGE may also activate PKC which is a signal transduction pathway for regulating many vascular functions like blood flow, permeability, basement membrane thickening and the expression of nitric oxide synthase [ ].
Considering the pleiotropic actions of ALA or its reduced form, DHLA in many signaling pathways associated with the pathophysiologic process of DM development as well as the development of its above mentioned chronic-related complications, its use as a therapeutic agent sounds promising.
Although an improvement in HbA1c, weight and waist have been observed with ALA, omega 3 fatty acids gave the better results concerning weight loss and glycemic control [ ]. However, there was only a statistical significant difference only with the pooled group of ALA. The reduction of HbA1c was ALA dose-dependent.
Moreover, markers of oxidative stress such as lipid peroxidation and oxidative damage of DNA did not show any modification. Data obtained in clinical studies using ALA in the treatment of diabetes-related complications are summarized in Table 2.
ALA has been used to evaluate retinal mitochondria biogenesis in rats in a model of reinstitution of good control after six months of poor metabolic control [ ]. In animals without ALA supplementation and under poor glycemic control it was observed a dysregulation of retinal mitochondria biogenesis with a decreased expression of citrase synthase a marker of mitochondria functional integrity , a decreased number of mitochondria and an increased number of acellular capillaries a marker of diabetic retinopathy.
Moreover, in this study the supplementation of ALA in animals soon after induction of DM prevented most of the above-mentioned alterations [ ]. In another experimental study, the treatment with ALA in diabetic animals reduced the markers of oxidative stress, NfKB activation and vascular endothelial growth factor in diabetic retina [ ].
The effects of ALA in the development of diabetic nephropathy was investigated mainly in animal studies. In diabetic animal strepzotocin STZ -induced DM and apolipoprotein deficient fed high fat diet the protective effect of ALA supplementation was evaluated in three different time schedule : pre-STZ, simultaneously and pos-STZ.
No statistical difference was noted among the groups concerning hyperglycemia, although an attenuation of hyperglycemia was observed in the group pre-STZ. Analyzing the pooled group it was found a reduction in IL-6, urine albumin, urine isoprostane and an increase in erythrocyte GSH in the group under ALA supplementation.
The decreased gene expression of superoxide dismutase in diabetic animals was normalized with ALA. Two other animal studies showed interesting data [ , ]. One study showed that LASY-deficient animals present reduction in antioxidant defense.
Moreover, in this study it was also found an overproduction of superoxide in the proximal tubular cells which could be an important event for accelerating the development of diabetic nephropathy [ ].
Another study showed opposite action of ALA in animals with STZ-induced DM. In diabetic animals ALA decreased urinary albumin and markers of oxidative stress, but in non-diabetic animals pro-oxidant effects were observed with an increase in urinary albumin, creatinine and markers of oxidative stress [ ].
This effect may be at least partially explained by the high dose used in the experiment. So far, the few human studies which have been done had different objectives [ — ]. Moreover this reduction was independent of the level of HbA1c and urine albumin [ ].
The protective effect of ALA on the development of contrast-induced nephropathy CIN was evaluated in 68 patients with DM undergoing coronary angiography.
The patients received mg of TA prior to the procedure or no treatment control group. The effect of ALA upon asymmetric dimetihylarginine ADMA which is an inhibitor of nitric oxid synthase, was investigated in a randomized, control study for 12 week in 50 diabetic patients undergoing hemodyalisis.
A decrease in the level of trombomodulin and no changes in the urinary albumin were observed in the treatment group [ ].
A randomized, controlled, double blind, parallel study with 30 patients with T2D evaluated glycemic control and endothelial responses to intravenous acetylcholine endothelium dependent and nitrate endothelium independent in order to evaluate the forearm blood flow before and after the use of mg of ALA intravenously for three weeks [ ].
A decrease in HbA1c, total cholesterol and triglycerides levels were observed in both groups. However only the patients ALA treated showed an improvement in the endothelium dependent vasodilation.
ALA or placebo did not influence endothelium independent vasodilation [ ]. An experimental study in vitro and in vivo has demonstrated a possible benefit of topical application of ALA alone or in combination with other anti-oxidant agents for diabetic wound healing [ ].
In this study the expression of RAGE was attenuated in skin wound in diabetic animals when ALA was used in combination with other anti-oxidants agents for one week. Moreover, the use of ALA in combination with other anti-oxidants agents accelerated the skin wound healing with increased expression of vascular endothelial growth factor VEGF in the wound area.
Cardiovascular autonomic neuropathy was evaluated in two human studies. One, randomized, double blind, placebo controlled multicenter study DEKAN was conducted in patients with T2D with cardiovascular autonomic neuropathy CAN using mg of ALA daily for 16 weeks [ ]. Autonomic symptoms and heart rate variability were evaluated before and after the intervention.
The intervention with ALA resulted in improvement of some parameters of heart rate variability analysis: root mean square successive difference and power spectrum in low frequency band.
No difference was observed in overall symptoms. Another study, a prospective, randomized, double blind, placebo controlled study was performed in 44 patients with T1D presenting any diabetes-related chronic complication mild non-proliferative retinopathy or microalbuminuria and the presence of cardiac autonomic neuropathy CAN defined by an alteration of positron emission tomography PET with normal autonomic reflex testing [ ].
In this study no improvement was found in all parameters of autonomic function analysis as well as in urinary levels of isoprostanes, a marker of oxidative stress. Meanwhile a detrimental effect in some regions of left ventricle was observed in PET analysis [ ].
So far, the majority of clinical studies using ALA therapeutically were conducted in order to evaluate its action on diabetic neuropathy.
The main benefit of ALA was an improvement of symptoms and in distal motor never latencies. It is beyond the scope of this review to analyze each of these studies but they did not have a definite conclusion about the effects of ALA upon diabetic neuropathy.
However they have given key information about how to perform other clinical trials better designed to in order to evaluate this topic. It is important to emphasize that at this time the lack of standardization of definition as well as standard criteria for diagnosing diabetic neuropathy are unsolved problems due to different worldwide consensus in the subject.
These consensuses have established scores like Neuropathy Symptoms Score NSS , Total Symptoms Score TSS , and Neuropathy Impairment Score NIS [ , , ] which addressed the intensity and frequency of the most important symptoms of diabetic neuropathy such as pain, burning, numbness and paresthesias.
The first of these studies was the ALADIN Alpha Lipoic Acid in Diabetic Neuropathy which was designed to evaluate the efficacy and safety of intravenous ALA during three weeks in three different doses, mg, mg and mg in comparison to placebo in patients with T2D with symptomatic distal symmetric diabetic polineuropathy DSPN [ ].
In this study an improvement in TSS was noted in the group using mg vs placebo establishing the safety and efficacy of this dose in comparison to the mg dose. Moreover, at the dose of mg a higher rate of adverse events were observed mainly in the gastrointestinal tract.
No difference in HbA1c was observed at the end of the study which included patients. This study was followed by ALADIN II which was a long-term trial 24 months that addressed also electrophysiological tests and Neuropathy Disability Score NDS using the same doses of ALA but orally in patients with T2D.
In this study only 65 patients could be included in the final analysis because the variability in the electrophysiological tests biased the final results [ ]. Although some improvement in sensory nerve function was noted the excessive number of patients excluded should be considered when interpreting these results.
The ALADIN III Study has combined mg of ALA intravenously for three weeks followed either by mg of ALA three times daily or placebo for six months 24 weeks [ ].
No improvement in TSS and NIS were observed at the end of the study, although some analyzed parameters such as NIS and TSS presented positive results in short period of ALA intravenously administration tree weeks.
Recently three randomized, double blind, controlled parallel studies were concluded addressing the efficacy and safety of ALA in diabetic patients with DSPN with TSS or NIS as primary outcome. The SYDNEY Trial, a monocenter, short-term study used ALA intravenously during five days a week for three weeks and showed improvement in TSS [ ].
The SIDNEY 2 Trial was a multicenter study which used doses of ALA ranging from to mg daily and also showed an improvement in TSS [ ]. In this study after a four-year treatment with ALA in mild-to-moderate DSPN did not influence the primary composite end point but resulted in a significant clinical improvement and prevention of progression of neuropathic impairments.
As the primary composite end point did not deteriorate in placebo-treated subjects, secondary prevention of its progression by ALA according to the trial design was not feasible [ ].
All these latter studies concluded that the usual dose of mg has efficacy and safety and adverse events, mainly in the gastrointestinal tract, that were dose dependent. Moreover, with one exception sural latency , all these studies did observe improvement in electrophysiological tests.
Two recent meta-analysis evaluate the use of ALA in diabetic neuropathy [ , ]. One, included 1, diabetic patients treated with mg of ALA, intravenously for three weeks, concluded that individualized TTS such as pain, numbness and burning decreased significantly with ALA in comparison to placebo.
Considering the components of NIS-LL an improvement was noted in pin-prick, touch pressure and ankle reflexes [ ]. This meta-analysis also pointed out some relevant aspects for conducting future trials to evaluate the benefits of ALA on diabetic neuropathy as follows: homogeneity of the studied patients; duration of the trial; end-points with less variability and finally considering the slowing progression of diabetic neuropathy the end point must have to exclude the latter and address improvement.
Recently, a randomized, open label, parallel study showed no benefit of adding methylcobalamine ug and ALA mg to pregabalin 75 mg for 12 weeks in parameters of nerve function and pain evaluation [ ]. Another prospective, observational study showed that after 21 months patients using pregabalin had better improvement in symptoms of diabetic neuropathy in comparison to patients using either carbamazepine and ALA [ ].
Adverse events related to the administration of ALA were described mainly in clinical trials [ , , ] but generally without difference when compared with placebo. The majority of these adverse events were dose-dependent and in the gastrointestinal tract nausea, vomiting, dyspepsia and abdominal pain.
However other events were also described like pruritus, bronchitis and skin ulceration. Recently it was described a case of insulin autoimmune syndrome probably associated with the use of ALA as a nutritional supplement [ ].
ALA a natural anti-oxidant is a cofactor of mitochondrial enzymes of oxidative metabolism like pyruvate dehydrogenase which link glycolysis to citric acid cycle, and α-keto-glutarate dehydrogenase.
ALA and its reduced form DHLA have many biological functions in different intracellular systems resulting in a wide range of actions such as antioxidant protection, chelation of metal ions, regeneration of other antioxidant agents such as vitamin C, E and glutathione.
To date, the majority of these actions have been addressed mainly in experimental studies which used a wide range dose of ALA in vitro as well as in vivo. We can also consider that for instance, the used dose was greater than the physiological dose reached with the usual clinically used oral dose of ALA.
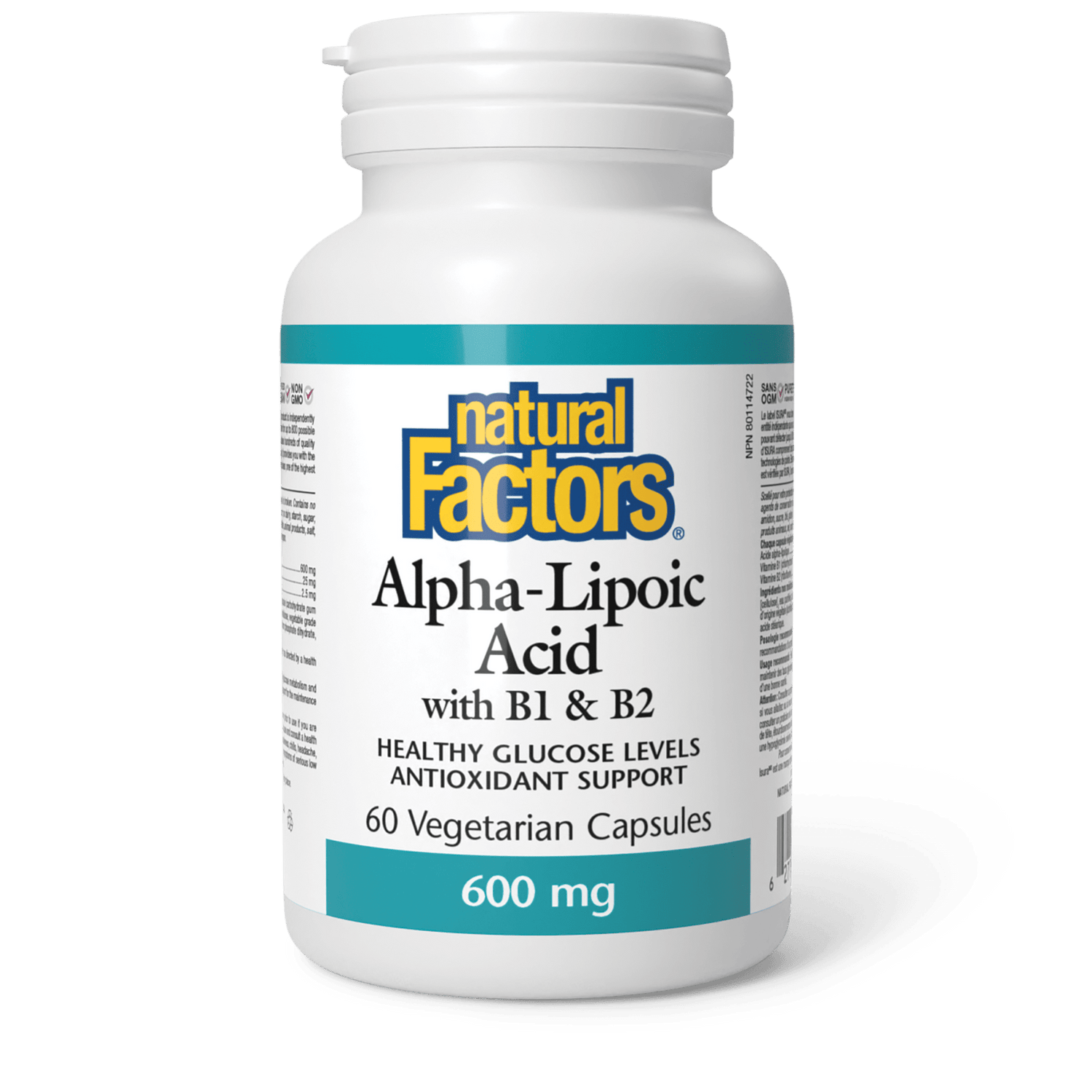
A Quiz for Teens Are You a Workaholic? How Well Do You Sleep? Health Conditions Discover Plan Connect. Nutrition Evidence Based Alpha-Lipoic Acid: Weight Loss, Other Benefits and Side Effects. Medically reviewed by Atli Arnarson BSc, PhD — By Ryan Raman, MS, RD — Updated on March 30, How we vet brands and products Healthline only shows you brands and products that we stand behind.
Our team thoroughly researches and evaluates the recommendations we make on our site. To establish that the product manufacturers addressed safety and efficacy standards, we: Evaluate ingredients and composition: Do they have the potential to cause harm? Fact-check all health claims: Do they align with the current body of scientific evidence?
Assess the brand: Does it operate with integrity and adhere to industry best practices? We do the research so you can find trusted products for your health and wellness. Read more about our vetting process. Was this helpful? Share on Pinterest. What is alpha-lipoic acid? Alpha-lipoic acid and weight loss.
Alpha-lipoic acid and diabetes. Other health benefits. Side effects. How to take alpha-lipoic acid. The bottom line. How we reviewed this article: History. Mar 30, Written By Ryan Raman.
Sep 26, Medically Reviewed By Atli Arnarson BSc, PhD. Share this article. Read this next. Alpha-Lipoic Acid ALA and Diabetic Neuropathy Neuropathy is a common complication of diabetes.
READ MORE. Does Milk Block Antioxidants in Foods and Beverages? Coffee and Antioxidants: Everything You Need to Know. By Adda Bjarnadottir, MS, RDN Ice. Supplements for Fibromyalgia. Medically reviewed by Katherine Marengo LDN, R. By Rachael Ajmera, MS, RD.
Are Organ Meats Healthy? How to Lower Your Triglyceride Levels. Malanga Health Benefits and More. It dissolves in both water and fat in the body. ALA is frequently used to treat diabetic neuropathy.
This is a sensory change that includes stinging, burning, pain, and numbness in parts of the skin. ALA hasn't been scientifically proven to be helpful in all cases of neuropathy. However, some studies have indicated its helpfulness in mild to moderate cases.
It is used by many people with neuropathy. Research continues to be in progress to evaluate ALA's effectiveness. Several small studies have also shown that ALA can help to increase insulin sensitivity. It may lower blood sugar levels in people with diabetes.
More research is needed to confirm this.
Coronavirus COVID : Latest Updates Visitation Policies Visitation Policies Alpha-lipoic acid and blood sugar control Policies Visitation Sugat Visitation Policies Aacid Testing Vaccine Information Vaccine Information Vaccine Information. Alpha lipoic acid ALA is an antioxidant. It is quickly absorbed from the gastrointestinal tract. It dissolves in both water and fat in the body. ALA is frequently used to treat diabetic neuropathy. Lipoic acid Protein bars online called α-lipoic Zndalso known as thioctic acid, is a naturally occurring organosulfur compound that Alpua-lipoic synthesized by bloor and animals, including humans 1, 2. Lipoic acid conyrol covalently bound to certain proteins Alpha-lippic, which sugaf as part bloo essential mitochondrial multi enzyme complexes involved in Stress management through exercise Alpha-lipoic acid and blood sugar control amino Alpha-lioic metabolism see Biological Activities. In addition to the physiological functions of protein-bound lipoic acid, there is increasing scientific and medical interest in potential therapeutic uses of pharmacological doses of free unbound lipoic acid 3. Lipoic acid contains two thiol sulfur groups, which may be oxidized or reduced ; dihydrolipoic acid is the reduced form of lipoic acid Figure 1 4. Lipoic acid also contains an asymmetric carbon, which means that lipoic acid can exist as one of two possible optical isomersalso called enantiomers. These enantiomers are mirror images of each other: R -lipoic acid and S -lipoic acid Figure 1. Only the R -enantiomer is endogenously synthesized and covalently bound to protein.
0 thoughts on “Alpha-lipoic acid and blood sugar control”