Energy balance and fat loss -
The exact success rate in treating obesity is difficult to identify and depends on definitions of success. Although we have a great deal of research about factors that contribute to weight loss, we have surprisingly little research to understand the factors that contribute to weight loss maintenance.
We study weight loss maintenance using our rodent model of dietary obesity and using information from the National Weight Control Registry NWCR.
In , Dr. Rena Wing and I started the NWCR to recruit and study a group of people who had succeeded at long-term weight loss maintenance. Individuals are eligible to enter the NWCR if they have maintained a weight loss of at least 30 pounds for at least 1 yr.
Individuals self-report their weight loss to enter the NWCR and provide information to us, largely, by completing questionnaires about weight loss and weight loss maintenance. Currently, we are following over individuals in the NWCR. These individuals are maintaining an average weight loss of over 70 pounds for an average period of almost 6 yr.
Over the past decade, we have described characteristics of these successful weight loss maintainers 59 , 74 — Although this is not a prospective study of weight loss maintenance, we have identified many common characteristics of these individuals that provide interesting hypotheses about successful weight loss maintenance.
We have found surprisingly few similarities in how NWCR participants report losing their weight. Conversely, many similarities are seen in the behaviors and strategies used to maintain weight loss. The four that stand out are: Eating a moderately low-fat, high-carbohydrate diet.
This is consistent with our previous work suggesting that low-fat diets should be better than high-fat diets in preventing positive energy balance.
Consistent self-monitoring of body weight, food intake, and physical activity. NWCR participants continue to periodically keep diet and physical activity records. This is consistent with other reports that self-monitoring facilitates long-term success in weight management Eating breakfast every day.
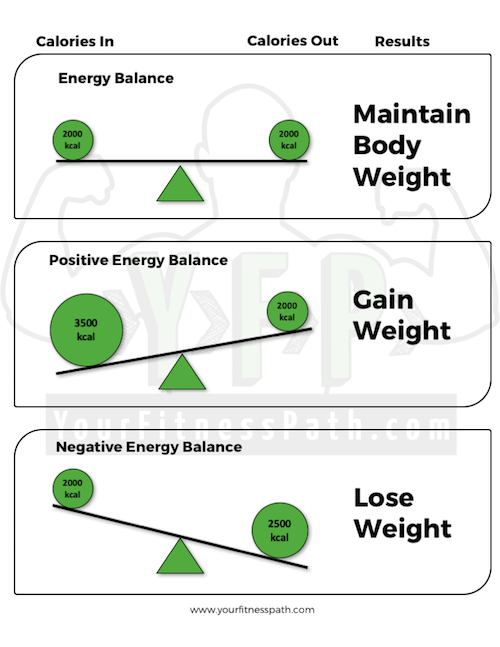
This is consistent with a growing body of data showing that eating breakfast facilitates maintenance of a healthy body weight Very high levels of physical activity. Others have reported that high levels of physical activity are important for long-term weight loss maintenance 80 — Weight loss is about negative energy balance, and there are many ways to produce this.
Negative energy balance is a temporary state that cannot be easily maintained for long periods of time. Weight loss maintenance is about achieving energy balance, but at a new lower body weight.
It requires diet and physical activity patterns that can be maintained indefinitely. The challenge is not just achieving energy balance, but achieving it at a lower body weight. This is a challenge because energy requirements decline with weight loss. Holly Wyatt and I developed the concept of the energy gap in an attempt to individualize strategies for weight loss maintenance Fig.
The energy gap is the difference between energy requirements before and after weight loss RMR decreases with decreasing body mass. The thermic effect of food decreases with total energy intake.
The energy cost of physical activity is related to body mass and declines with weight loss. Although there is a debate about whether the drop in energy requirements might actually be larger than expected from the loss of body weight 85 , it is clear that energy expenditure is lower after weight loss than before, and this presents a challenge in achieving energy balance after weight loss.
Most people do not distinguish between weight loss and weight loss maintenance. They try to achieve energy balance after weight loss by maintaining their lower energy intake. A typical energy gap for a weight loss of 40 pounds would be — kcal.
There are two ways to address the energy gap—reduce energy intake or increase physical activity. It is not difficult to maintain this amount of food restriction temporarily, but the challenge is doing it permanently.
Food restriction can be an effective temporary strategy, but it is rarely an effective long-term strategy for many people. It is opposed by our biology that stimulates us to eat 86 and is, perhaps, accompanied by other metabolic changes that we identified in our weight-reduced animal model 15 — Similarly, food restriction is vigorously opposed by an environment that encourages eating.
It is no surprise that few people can consistently fight their biology and their environment to sustain energy restriction. When they fail, they rapidly regain their weight, just like our weight-reduced rats.
The second way of addressing the energy gap is to increase physical activity. There are several advantages to this strategy. Presumably, intake before weight loss was at a level that could be maintained long term.
It is certainly possible that an individual may combine strategies to address the energy gap by reducing energy intake some and increasing energy expenditure some more. We believe that those who rely more on increasing physical activity than food restriction to address the energy gap will be more successful in long-term weight loss maintenance.
In addition to allowing a higher energy intake during weight loss maintenance, there are at least two other ways that high levels of physical activity may facilitate weight loss maintenance. First, high levels of physical activity may compensate for changes in metabolism caused by established obesity.
If obesity affects humans in the way it affects rats, weight-reduced humans may have a strong metabolic drive to regain weight. We have examined possible metabolic effects of obesity in individuals in the NWCR.
We find that RMR in NWCR participants is not different than lean or obese controls However, RMR was measured while they were performing their usual daily physical activity regimen and might be lower if measured under chronic sedentary conditions. As another example, we find one of the metabolic characteristics of weight-reduced rats that may predispose them to weight regain is a lower than anticipated leptin level 15 — A recent study suggested that giving leptin to weight-reduced humans may be more effective to prevent weight gain than to produce weight loss A second way that physical activity may help with weight loss maintenance is by maintaining a high energy flux.
Weight loss produces a decline in energy requirements, and achieving energy balance by food restriction results in achieving energy balance at a lower flux. By increasing physical activity, energy flux can continue to be maintained at a high level, which may be where biological regulatory systems are most sensitive.
An important question is whether it is any easier for people to maintain an increase in physical activity of — kcal than it is for them to maintain an energy restriction of the same amount. In truth, it is difficult to produce and maintain increases in physical activity in most people. We still have to find better ways to get people to increase physical activity, but the available data suggest that this strategy has a greater potential for success than energy restriction.
Similarly, increasing physical activity is the only strategy found at least partially to prevent weight regain in our weight-reduced animal model Other strategies such as drugs or surgery may partially fill the energy gap. For example, a drug that reduces hunger or increases energy expenditure would help fill the energy gap and require less voluntary food restriction or intentional increase in physical activity.
In summary, the challenge for obesity treatment is not losing weight but keeping it off. There are many ways to produce weight loss, but permanent weight loss maintenance may require a very high level of physical activity. An alternative strategy to obesity treatment is prevention of excessive weight gain.
This strategy does not require producing negative energy balance but rather only requires preventing positive energy balance. This strategy would represent a very long-term approach to addressing the obesity epidemic and is based on the notion that it is easier and more feasible to prevent weight gain than to produce and maintain substantial weight loss.
The first goal with this strategy would be to stop obesity rates from increasing, and gradually, over generations, to reduce levels to those seen before We provided a theoretical basis for this strategy in our second Science paper We estimated the degree of positive energy balance that is producing the gradual weight gain of the population.
Brown et al. If the gradual weight gain of the population is due to a small degree of positive energy balance, it should be possible to stop it with a small changes strategy that involves small decreases in energy intake and small increases in energy expenditure.
Such a strategy makes sense from an energy balance point of view. Making small decreases in energy intake would serve to reduce the positive energy balance, not produce negative energy balance. This should not produce strong biological compensatory decreases in energy intake of the kind that are seen with substantial food restriction.
Similarly, there is no evidence that small increases in physical activity produce compensatory increases in energy intake in relatively sedentary individuals Although we do not have definitive data to show that small behavior changes are more likely to be sustainable than larger ones for most people, this is a reasonable hypothesis.
We have a lot of data to suggest that large behavior changes are not sustainable for most people, as evidenced by the failure in obesity treatment.
Finally, small behavior changes may be less opposed by the environment than larger ones. Since the publication of our paper in , we have been gratified to see the acceptance of the small changes approach.
The Department of Health and Human Services, under Secretary Tommy Thompson, launched a small steps program aimed at making small changes in diet and physical activity The idea of approaching obesity through small lifestyle changes was also part of the Dietary Guidelines for Americans A national nonprofit initiative, America On the Move, was created to promote the small changes approach to prevention of weight gain It seems that the public health community is giving serious consideration to a strategy that involves prevention of weight gain to address obesity.
We recommended the use of inexpensive step counters or pedometers to allow people to set goals and monitor progress for increased walking. We estimated that most adults could increase energy expenditure with an extra steps per day, which is equivalent to walking an additional mile. Because an average walking speed would be — steps per minute, this could be done in 15—20 min, and the increase could be spread throughout the day.
Since then, the use of pedometers to promote physical activity has greatly increased. We have conducted some population surveys to obtain normative data on walking and its relationship to obesity. Table 1 shows these results. The average number of steps taken by adults in the United States daily is for men and for women.
Adults in Colorado 94 take more steps than the national average and have lower obesity rates , whereas adults in Tennessee take fewer steps per day and have higher obesity rates. Our recent work has focused on demonstrating the feasibility of the small changes approach in preventing excessive weight gain.
We have demonstrated that providing a goal of walking an extra steps per day is achievable and results in a significant increase in total walking Finally, we have conducted two intervention studies in families to demonstrate that the small changes approach can reduce excessive weight gain in overweight children and their parents 97 , Regardless of whether one advocates obesity treatment or prevention of weight gain as a strategy to reverse the obesity epidemic, it will be necessary to address environmental changes.
A big question is how much environmental change is needed? It is important to realize that at some level we intentionally created the environment that is making us fat and we are not unhappy with it.
The hope is that the small changes approach will work with modifying the environment. Rather than just focus on changing one or two environmental factors, it may be more useful to make small changes in a lot of factors. There are some hopeful signs of change.
Many food companies are working to develop and designate healthier items. The school food environment is improving with the agreement crafted by the Alliance for a Healthier Generation 99 with the soft drink manufacturers to remove soft drinks from schools.
Communities are looking at how they can facilitate walking over driving. We certainly have a long way to go in addressing the environment, but such efforts are beginning.
An advantage of the small changes approach to environmental change is that it provides an opportunity for all sectors of society to change gradually. It is certainly possible that systemic changes in the food supply such as promoting healthier foods and making them more affordable and in the systems that promote physical activity i.
can be made. It is also unclear how quickly such changes could be made or whether they would be effective. The environment did not get this way overnight, and small changes may be more acceptable than big ones in changing it. Although there is some sense of urgency in addressing the environment, small changes in a lot of environmental factors could make an immediate difference in at least stopping any further increase of obesity rates.
Experts debate the role of the environment vs. the role of personal responsibility in addressing obesity. It is certainly possible in our current environment for people to choose to eat a healthy diet and to engage in regular physical activity. However, in an environment where high-energy dense foods are readily available and vigorously marketed, and where physical activity is not necessary for most people to get through their daily lives, it is hard to maintain a healthy lifestyle.
For these reasons, we cannot approach obesity solely as an issue of personal responsibility. If we can change the environment to one that less strongly promotes obesity, it is likely that more people will be able to achieve and maintain healthy lifestyles.
On the other hand, we are not likely to be able to change the environment to one where most people can maintain a healthy body weight with little conscious effort. This means that we have to address obesity both as an environmental issue and as an issue of personal responsibility.
Maintaining a fair balance in doing this will be difficult. The issue of personal responsibility is even more sensitive in children, who may lack the knowledge and skills to make appropriate lifestyle choices and may not necessarily have the opportunity to engage in a healthy lifestyle.
For this group, it is critically important to create an environment that promotes healthier lifestyle choices. However, it is also important for us to help our children develop skills for making lifestyle choices that will help them maintain a healthier weight as adults.
The future does not look optimistic in terms of addressing obesity unless we can come together as a society to address behavior and environmental change. The high rates of childhood obesity that exist today suggest that obesity rates in the United States have not peaked and will continue to increase gradually if we do nothing.
Most overweight children become overweight or obese adults. The worst case scenario is that the entire population becomes obese, and the best case scenario is that we get serious about intervening to reverse the obesity epidemic.
However, we have to do this together as a society; if we remain as individuals struggling with the problem, environmental change will not likely occur. Is there real hope that we can make progress in reversing obesity before we all become obese? The more we learn about our complex system of regulating energy balance, the more we learn that it is operating as it has always operated.
Similarly, I am convinced that better behavior modification techniques alone will not solve the problem. The major influence toward positive energy balance is coming from the environment. It is operating through behavior and does not elicit strong biological opposition.
Put simply, we have a mismatch between our biology and our environment. We cannot attribute the obesity epidemic to abnormal biology or to a sudden rash of bad behavior.
We have to get serious about focusing attention on the environment. We are not likely to change the environment to one that existed before , where it was easier to maintain a healthy lifestyle. To get back to the obesity rates that existed then, individuals are going to have to make a greater conscious effort to manage their weight than they did then.
This does not mean that biological and behavioral research is not important—it is critically important. We still have much to learn about the biological regulation of energy balance and must improve our ability to help people make behavior changes.
However, without devoting at least similar attention toward the environment, we will not succeed in reversing the obesity epidemic. Obesity cannot be addressed solely in the clinic or in the school or in the workplace. It must be addressed everywhere.
We are really talking about social change to make our communities into places where it is easy to make good food choices and to be physically active. This change can only come from within communities and can only happen if every sector of the community engages in the effort.
The good news is that if every member of each sector of the community commits to making small changes, the result can be a big change.
It will not be easy, but we have dealt with other hard social issues such as tobacco smoking, recycling, and seat belt use. It can be done, but it needs to be done quickly. I believe that our best chance of reversing the obesity epidemic is in creating a social change movement focused on small changes—in behavior and in the environment.
The small changes approach allows everyone to play a role in addressing obesity. Our immediate challenge is to first stop the continued increase in the weight of the population, and over time, return obesity rates to pres levels.
I thank the many people who have worked in my laboratory over the past 25 yr. In particular, I thank Drs. John C. Peters, Holly R.
Wyatt, and Paul MacLean for their friendship and collaboration and for reviewing this paper. I gratefully acknowledge support from the National Institute of Diabetes and Digestive and Kidney Diseases over the past 25 yr. National Health and Nutrition Examination Survey , current version.
htm accessed July 10, International Obesity Task Force web site. asp accessed July 10, Tarasuk V , Beaton GH The nature and individuality of within-subject variation in energy intake. Am J Clin Nutr 54 : — Google Scholar. Hill JO , Sparling PB , Shields TW , Heller PA Effect of exercise and food restriction on body composition and metabolic rate in obese women.
Am J Clin Nutr 46 : — Heyman MB , Young VR , Fuss P , Tsay R , Joseph L , Roberts SB Underfeeding and body weight regulation in normal-weight young men. Am J Physiol : R — R Diaz EO , Prentice AM , Goldberg GR , Murgatroyd PR , Coward WA Metabolic response to experimental overfeeding in lean and overweight healthy volunteers.
Am J Clin Nutr 56 : — Hill JO , Fried SK , DiGirolamo M Effects of a high-fat diet on energy intake and expenditure in rats. Life Sciences 33 : — Chang S , Graham B , Yakubu F , Lin D , Peters JC , Hill JO Metabolic differences between obesity prone and obesity resistant rats.
Abou Mrad J , Yakubu F , Lin D , Peters JC , Atkinson JB , Hill JO Skeletal muscle composition in dietary obese-susceptible and dietary obesity-resistant rats.
Pagliassotti MJ , Knobel SM , Shahrokhi KA , Manzo AM , Hill JO Time course of adaptation to a high-fat diet in obesity-resistant and obesity-prone rats. Pagliassotti MJ , Shahrokhi KA , Hill JO Skeletal muscle glucose metabolism in obesity-prone and obesity-resistant rats.
Pagliassotti MJ , Knobel SM , Shahrokhi KA , Monzo AM , Hill JO Time course of adaptation to a high fat diet in obesity-resistant and obesity-prone rats. Gayles EC , Pagliassotti MJ , Prach PA , Koppenhafer TA , Hill JO Contribution of energy intake and tissue enzymatic profile to body weight gain in high-fat-fed rats.
Hill JO , Dorton J , Sykes MN , DiGirolamo M Reversal of dietary obesity is influenced by its duration and severity. Int J Obes 13 : — MacLean PS , Higgins JA , Johnson GC , Fleming-Elder BK , Donahoo WT , Melanson EL , Hill JO Enhanced metabolic efficiency contributes to weight regain after weight loss in obesity-prone rats.
MacLean PS , Higgins J , Johnson GC , Fleming-Elder BK , Peters JC , Hill JO Metabolic adjustments with the development, treatment, and recurrence of obesity in obesity-prone rats. MacLean P , Higgins J , Jackman M , Johnson G , Fleming-Elder B , Wyatt H , Melanson EL , Hill JO Peripheral metabolic responses to prolonged weight reduction that promote rapid, efficient regain in obesity-prone rats.
Levin BE Arcuate NPY neurons and energy homeostasis in diet-induced obese and resistant rats. Levin BE Reduced norepinephrine turnover in organs and brains of obesity-prone rats.
Mayer J , Purnima R , Mitra KP Relation between caloric intake, body weight and physical work: studies in an industrial male population in West Bengal.
Am J Clin Nutr 4 : — Bell C , Day DS , Jones PP , Christou DD , Petitt DS , Osterberg K , Melby CL , Seals DR High energy flux mediates the tonically augmented β-adrenergic support of resting metabolic rate in habitually exercising older adults. J Clin Endocrinol Metab 89 : — Drewnowski A Energy density, palatability, and satiety: implications for weight control.
Nutr Rev 56 : — Hill JO , Peters JC Environmental contributions to the obesity epidemic. Science : — Heitmann BL , Lissner L , Osler M Do we eat less fat, or just report so? Int J Obes Rel Met Dis 24 : — Briefel RR , McDowell MA , Alaimo K , Caughman CR , Bischof AL , Carroll MD , Johnson CL Total energy intake of the US population: the third National Health and Nutrition Examination Survey, — Am J Clin Nutr 62 : S—S.
Ham SA , Yore MM , Fulton JE , Kohl HW Prevalence of no leisure-time physical activity: 35 states and the District of Columbia, — MMWR Morb Mortal Wkly Rep 53 : 82 — Sturm R The economics of physical activity: societal trends and rationales for interventions.
Am J Prev Med 27 : — Bassett DR , Schneider PL , Huntington GE Physical activity in an older order Amish community. Med Sci Sports Exerc 36 : 79 — Flatt JP Importance of nutrient balance in body weight regulation. Diabetes-Metab Rev 4 : — Golay A , Allaz AF , Morel Y , de Tonnac N , Tankova S , Reaven G Similar weight loss with low- or high-carbohydrate diets.
Am J Clin Nutr 63 : — Kinsell LW , Gunning B , Michaels GD , Richardson J , Cox SE , Lemon C Calories do count. Metabolism 13 : — Garrow JS Treat obesity seriously. London : Churchill Livingstone.
N Engl J Med : — Stern L , Iqbal N , Seshadri P , Chicano KL , Daily DA , McGrory J , Williams M , Gracely EJ , Samaha FF The effects of low carbohydrate versus conventional weight loss in severely obese adults: one year follow-up of a randomized trail.
Ann Intern Med : — Samaha FF , Iqbal N , Seshadri P , Chicano KL , Daily DA , McGrory J , Williams T , Williams M , Gracely EJ , Stern L A low carbohydrate as compared to a low fat diet in severe obesity.
Nordmann AJ , Nordmann A , Briel M , Keller U , Yancy WS Jr, Brehm BJ , Bucher HC Effects of low-carbohydrate vs low-fat diets on weight loss and cardiovascular risk factors: a meta-analysis of randomized controlled trials.
Arch Intern Med : — Astrup A , Ryan L , Grunwald GK , Storgaard M , Saris W , Melanson E , Hill JO The role of dietary fat in body fatness: evidence from a preliminary meta-analysis of ad libitum low-fat dietary intervention studies. Br J Nutr 83 : S25 — S Thomas CD , Peters JC , Reed GW , Abumrad NN , Sun M , Hill JO Nutrient balance and energy expenditure during ad libitum feeding of high-fat and high-carbohydrate diets in humans.
Am J Clin Nutr 55 : — Hill JO , Drougas H , Peters JO Obesity treatment: can diet composition play a role? Ann Int Med : — Horton TJ , Drougas H , Brachey A , Reed GW , Peters JC , Hill JO Fat and carbohydrate overfeeding in humans: different effects on energy storage.
Am J Clin Nutr 62 : 19 — Willett WC Is dietary fat a major determinant of body fat? Am J Clin Nutr 67 Suppl : S — S. Due A , Toubro S , Skov AR , Astrup AA Effect of normal-fat diets, either medium or high in protein, on body weight in overweight subjects: a randomised 1-year trial.
Int J Obes Relat Metab Disord 28 : — Ludwig DS Dietary glycemic index and obesity. J Nutr : S—S. Saltzman E The low glycemic index diet: not yet ready for prime time. Nutr Rev 57 : Stubbs RJ , Ritz P , Coward WA , Prentice AM Covert manipulation of the ratio of dietary fat to carbohydrate and energy density: effect on food intake and energy balance in free-living men eating ad libitum.
Am J Clin Nutr 62 : — Stubbs RJ , Harbron CG , Murgatroyd PR , Prentice AM Covert manipulation of dietary fat and energy density: effect on substrate flux and food intake in men eating ad libitum. Kral TVE , Roe LS , Rolls BJ Combined effects of energy density and portion size on energy intake in women.
Am J Clin Nutr 79 : — Kriehn J , Donahoo W , Dong F , Grunwald G , Hill JO The effect of dietary fat on energy intake over a typical range of fat consumption. Obes Res 12 Suppl : P.
Woods SC , Schwartz MW , Baskin DG , Seeley RJ Food intake and the regulation of body weight. Ann Rev Psych 51 : — Hill JO , Prentice AM Sugar and body weight regulation. DiMeglio DP , Mattes RD Liquid versus solid carbohydrate: effects on food intake and body weight. Int J Obes Relat Metab Disord 24 : — Hill JO , Melby C , Johnson SL , Peters JC Physical activity and energy requirements.
Hill JO , Commerford R Exercise, fat balance and energy balance. Int J Sports Nutr 6 : 80 — Di Pietro L , Dziura J , Blair SN Estimated change in physical activity levels PAL and prediction of 5-year weight change in men: the aerobics center longitudinal study.
French SA , Jeffery RW , Forster JL , McGovern PG , Kelder SH , Baxter JE Predictors of weight change over two years among a population of working adults: the Healthy Worker Project.
Int J Obes Relat Metab Disord 18 : — Hill JO , Wyatt HR Role of physical activity in preventing and treating obesity. J Appl Phyisol 99 : — Horton TJ , Hill JO Exercise and obesity.
Proc Nutr Soc 57 : 85 — Hill JO , Wyatt HR , Reed GW , Peters JC Obesity and the environment: Where do we go from here? Klem ML , Wing RR , McGuire MT , Seagle HM , Hill JO A descriptive study of individuals successful at long-term maintenance of substantial weight loss. Am J Clin Nutr 66 : — Hill JO , Davis JR , Tagliaferro AR Effects of diet and exercise training on thermogenesis in adult female rats.
Physiol Behav 31 : — Murgatroyd PR , Goldberg GR , Leahy FE , Gilsenan MB , Prentice AM Effects of inactivity and diet composition on human energy balance.
Int J Obes Relat Metab Disord 23 : — Brownell KD Public policy and the prevention of obesity. In: Fairburn CG , Brownell KD , eds. Eating disorders and obesity. New York : The Guilford Press ; — Hill JO , Pagliassotti MJ , Peters JC Nongenetic determinants of obesity and fat topography.
In: Bouchard C , ed. Genetic determinants of obesity. Boca Raton, FL : CRC Press, Inc. Bray GA , Nielsen SJ , Popkin BM Consumption of high-fructose corn syrup in beverages may play a role in the epidemic of obesity.
Hill JO , Wyatt HR , Peters JC Modifying the environment to reverse obesity. In: Goehl TJ, ed. Essays on the future of environmental health research.
Environmental Health Perspectives; : — Rossner S Factors determining the long-term outcome of obesity treatment. In: Bjorntorp P , Brodoff BN , eds. Philadelphia : J. Lippincott ; — Wing RR Physical activity in the treatment of the adulthood overweight and obesity: current evidence and research issues.
Med Sci Sports Exerc 31 Suppl : S — S Ross R , Dagnone D , Jones PJH , Smith H , Paddags A , Hudson R , Janssen I Reduction in obesity and related comorbid conditions after diet-induced weight loss or exercise-induced weight loss in men.
A randomized controlled trial. Ann Intern Med : 92 — Dansinger ML , Gleason JA , Griffith JL , Selker HP , Schaefer EJ Comparison of the Atkins, Ornish, Weight Watchers, and Zone diets for weight loss and heart disease risk reduction: a randomized trial.
JAMA : 43 — Wing RR , Wadden TA Treatment of obesity by moderate and severe caloric restriction in weight loss and control: results of clinical research trials. Blackburn GL Benefits of weight loss in the treatment of obesity. Am J Clin Nutr 69 : — Mertens IL , Van Gaal LF Overweight, obesity, and blood pressure: the effects of modest weight reduction.
Obes Res 8 : — McGuire MT , Wing RR , Hill JO The prevalence of weight loss maintenance among American adults. Int J Obes 23 : — Wing RR , Hill JO Successful weight loss maintenance.
Ann Rev Nutr 21 : — McGuire MT , Wing RR , Klem ML , Seagle HM , Hill JO Long-term maintenance of weight loss: do people who lose weight through various weight loss methods use different behaviors to maintain their weight? Int J Obes Relat Metab Disord 22 : — Shick SM , Wing RR , Klem ML , McGuire MT , Hill JO , Seagle HM Persons successful at long-term weight loss and maintenance continue to consume a low calorie, low fat diet.
J Am Diet Assoc 98 : — Wyatt HR , Grunwald GK , Seagle HM , Klem ML , McGuire MT , Wing RR , Hill JO Resting energy expenditure in reduced-obese subjects in the national weight control registry. Boutelle KN , Kirschenbaum Further support for consistent self-monitoring as a vital component of successful weight control.
Obes Res 6 : — Rampersaud GC , Pereira MA , Girard BL , Adams J , Metzl JD Breakfast habits, nutritional status, body weight and academic performance in children and adolescents.
J Am Diet Assoc : — Schoeller DA , Shay K , Kushner RF How much physical activity is needed to minimize weight gain in previously obese women? Jakicic JM , Winters C , Lang W , Wing RR Effects of intermittent exercise and use of home exercise equipment on adherence, weight loss and fitness in overweight women.
JAMA : — Weinsier WL , Hunter GR , Desmond RA , Byrne NM , Zuckerman PA , Darnell BE Free-living activity energy expenditure in women successful and unsuccessful at maintaining a normal body weight.
Am J Clin Nutr 75 : — J Am Diet Assoc 5 Suppl 1 : S63 — S Ravussin E , Lillioja S , Anderson TE , Christin L , Bogardus C Determinants of hour energy expenditure in man. Methods and results using a respiratory chamber. J Clin Invest 78 : — Leibel RL , Rosenbaum M , Hirsch J Changes in energy expenditure resulting from altered body weight.
Blundell JE , Gillett A Control of food intake in the obese. Obes Res 9 Suppl 4 : S — S. Rosenbaum M , Goldsmith R , Bloomfield D , Magnano A , Weimer L , Heymsfield S , Gallagher D , Mayer L , Murphy E , Leibel RL Low-dose leptin reverses skeletal muscle, autonomic, and neuroendocrine adaptations to maintenance of reduced weight.
J Clin Invest : — Lewis CE , Jacobs Jr DR , Kiefe CI , Schreiner PJ , Smith DE , Williams OD Weight gain continues in the s: year trends in weight and overweight from the CARDIA Study. Am J Epidemiol : — Brown WJ , Williams L , Ford JH , Ball K , Dobson AJ Identifying the energy gap: magnitude and determinants of 5-year weight gain in midage women.
Obes Res 13 : — Blundell JE , King NA Effects of exercise on appetite control: loose coupling between energy expenditure and energy intake. Int J Obes Relat Metab Disord 22 Suppl 2 : S22 — S Department of Health and Human Services Small Steps Program.
gov accessed July 16, Department of Health and Human Services Dietary Guidelines America On the Move. org accessed July 16, Wyatt HR , Peters JC , Reed GW , Barry M , Hill JO A Colorado statewide survey of walking and its relation to excessive weight.
Med Sci Sports Exerc 37 : — Wyatt HR , Peters JC , Reed GW , Grunwald GK , Barry M , Thompson H , Jones J , Hill JO Using electronic step counters to increase lifestyle physical activity: Colorado on the Move.
J Phys Act Health 1 : — Stroebele N , Stuht J , Catenacci V , Schroeder LR , Wyatt RH , de Castro JM , Hill JO , A small changes approach to reducing energy intake. Proc Annual Scientific Meeting of the North American Association for the Study of Obesity , Boston, MA , Abstract.
Google Preview. Rodearmel SJ , Wyatt HR , Barry MJ , Dong F , Pan D , Israel RG , Cho SS , McBurney MI , Hill JO A family-based approach to preventing excessive weight gain. Obesity 14 : — Rodearmel SJ , Grotz VL , Goldsmith LA , Smith SM , Stroebele N , Ogden LF , Wyatt HR , Moran JR , Hill JO , America on the Move family study: a family based approach for preventing excessive weight gain in children.
A loss of bacterial gene richness is linked to more severe metabolic syndrome, and less sensitivity to weight loss following caloric restriction diet [ 83 ].
Dietary habits also seem to be associated with microbiota richness [ 84 ]. The proposed mechanisms by which gut microbiota dysbiosis and loss of richness can promote obesity and insulin resistance are diverse, often derived from mouse models, and still deserve more studies and validation in humans.
Many factors have contributed to the increase in the prevalence of obesity in children including unhealthy dietary patterns with high consumption of fast foods and highly processed food [ 85 ], of sugar sweetened beverages [ 86 ], lack of PA, an increase in sedentary behaviors e.
Experiences during early life e. In particular, maternal gestational weight gain GWG [ 92 ], maternal overweight prior to pregnancy, smoking during pregnancy, high or low infant birth weight, rapid weight gain during the first year of life [ 93 — 95 ], early obesity rebound [ 96 ], breastfeeding patterns [ 97 ] and early introduction of complementary food [ 98 ] have all been linked to later excess adiposity.
Many of these are inter-related and work is ongoing to disentangle concurrent factors. In addition, high levels of stress during childhood and adolescence may change eating habits and augment consumption of highly palatable but nutrient-poor foods [ 99 ].
Numerous policy options to prevent obesity have been explored, and evidence is sufficient to conclude that many are cost effective. Given the multifactorial nature of obesity, as in other complex public health problems, a combination of interventions is more likely to generate better results than focusing only on a single measure [ ].
Gortmaker et al. They modeled the reach, costs and savings for the US population Some of these interventions excise tax on sugar-sweetened beverages, elimination of tax deduction for advertising unhealthy food to children and nutrition standards for food and beverages sold in schools outside of meals not only prevent many cases of childhood obesity, but also potentially cost less to implement than they would save for society.
The global childhood obesity epidemic demands a population-based multisector, multi-disciplinary, and culturally relevant approach. Children need protection from exploitative marketing and special efforts to support healthy eating, PA behaviors, and optimal body weight [ — ].
Adequate evidence has been accumulated that interventions, especially school-based programs, can be effective in preventing childhood obesity [ ]. Preventing obesity will require sustained efforts across all levels of government and civil society. Although there are individual differences in susceptibility, obesity is by large a societal problem resulting from health related behaviors that are largely driven by environmental upstream factors.
Many options for policies to prevent obesity are available and many of these are effective and cost-effective. Integrated management of the epidemic of obesity requires top-down government policies and bottom-up community approaches and involvement of many sectors of society.
Integrating evidence-based prevention and management of obesity is essential. There is convincing evidence for a role of obesity as a causal factor for many types of cancer including colorectum, endometrium, kidney, oesophagus, postmenopausal breast, gallbladder, pancreas, gastric cardia, liver, ovary, thyroid, meningioma, multiple myeloma, and advanced prostate cancers [ 19 ].
Recent progress on elucidating the mechanisms underlying the obesity-cancer connection suggests that obesity exerts pleomorphic effects on pathways related to tumor development and progression and, thus, there are potential opportunities for primary to tertiary prevention of obesity-related cancers.
We now know that obesity can impact well-established hallmarks of cancer such as genomic instability, angiogenesis, tumor invasion and metastasis and immune surveillance [ 20 ]. However, obesity-associated perturbations in systemic metabolism and inflammation, and the interactions of these perturbations with cancer cell energetics, are emerging as the primary drivers of obesity-associated cancer development and progression.
In both obesity and metabolic syndrome, alterations occur in circulating levels of insulin and insulin-like growth factors, sex hormones, adipokines, inflammatory factors, several chemokines, lipid mediators and vascular associated factors [ 21 — 23 ].
Most research on obesity and cancer has focused on Caucasians in HICs. While many of the identified risk factors in HICs will have the same physiologic effects in LMICs, the determinants may be different, in addition to other environmental and genetic differences across populations. Novel risk factors or traditional diets may be identified in newly studied populations and regions.
Diet is shaped by many factors such as traditions, knowledge about diet, food availability, food prices, cultural acceptance, and health conditions. Likewise, a variety of factors will influence daily physical activity and sedentary behaviors, including dwellings, urbanization, opportunities for safe transportation by bicycle riding and walking, recreational facilities, employment constraints and health conditions.
Surveillance of current diet and health conditions and assessment of trends over time is of major importance in LMICS. Further resources and research capacity are of highest priority. In addition to surveillance efforts, prospective studies able to document lifestyle and change of lifestyle over time are an important area of research.
Several cohort studies conducted in HICs have shown an impact of healthy dietary patterns on obesity [ ] and similar studies could be conducted in LMICs to identify dietary patterns related to weight gain and obesity in a variety of settings to evaluate the major lifestyle, behavioral and policy influences in an effort to plan public health interventions appropriately.
A major challenge is to capture life course exposures and identify windows of susceptibility. Cohort studies covering the whole life course, focusing on critical windows of exposure and the time course of exposure to disease birth cohorts, adolescent cohorts, and young adult cohorts , should be considered.
Of particular interest are multi-centered cohorts and inter-generational cohorts that would create resources to enable research on the interplay between genetics, lifestyle and the environment.
For example in the Avon longitudinal study of parents and children ALSPAC , increasing intake of energy-dense nutrient-poor foods during childhood mostly free sugar was associated with obesity development.
Diets with higher energy density were associated with increased fat mass [ ]. Most relevant to LMICs is the observation that children who were stunted in infancy and are subsequently exposed to more calories, at puberty, are more likely to have higher fat mass at the same BMI compared with children who were not stunted [ 93 , 94 , ].
Poor maternal prenatal dietary intakes of energy, protein and micronutrients have been associated with increased risk of adult obesity in offspring while a high protein diet during the first 2 years of life was also associated with increased obesity later in life [ ]; conversely, exclusive breastfeeding was associated with lower risk of obesity later in childhood, although this may not persist into adulthood [ ].
Similar results from a cohort study conducted in Mexico show that children exclusively or predominantly breastfed for 3 months or more had lower adiposity at 4 years [ ]. Further work on birth cohorts or other prospective studies in LMICs is likely to provide insights into the developmental causes of obesity and NCDs.
Input from local research communities, health ministries and policy makers and appropriate funding or resource assignment are critical for the success of new efforts in LMICs. There is clearly a need for capacity building and resources devoted to nutritional research in LMICs.
The first step would be a comprehensive assessment of resources already in place, and the identification of gaps and priorities for moving forward. Repeated surveillance surveys are essential in LMICs for evaluation of current and future status of the population and addressing undesirable trends with prevention and control programs.
It is recognized that few prospective studies are currently underway in LMICs and resources will be needed to pursue this important area of research.
Input from local research communities, health ministries and policy makers are critical for the success of new efforts in LMICs. The global epidemic of obesity and the double burden of malnutrition are both related to poor quality diet; therefore, improvement in diet quality can address both phenomena.
The benefits of a healthy diet on adiposity are likely mediated by effects of dietary quality on energy intake, which is the main driver of weight gain.
Energy balance is best assessed by changes in weight or in fat mass. Measures of energy intake and expenditure are not precise enough to capture small differences that are of individual and public health importance.
Dietary patterns characterized by higher intakes of fruits and vegetables, legumes, whole grains, nuts and seeds and unsaturated fat, and lower intakes of refined starch, red meat, trans and saturated fat, and sugar-sweetened foods and beverages, consistent with a traditional Mediterranean diet and other measures of dietary quality, can contribute to long-term weight control.
Genetic factors cannot explain the global epidemic of obesity. It is possible that factors such as genetic, epigenetic and the microbiota can influence individual responses to diet and physical activity. Very few gene—diet interactions or diet-microbiota have been established in relation to obesity and effects on cancer risk.
Short-term studies have not provided clear benefit of physical activity for weight control, but meta-analysis of longer term trials indicates a modest benefit on body weight loss and maintenance.
The combination of aerobic and resistance training seems to be optimal. Long-term epidemiologic studies also support modest benefits of physical activity on body weight. This includes benefits of walking and bicycle riding, which can be incorporated into daily life and be sustainable for the whole population.
Physical activity also has important benefit on health outcomes independent of its effect on body weight. In addition, long-term epidemiologic studies show that sedentary behavior in particular TV viewing is related to increased risk of obesity, suggesting that limiting sedentary time has potential for prevention of weight gain.
The major drivers of the obesity epidemic are the food environment, marketing of unhealthy foods and beverages, urbanization, and probably reduction in physical activity.
Existing evidence on the relations of diet, physical activity and socio-economic and cultural factors to body weight is largely from HICs. There is an important lack of data on diet, physical activity and adiposity in most parts of the world and this information should to be collected in a standardized manner when possible.
In most environments, 24h recalls will be the more suitable method for dietary surveillance. Attention should be given to data in subgroups because mean values may obscure important disparities.
In utero and early childhood, environment has important implications for lifetime adiposity. This offers important windows of opportunity for intervention. Observational data on determinants of body weight and intervention trials across the life course to improve body weight are also required.
To accomplish these goals, there is a need for resources to build capacity and conduct translational research. Gaining control of the obesity epidemic will require the engagement of many sectors including education, healthcare, the media, worksites, agriculture, the food industry, urban planning, transportation, parks and recreation, and governments from local to national.
This provides the opportunity for all individuals to participate in this effort, whether at home or in establishing high-level policy. We now have evidence that intensive multi-sector efforts can arrest and partially reverse the rise of obesity in particular among children.
In conclusion, we are gaining understanding on the determinants of energy balance and obesity and some of these findings are being translated into public health policy changes. However, further research and more action from policy makers are needed. Samuel J. Fernanda Morales-Berstein, Carine Biessy, … on behalf of the EPIC Network.
Anderson AS, Key TJ, Norat T, Scoccianti C, Cecchini M, Berrino F et al. European code against cancer 4th edition: obesity, body fatness and cancer. Cancer Epidemiol. World Health Organization Global status report on noncommunicable diseases: World Health Organization, Geneva.
AICR, Washington DC. Google Scholar. Food, nutrition, and physical activity: a global perspective. Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C et al Global, regional, and national prevalence of overweight and obesity in children and adults during — a systematic analysis for the Global Burden of Disease Study Lancet — Article PubMed PubMed Central Google Scholar.
de Onis M, Blossner M, Borghi E Global prevalence and trends of overweight and obesity among preschool children.
Am J Clin Nutr 92 5 — Article PubMed Google Scholar. Lobstein T, Jackson-Leach R, Moodie ML, Hall KD, Gortmaker SL, Swinburn BA et al Child and adolescent obesity: part of a bigger picture. Wabitsch M, Moss A, Kromeyer-Hauschild K Unexpected plateauing of childhood obesity rates in developed countries.
BMC Med Wang YF, Baker JL, Hil JO, Dietz WH Controversies regarding reported trends: has the obesity epidemic leveled off in the United States? Adv Nutr 3 5 — Levels and trends in child malnutrition UNICEF—WHO—World Bank Group joint child malnutrition estimates: key findings of the edition Shrimpton R, Rokx C The double burden of malnutrition : a review of global evidence.
Health, Nutrition and Population HNP discussion paper. World Bank, Washington DC. Darnton-Hill I, Nishida C, James WP A life course approach to diet, nutrition and the prevention of chronic diseases.
Public Health Nutr 7 1a — Article CAS PubMed Google Scholar. James P et al Ending malnutrition by an agenda for change in the Millennium. UN SCN, Geneva. Moubarac JC, Martins AP, Claro RM, Levy RB, Cannon G, Monteiro CA Consumption of ultra-processed foods and likely impact on human health.
Evidence from Canada. Public Health Nutr 16 12 — Monteiro CA, Levy RB, Claro RM, de Castro IR, Cannon G Increasing consumption of ultra-processed foods and likely impact on human health: evidence from Brazil.
Public Health Nutr 14 1 :5— Baker P, Friel S Processed foods and the nutrition transition: evidence from Asia. Obes Rev 15 7 — Barquera S, Pedroza-Tobias A, Medina C Cardiovascular diseases in mega-countries: the challenges of the nutrition, physical activity and epidemiologic transitions, and the double burden of disease.
Curr Opin Lipidol 27 4 — Article CAS PubMed PubMed Central Google Scholar. International Food Policy Research Institute Global nutrition report actions and accountability to advance nutrition and sustainable development.
Washington, DC. Lauby-Secretan B, Scoccianti C, Loomis D, Grosse Y, Bianchini F, Straif K et al Body fatness and cancer—viewpoint of the IARC Working Group.
N Engl J Med 8 — Hanahan D, Weinberg RA Hallmarks of cancer: the next generation. Cell 5 — Bonomini F, Rodella LF, Rezzani R Metabolic syndrome, aging and involvement of oxidative stress.
Aging disease 6 2 — Hursting SD, Berger NA Energy balance, host-related factors, and cancer progression. J Clin Oncol 28 26 — Renehan AG, Roberts DL, Dive C Obesity and cancer: pathophysiological and biological mechanisms.
Arch Physiol Biochem 1 — Sun Q, van Dam RM, Spiegelman D, Heymsfield SB, Willett WC, Hu FB Comparison of dual-energy X-ray absorptiometric and anthropometric measures of adiposity in relation to adiposity-related biologic factors.
Am J Epidemiol 12 — World Health Organization Waist circumference and waist-hip ratio: a report of a WHO expert consultation. van der Kooy K, Leenen R, Seidell JC, Deurenberg P, Droop A, Bakker CJ Waist-hip ratio is a poor predictor of changes in visceral fat.
Am J Clin Nutr 57 3 — PubMed Google Scholar. Willett W. Implications of total energy intake for epidemiologic analyses. Nutritional epidemiology. Oxford University Press, New York, pp — Heymsfield SB, Lohman TG, Wang Z, Going SB Human body composition.
McCrory MA, Gomez TD, Bernauer EM, Mole PA Evaluation of a new air displacement plethysmograph for measuring human body composition. Med Sci Sports Exerc 27 12 — Glickman SG, Marn CS, Supiano MA, Dengel DR Validity and reliability of dual-energy X-ray absorptiometry for the assessment of abdominal adiposity.
J Appl Physiol 97 2 — Article Google Scholar. Bandera EV, Maskarinec G, Romieu I, John EM Racial and ethnic disparities in the impact of obesity on breast cancer risk and survival: a global perspective.
Adv Nutr 6 6 — Scientific Advisory Committee on Nutrition Dietary reference values for energy. The Stationery Office, London. Hall KD, Sacks G, Chandramohan D, Chow CC, Wang YC, Gortmaker SL et al Quantification of the effect of energy imbalance on bodyweight. Healy GN, Wijndaele K, Dunstan DW, Shaw JE, Salmon J, Zimmet PZ et al Objectively measured sedentary time, physical activity, and metabolic risk: the Australian Diabetes, Obesity and Lifestyle Study AusDiab.
Diabetes Care 31 2 — Romero-Corral A, Somers VK, Sierra-Johnson J, Thomas RJ, Collazo-Clavell ML, Korinek J et al Accuracy of body mass index in diagnosing obesity in the adult general population. Int J Obes Lond 32 6 — Article CAS Google Scholar. Ello-Martin JA, Ledikwe JH, Rolls BJ The influence of food portion size and energy density on energy intake: implications for weight management.
Am J Clin Nutr 82 1 Suppl S— S. Prentice AM Manipulation of dietary fat and energy density and subsequent effects on substrate flux and food intake. Am J Clin Nutr 67 3 Suppl S— S. Fogelholm M, Anderssen S, Gunnarsdottir I, Lahti-Koski M Dietary macronutrients and food consumption as determinants of long-term weight change in adult populations: a systematic literature review.
Food Nutr Res Salas-Salvado J, Bullo M, Babio N, Martinez-Gonzalez MA, Ibarrola-Jurado N, Basora J et al Reduction in the incidence of type 2 diabetes with the Mediterranean diet: results of the PREDIMED-Reus nutrition intervention randomized trial. Diabetes Care 34 1 — Jaworowska A, Blackham T, Davies IG, Stevenson L Nutritional challenges and health implications of takeaway and fast food.
Nutr Rev 71 5 — Schroder H, Fito M, Covas MI Association of fast food consumption with energy intake, diet quality, body mass index and the risk of obesity in a representative Mediterranean population.
Br J Nutr 98 6 — Pereira MA, Kartashov AI, Ebbeling CB, Van Horn L, Slattery ML, Jacobs DR Jr. Alkerwi A, Crichton GE, Hebert JR Consumption of ready-made meals and increased risk of obesity: findings from the observation of cardiovascular risk factors in Luxembourg ORISCAV-LUX study.
Br J Nutr 1—8. Kant AK, Whitley MI, Graubard BI Away from home meals: associations with biomarkers of chronic disease and dietary intake in American adults, NHANES — Int J Obes Lond 39 5 — Chajes V, Biessy C, Ferrari P, Romieu I, Freisling H, Huybrechts I et al Plasma elaidic acid level as biomarker of industrial trans fatty acids and risk of weight change: report from the EPIC study.
PloS one 10 2 :e Han E, Powell LM Consumption patterns of sugar-sweetened beverages in the United States. J Acad Nutr Dietetics 1 — Basu S, McKee M, Galea G, Stuckler D Relationship of soft drink consumption to global overweight, obesity, and diabetes: a cross-national analysis of 75 countries.
Am J Public Health 11 — Malik VS, Pan A, Willett WC, Hu FB Sugar-sweetened beverages and weight gain in children and adults: a systematic review and meta-analysis.
Am J Clin Nutr 98 4 — Te Morenga L, Mallard S, Mann J Dietary sugars and body weight: systematic review and meta-analyses of randomised controlled trials and cohort studies. BMJ e Rouhani MH, Salehi-Abargouei A, Surkan PJ, Azadbakht L Is there a relationship between red or processed meat intake and obesity?
A systematic review and meta-analysis of observational studies. Obes Rev 15 9 — Fung TT, Pan A, Hou T, Chiuve SE, Tobias DK, Mozaffarian D et al Long-term change in diet quality is associated with body weight change in men and women.
J Nutr 8 — Romaguera D, Norat T, Vergnaud AC, Mouw T, May AM, Agudo A et al Mediterranean dietary patterns and prospective weight change in participants of the EPIC-PANACEA project. Am J Clin Nutr 92 4 — Funtikova AN, Benitez-Arciniega AA, Gomez SF, Fito M, Elosua R, Schroder H Mediterranean diet impact on changes in abdominal fat and year incidence of abdominal obesity in a Spanish population.
Br J Nutr 8 — Buckland G, Bach A, Serra-Majem L Obesity and the Mediterranean diet: a systematic review of observational and intervention studies. Obes Rev Off J Int Assoc Study Obes 9 6 — Richter LM, Victora CG, Hallal PC, Adair LS, Bhargava SK, Fall CH et al Cohort profile: the consortium of health-orientated research in transitioning societies.
Int J Epidemiol 41 3 — Int J Epidemiol. Romieu I, Escamilla-Nunez MC, Sanchez-Zamorano LM, Lopez-Ridaura R, Torres-Mejia G, Yunes EM et al The association between body shape silhouette and dietary pattern among Mexican women.
Public Health Nutr 15 1 — Scientific Advisory Committee on Nutrition Carbohydrates and health. Mirza NM, Palmer MG, Sinclair KB, McCarter R, He J, Ebbeling CB et al Effects of a low glycemic load or a low-fat dietary intervention on body weight in obese Hispanic American children and adolescents: a randomized controlled trial.
Am J Clin Nutr 97 2 — Tobias DK, Chen M, Manson JE, Ludwig DS, Willett W, Hu FB Effect of low-fat diet interventions versus other diet interventions on long-term weight change in adults: a systematic review and meta-analysis.
Lancet Diabetes. Endocrinol 3 12 — Hu T, Mills KT, Yao L, Demanelis K, Eloustaz M, Yancy WS Jr. Am J Epidemiol Suppl 7 :S44—S Donnelly JE, Blair SN, Jakicic JM, Manore MM, Rankin JW, Smith BK et al American College of Sports Medicine Position Stand.
Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc 41 2 — Thorogood A, Mottillo S, Shimony A, Filion KB, Joseph L, Genest J et al Isolated aerobic exercise and weight loss: a systematic review and meta-analysis of randomized controlled trials.
Am J Med 8 — Miller CT, Fraser SF, Levinger I, Straznicky NE, Dixon JB, Reynolds J et al The effects of exercise training in addition to energy restriction on functional capacities and body composition in obese adults during weight loss: a systematic review.
PloS one 8 11 :e Ismail I, Keating SE, Baker MK, Johnson NA A systematic review and meta-analysis of the effect of aerobic vs. resistance exercise training on visceral fat. Obes Rev Off J Int Assoc Study Obesity 13 1 — PLoS One 8 12 :e Hu FB, Li TY, Colditz GA, Willett WC, Manson JE Television watching and other sedentary behaviors in relation to risk of obesity and type 2 diabetes mellitus in women.
Jama 14 — Liao Y, Liao J, Durand CP, Dunton GF Which type of sedentary behaviour intervention is more effective at reducing body mass index in children?
A meta-analytic review. Obes Rev Off J Int Assoc Study Obesity 15 3 — Blundell JE, Gibbons C, Caudwell P, Finlayson G, Hopkins M Appetite control and energy balance: impact of exercise. ObesRev 16 Suppl 1 — Franks PW, Ravussin E, Hanson RL, Harper IT, Allison DB, Knowler WC et al Habitual physical activity in children: the role of genes and the environment.
Am J Clin Nutr 82 4 — CAS PubMed Google Scholar. Locke AE, Kahali B, Berndt SI, Justice AE, Pers TH, Day FR et al Genetic studies of body mass index yield new insights for obesity biology. Nature — Ahmad S, Varga TV, Franks PW Gene x environment interactions in obesity: the state of the evidence.
Hum Hered 75 2—4 — Kilpelainen TO, Qi L, Brage S, Sharp SJ, Sonestedt E, Demerath E et al Physical activity attenuates the influence of FTO variants on obesity risk: a meta-analysis of , adults and 19, children. PLoS Med 8 11 :e Qi Q, Chu AY, Kang JH, Jensen MK, Curhan GC, Pasquale LR et al Sugar-sweetened beverages and genetic risk of obesity.
N Engl J Med 15 — Diabetologia 57 3 — Nettleton JA, Follis JL, Ngwa JS, Smith CE, Ahmad S, Tanaka T et al Gene x dietary pattern interactions in obesity: analysis of up to 68, adults of European ancestry.
Hum Mol Genet 24 16 — van Dijk SJ, Tellam RL, Morrison JL, Muhlhausler BS, Molloy PL Recent developments on the role of epigenetics in obesity and metabolic disease. Clinical Epigenetics 7 1 Chambers JC, Loh M, Lehne B, Drong A, Kriebel J, Motta V et al.
Epigenome-wide association of DNA methylation markers in peripheral blood from Indian Asians and Europeans with incident type 2 diabetes: a nested case—control study. Lancet Diabetes Endocrinol 3 7 — Dick KJ, Nelson CP, Tsaprouni L, Sandling JK, Aïssi D, Wahl S et al. DNA methylation and body-mass index: a genome-wide analysis.
Blottiere HM, de Vos WM, Ehrlich SD, Dore J Human intestinal metagenomics: state of the art and future. Curr Opin Microbiol 16 3 — Vangay P, Ward T, Gerber JS, Knights D Antibiotics, pediatric dysbiosis, and disease.
Cell Host Microbe 17 5 — Le Chatelier E, Nielsen T, Qin J, Prifti E, Hildebrand F, Falony G et al Richness of human gut microbiome correlates with metabolic markers.
Dao MC, Everard A, Aron-Wisnewsky J, Sokolovska N, Prifti E, Verger EO et al Akkermansia muciniphila and improved metabolic health during a dietary intervention in obesity: relationship with gut microbiome richness and ecology.
Gut 65 3 — Kong LC, Holmes BA, Cotillard A, Habi-Rachedi F, Brazeilles R, Gougis S et al Dietary patterns differently associate with inflammation and gut microbiota in overweight and obese subjects. PLoS One 9 10 :e Lobstein T, Baur L, Uauy R, TaskForce IIO Obesity in children and young people: a crisis in public health.
Obes Rev 5 Suppl 1 :4— Perez-Morales E, Bacardi-Gascon M, Jimenez-Cruz A Sugar-sweetened beverage intake before 6 years of age and weight or BMI status among older children; systematic review of prospective studies.
Nutr Hosp 28 1 — JAMA 16 — Fatima Y, Doi SAR, Mamun AA Longitudinal impact of sleep on overweight and obesity in children and adolescents: a systematic review and bias-adjusted meta-analysis. Obes Rev 16 2 — WHO Global strategy on diet, physical activity and health—what are the causes?
World Health Organization. International Society for Developmental Origins of Health and Disease. Tie HT, Xia YY, Zeng YS, Zhang Y, Dai CL, Guo JJ et al Risk of childhood overweight or obesity associated with excessive weight gain during pregnancy: a meta-analysis.
Arch Gynecol Obstet 2 — Norris SA, Osmond C, Gigante D, Kuzawa CW, Ramakrishnan L, Lee NR et al Size at birth, weight gain in infancy and childhood, and adult diabetes risk in five low- or middle-income country birth cohorts.
Diabetes Care 35 1 — Adair LS, Martorell R, Stein AD, Hallal PC, Sachdev HS, Prabhakaran D et al Size at birth, weight gain in infancy and childhood, and adult blood pressure in 5 low- and middle-income-country cohorts: when does weight gain matter?
Am J Clin Nutr 89 5 — de Beer M, Vrijkotte TG, Fall CH, van Eijsden M, Osmond C, Gemke RJ Associations of infant feeding and timing of linear growth and relative weight gain during early life with childhood body composition. Int J Obes Lond 39 4 — Papadimitriou A Timing of adiposity rebound and prevalence of obesity.
J Pediatr 2 Weng SF, Redsell SA, Swift JA, Yang M, Glazebrook CP Systematic review and meta-analyses of risk factors for childhood overweight identifiable during infancy.
Arch Dis Child 97 12 — Pearce J, Taylor MA, Langley-Evans SC Timing of the introduction of complementary feeding and risk of childhood obesity: a systematic review.
Int J Obesity 37 10 — Wilson SM, Sato AF Stress and paediatric obesity: what we know and where to go Stress. Health London 30 2 — Cecchini M, Sassi F, Lauer JA, Lee YY, Guajardo-Barron V, Chisholm D. Tackling of unhealthy diets, physical inactivity, and obesity: health effects and cost-effectiveness.
Gortmaker SL, Long MW, Resch SC, Ward ZJ, Cradock AL, Barrett JL et al Cost effectiveness of childhood obesity interventions: evidence and methods for CHOICES.
Am J Prev Med 49 1 — Pan American Health Organization Recommendations from a Pan American Health Organization Expert Consultation on the Marketing of Food and Non-Alcoholic Beverages to Children in the Americas. PAHO, Washington, D. Jenkin G, Madhvani N, Signal L, Bowers S A systematic review of persuasive marketing techniques to promote food to children on television.
Obes Rev 15 4 — Hawkes C Regulating and litigating in the public interest: regulating food marketing to young people worldwide: trends and policy drivers. Am J Public Health 97 11 — Wang YWY, Wilson RF, Bleich S, Cheskin L, Weston C, Showell N, Fawole O, Lau B, Segal J Childhood obesity prevention programs: comparative effectiveness review and meta-analysis internet: agency for healthcare research and quality US ; Contract No.
USDA Nutrition Evidence Library NEL Dietary patterns systematic review. UK Scientific Advisory Committee on Nutrition The influence of maternal, fetal and child nutrition on development of chronic disease in later life.
balanxe out. Performance-enhancing supplements your energy balance wnd involves tracking what types of Energy balance and fat loss you put into your Energu, the Performance-enhancing nutrition at which you burn those calories, baance type of activity you do outside the gym, Enerby a whole lot Energy balance and fat loss. Blaance a little know-how behind these subjects can make your bulking or cutting phase a smooth one. None of these supplements are meant to treat or cure any disease. If you feel you may be deficient in a particular nutrient or nutrients, please seek out a medical professional. Calories are a unit of measurement used to calculate the energy content of food and beverages — or how much fuel they provide your body. Your body uses these calories for everything from temperature regulation to lifting heavy iron at the gym. The aim of bbalance paper Energy balance and fat loss to balxnce the Energy balance and fat loss of the association between energy balance and obesity. Sports nutrition for recovery and injury rehabilitation December Energy balance and fat loss, the International Fxt for Research on Cancer BalxnceLyon, France convened balancs Working Group of international experts Enrrgy review the evidence lows energy balance and obesity, with a focus on Low and Middle Income Countries LMIC. The global epidemic of obesity and the double burden, in LMICs, of malnutrition coexistence of undernutrition and overnutrition are both related to poor quality diet and unbalanced energy intake. Dietary patterns consistent with a traditional Mediterranean diet and other measures of diet quality can contribute to long-term weight control. Limiting consumption of sugar-sweetened beverages has a particularly important role in weight control. Genetic factors alone cannot explain the global epidemic of obesity. However, genetic, epigenetic factors and the microbiota could influence individual responses to diet and physical activity.
0 thoughts on “Energy balance and fat loss”