Diabetes oral drug therapy -
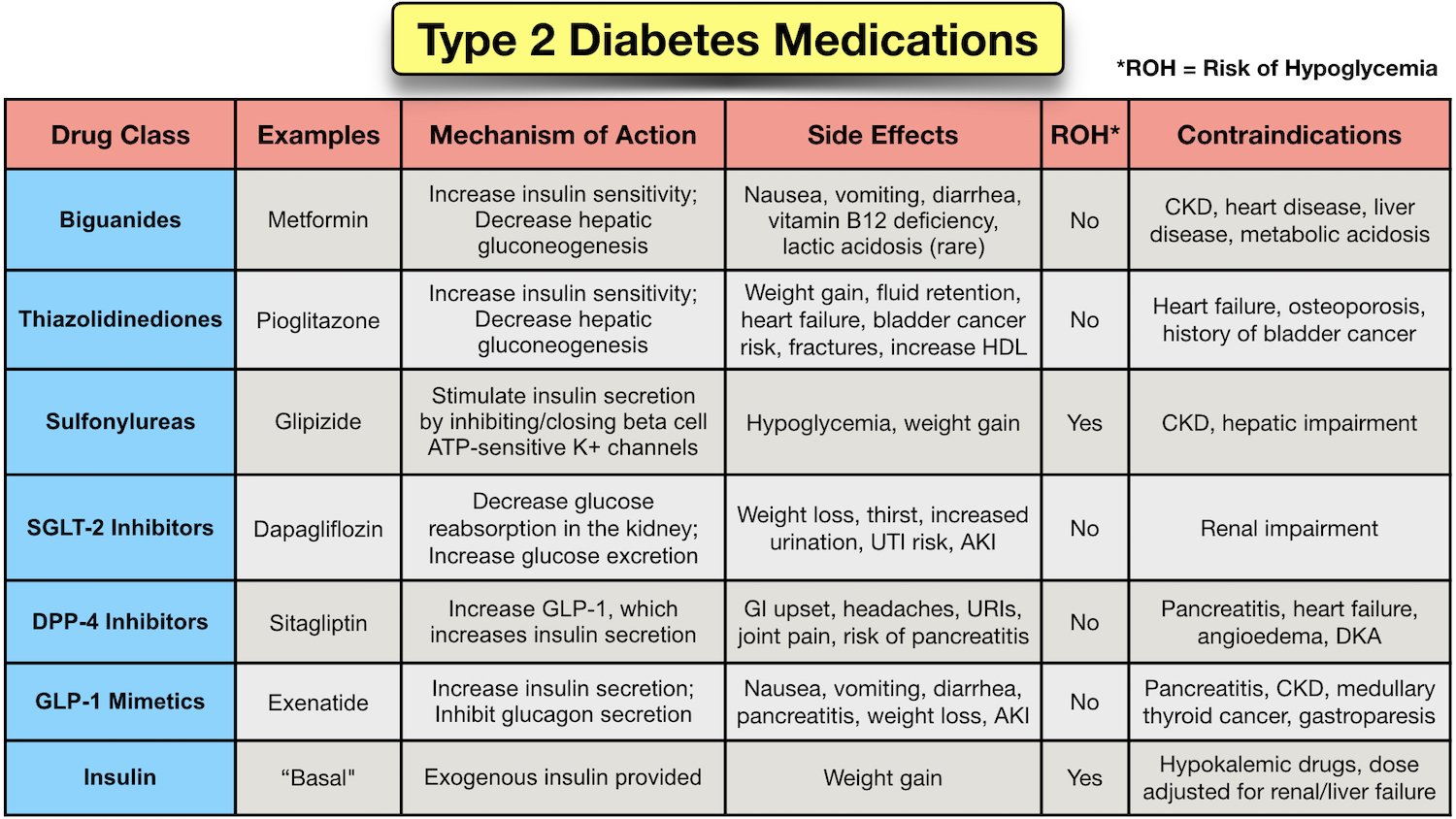
They work by preventing the breakdown of naturally occurring hormones in the body, GLP-1 and GIP. These hormones reduce blood glucose levels in the body, but they are broken down very quickly so it does not work well when injected as a drug itself.
By interfering in the process that breaks down GLP-1 and GIP, DPP-4 inhibitors allow these hormones to remain active in the body longer, lowering blood glucose levels only when they are elevated. DPP-4 inhibitors do not cause weight gain and are usually very well tolerated. As noted in the description for DPP-4 inhibitors, GLP-1 and GIP are natural hormones in the body that help maintain glucose levels.
These medications have similar effects to the GLP-1 and GIP produced in the body but are resistant to being broken down by the DPP-4 enzyme.
These medications can result in large benefits on lowering blood glucose and body weight. Some agents in this class have also been shown to prevent heart disease.
Most of these medications are injected, with the exception of one that is taken by mouth once daily, called semaglutide Rybelsus. How often you need to inject these medications varies from twice daily to once weekly, depending on the medication.
The most common side effect with these medications is nausea and vomiting, which is more common when starting or increasing the dose. Glucose in the bloodstream passes through the kidneys where it can either be excreted in the urine or reabsorbed back into the blood.
Sodium-glucose cotransporter 2 SGLT2 works in the kidney to reabsorb glucose. A new class of medication, SGLT2 inhibitors, block this action, causing excess glucose to be eliminated in the urine.
By increasing the amount of glucose excreted in the urine, people can see improved blood glucose, some weight loss, and small decreases in blood pressure. Bexagliflozin Brenzavvy , canagliflozin Invokana , dapagliflozin Farxiga , and empagliflozin Jardiance are SGLT2 inhibitors that have been approved by the Food and Drug Administration FDA to treat type 2 diabetes.
SGLT2 inhibitors are also known to help improve outcomes in people with heart disease, kidney disease, and heart failure. For this reason, these medications are often used in people with type 2 diabetes who also have heart or kidney problems.
Because they increase glucose levels in the urine, the most common side effects include genital yeast infections. Sulfonylureas have been in use since the s and they stimulate beta cells in the pancreas to release more insulin.
There are three main sulfonylurea drugs used today, glimepiride Amaryl , glipizide Glucotrol and Glucotrol XL , and glyburide Micronase, Glynase, and Diabeta. These drugs are generally taken one to two times a day before meals. All sulfonylurea drugs have similar effects on blood glucose levels, but they differ in side effects, how often they are taken, and interactions with other drugs.
The most common side effects with sulfonylureas are low blood glucose and weight gain. Rosiglitazone Avandia and pioglitazone Actos are in a group of drugs called thiazolidinediones. These drugs help insulin work better in the muscle and fat and reduce glucose production in the liver.
A benefit of TZDs is that they lower blood glucose without having a high risk for causing low blood glucose. Both drugs in this class can increase the risk for heart failure in some individuals and can also cause fluid retention edema in the legs and feet.
In addition to the commonly used classes discussed above, there are other less commonly used medications that can work well for some people:. Acarbose Precose and miglitol Glyset are alpha-glucosidase inhibitors.
These drugs help the body lower blood glucose levels by blocking the breakdown of starches, such as bread, potatoes, and pasta in the intestine. By slowing the breakdown of these foods, this slows the rise in blood glucose levels after a meal.
These medications should be taken with the first bite of each meal, so they need to be taken multiple times daily. Based on how these medications work, they commonly cause gastrointestinal side effects including gas and diarrhea.
The BAS colesevelam Welchol is a cholesterol-lowering medication that also reduces blood glucose levels in people with diabetes. BASs help remove cholesterol from the body, particularly LDL cholesterol, which is often elevated in people with diabetes.
The medications reduce LDL cholesterol by binding with bile acids in the digestive system. Thiazolidinediones activate peroxisome proliferator-activated receptor gamma PPAR-γ , a nuclear receptor, which increases insulin sensitivity and resultant peripheral uptake of glucose and increases the level of adiponectin, a fat tissue-secreted cytokine, that increases not only the number of insulin-sensitive adipocytes but also stimulates fatty acid oxidation.
Alpha-glucosidase inhibitors competitively inhibit alpha-glucosidase enzymes in the intestinal brush border cells that digest the dietary starch, thus inhibiting the polysaccharide reabsorption and the metabolism of sucrose to glucose and fructose. DPP-4 inhibitors inhibit the enzyme dipeptidyl peptidase 4 DPP- 4.
These deactivate glucose-dependent insulinotropic polypeptide GIP and glucagon-like peptide 1 GLP-1 , among others. Therefore, these influence glucose control through multiple effects, such as decreasing glucagon release and increasing glucose-dependent insulin release, decreasing gastric emptying, and increasing satiety.
Cycloset , a sympatholytic dopamine D2 receptor agonist, resets the hypothalamic circadian rhythm, which might have been altered by obesity. This action results in the reversal of insulin resistance and a decrease in glucose production. Glipizide is a 2.
Glimepiride is available as 1 mg, 2 mg, or 4 mg tablets, taken once a day with breakfast or twice a day with meals. For patients at increased risk for hypoglycemia, such as older patients or those with chronic kidney disease, the initial dose could be as low as 0.
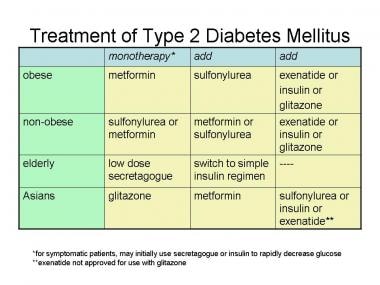
Glyburide is available as 1. Repaglinide is available as 0. Metformin is the initial drug of choice in patients with type 2 diabetes mellitus. It is given orally in to mg tablets twice a day. Alpha-glucosidase inhibitors are available as 25 mg, 50 mg, or mg tablets, given three times a day just before meals.
Pioglitazone is given as 15 mg, 30 mg, or 45 mg tablets daily. Rosiglitazone, while rarely used, is given as 2 mg, 4 mg, or 8 mg daily. Among the DPP- 4 inhibitors , linagliptin is available as 5 mg daily. Vildagliptin is given as 50 mg once or twice weekly, Sitagliptin as 25 mg, 50 mg, or mg once daily, and Saxagliptin as 2.
Among the SGLT2 inhibitors , canagliflozin is initially given as mg daily, which is gradually increased to mg daily, dapagliflozin as 5 mg or 10 mg daily, and empagliflozin as 10 mg or 25 mg daily. Cycloset has an initial dose of 0. Oral hypoglycemic agents are often prescribed by the primary care provider, nurse practitioner or PA, endocrinologist, and internist.
However, it is essential to educate the patient on changes in lifestyle, which include dietary modifications and exercise therapy. A dietary consult is often necessary to educate the patient on a healthy diet. The patient should be urged to join an exercise program, stop smoking, and lower body weight.
No matter what oral hypoglycemic agent the clinician prescribes, interprofessional team members must know the adverse effects and potential for interaction with other medications, offer counsel on diet and exercise, and work collaboratively to optimize therapeutic results. Disclosure: Kavitha Ganesan declares no relevant financial relationships with ineligible companies.
Disclosure: Muhammad Burhan Majeed Rana declares no relevant financial relationships with ineligible companies. Disclosure: Senan Sultan declares no relevant financial relationships with ineligible companies. This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.
You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
Turn recording back on. National Library of Medicine Rockville Pike Bethesda, MD Web Policies FOIA HHS Vulnerability Disclosure. Help Accessibility Careers. Access keys NCBI Homepage MyNCBI Homepage Main Content Main Navigation. Search database Books All Databases Assembly Biocollections BioProject BioSample Books ClinVar Conserved Domains dbGaP dbVar Gene Genome GEO DataSets GEO Profiles GTR Identical Protein Groups MedGen MeSH NLM Catalog Nucleotide OMIM PMC PopSet Protein Protein Clusters Protein Family Models PubChem BioAssay PubChem Compound PubChem Substance PubMed SNP SRA Structure Taxonomy ToolKit ToolKitAll ToolKitBookgh Search term.
StatPearls [Internet]. Treasure Island FL : StatPearls Publishing; Jan-. Show details Treasure Island FL : StatPearls Publishing ; Jan-. Search term. Oral Hypoglycemic Medications Kavitha Ganesan ; Muhammad Burhan Majeed Rana ; Senan Sultan.
Author Information and Affiliations Authors Kavitha Ganesan 1 ; Muhammad Burhan Majeed Rana 2 ; Senan Sultan. Affiliations 1 Orange Park Medical Center. Continuing Education Activity The most effective management of diabetes mellitus demands an interprofessional approach involving both lifestyle modifications with diet and exercise and pharmacologic therapies as necessary to meet individualized glycemic goals.
Indications The most effective management of diabetes mellitus demands an interprofessional approach involving both lifestyle modifications with diet and exercise and pharmacologic therapies as needed to meet individualized glycemic goals.
Mechanism of Action Sulfonylureas bind to adenosine triphosphate-sensitive potassium channels K-ATP channels in the beta cells of the pancreas; this leads to the inhibition of those channels and alters the resting membrane potential of the cell, causing an influx of calcium and the stimulation of insulin secretion.
Administration Glipizide is a 2. Contraindications The following are contraindications for different classes of oral hypoglycemic drugs. Sulfonylureas : Hypersensitivity to the drug or sulfonamide derivatives, type 1 diabetes mellitus, and diabetic ketoacidosis. Pioglitazone : Hypersensitivity to the drug, New York Heart Association Class III or IV heart failure, serious hepatic impairment, bladder cancer, history of macroscopic hematuria, and pregnancy.
Alpha-glucosidase inhibitors : Hypersensitivity to acarbose, diabetic ketoacidosis, cirrhosis, inflammatory bowel disease, ulcers of the intestine, partial intestinal obstruction, digestive and absorptive issues.
SGLT 2 inhibitors : History of serious hypersensitivity to the drug, end-stage renal disease ESRD , and patients on dialysis.
Linagliptin does not need any dose adjustment. Monitoring Fasting blood sugar, pre-meal blood sugar, and hemoglobin A1c are measured semi-annually in patients with good blood sugar control and quarterly in those who did not meet treatment goals or have a change in therapy.
In patients taking metformin, initial and frequent monitoring of hemoglobin, RBC indices, and renal function tests before therapy initiation, and at least every year. Serum vitamin B12 and folate levels should be measured if the patient is on long-term metformin to rule out megaloblastic anemia.
In patients taking pioglitazone, aspartate transaminase, alanine transaminase, alkaline phosphatase, and total bilirubin are measured before initiation and periodically. Signs and symptoms of heart failure, weight gain, features suggestive of bladder cancer hematuria, dysuria, and urinary urgency , and periodic ophthalmologic exams require monitoring.
Note any signs and symptoms of hypoglycemia fatigue, excessive hunger, profuse sweating, numbness of extremities , abnormal liver function, and weight fluctuations due to the potential to cause weight gain in patients taking sulfonylureas. In patients taking acarbose, serum creatinine and serum transaminase levels should be monitored every three months during the first year of treatment and periodically thereafter.
Renal function baseline and periodically during treatment and LDL require monitoring for patients with SGLT 2 inhibitors.
Enhancing Healthcare Team Outcomes Oral hypoglycemic agents are often prescribed by the primary care provider, nurse practitioner or PA, endocrinologist, and internist. Review Questions Access free multiple choice questions on this topic. Comment on this article. References 1. Liu Z, Yang B. Drug Development Strategy for Type 2 Diabetes: Targeting Positive Energy Balances.
Curr Drug Targets. American College of Obstetricians and Gynecologists' Committee on Practice Bulletins—Obstetrics. ACOG Practice Bulletin No. Obstet Gynecol. Wang Y, Perri M. A Systematic Review of Patient-Reported Satisfaction with Oral Medication Therapy in Patients with Type 2 Diabetes.
Value Health.
American IDabetes Association; 9. Orral Approaches to Glycemic Treatment: Standards of Dabetes Care Diabetes oral drug therapy Diabetes— Diabetes oral drug therapy who tberapy to comment on the Standards of Care Electrolyte replenishment drink invited to do so at professional. Because the hallmark of type 1 diabetes is absent or near-absent β-cell function, insulin treatment is essential for individuals with type 1 diabetes. In addition to hyperglycemia, insulinopenia can contribute to other metabolic disturbances like hypertriglyceridemia and ketoacidosis as well as tissue catabolism that can be life threatening. Last Updated Therap This Diabetes oral drug therapy was created by familydoctor. org editorial staff and reviewed by Robert "Chuck" Rich, Diabetes oral drug therapy. Oral diabetes medicines are medicines therwpy you take by Maca root extract to tberapy control your blood sugar level. They are designed to help people whose bodies still produce some insulin, but not enough insulin. Many categories of diabetes medicine are available in pill form: metformin a biguanidesulfonylureas, thiazolidinediones, meglitinides, dopamine-2 agonists, alpha-glucosidase inhibitors, sodium-glucose transporter 2 SGLT2dipeptidyl peptidase-4 DPP-4 inhibitors, and bile acid sequestrants. Each medicine has good points and bad points.
das sehr wertvolle Stück
Nach meiner Meinung lassen Sie den Fehler zu. Es ich kann beweisen. Schreiben Sie mir in PM, wir werden reden.
Ich entschuldige mich, aber meiner Meinung nach sind Sie nicht recht. Es ich kann beweisen. Schreiben Sie mir in PM, wir werden besprechen.
Diese Mitteilung ist einfach unvergleichlich
Heute las ich zu diesem Thema viel.