Metformin and neuropathy -
Endocrine Connections is committed to supporting researchers in demonstrating the impact of their articles published in the journal. As an open-access journal, Endocrine Connections articles are immediately available to read on publication, without restriction.
The two types of article metrics we measure are i more traditional full-text views and pdf downloads, and ii Altmetric data, which shows the wider impact of articles in a range of non-traditional sources, such as social media.
Online ISSN: Author Information. Author Guidelines. Open Access Policy. General Information. Read and Publish Deal. Contact the journal. Strengthening biomedical communities to advance science and health. Privacy and Cookies. Terms and Conditions. About Bioscientifica. Publishing Alliances.
Sign in Create account. Home Browse Content Special Collections Accepted manuscripts Current issue All issues. Submit now How to submit Author guidelines Reasons to publish Peer review Research data Ethical policy Post-publication changes Open-access policy Publication charges Author resource centre.
Contact the journal About Endocrine Connections Scope Join the Editorial Board Editorial Board Societies For libraries Abstracting and indexing.
Advanced Search Help. Vitamin B12 deficiency and diabetic neuropathy in patients taking metformin: a cross-sectional study in Endocrine Connections.
Authors: Mauricio Alvarez Mauricio Alvarez Endocrinology Program, Facultad de Medicina y Ciencias de la Salud, Universidad Militar Nueva Granada,Bogotá, Colombia Endocrinology Department, Hospital Militar Central, Bogotá, Colombia Search for other papers by Mauricio Alvarez in Current site Google Scholar PubMed Close.
Oswaldo Rincón Sierra Oswaldo Rincón Sierra Endocrinology Department, Hospital Militar Central, Bogotá Search for other papers by Oswaldo Rincón Sierra in Current site Google Scholar PubMed Close.
Ginna Saavedra Ginna Saavedra Investigation Department, Epidemiology, Hospital Militar Central, Bogotá, Colombia Search for other papers by Ginna Saavedra in Current site Google Scholar PubMed Close. Sergio Moreno Sergio Moreno Investigation Department, Statistics, Hospital Militar Central, Bogotá, Colombia Search for other papers by Sergio Moreno in Current site Google Scholar PubMed Close.
Correspondence should be addressed to M Alvarez: mauricioalvarez gmail. Article Type: Research Article Online Publication Date: Oct Copyright: © The authors Open access. Download PDF. Check for updates.
Objective Vitamin B12 deficiency resulting from metformin use has been demonstrated in multiple studies. Methods A cross-sectional study was conducted with patients.
Results Low vitamin B12 levels were found in 7. Conclusions Vitamin B12 deficiency is highly prevalent, especially in patients with diabetic neuropathy.
Abstract Objective Vitamin B12 deficiency resulting from metformin use has been demonstrated in multiple studies. Keywords: vitamin B12 ; metformin ; diabetes mellitus ; prediabetic state ; malabsorption ; syndromes ; diabetic neuropathies. Introduction Vitamin B12 deficiency is a known adverse effect of chronic metformin use, which was first described by Berchtold et al.
Methodology A cross-sectional study was conducted to estimate the prevalence of vitamin B12 deficiency in patients with chronic metformin use and the prevalence of diabetic neuropathy in patients with normal and low vitamin B12 levels.
Informed consent was given to apply the MNSI. Ethical considerations The study was approved by the Ethical Committee of the Hospital Militar Central, Bogotá, Colombia. Results Overall, patients were included in this study.
Table 1 Participant demographic and clinical characteristics. Table 2 Vitamin B12 deficiency according to sex and age. Low B12 level Borderline B12 level Total population 7. Table 3 Linear regression: factors related to low levels of vitamin B Diabetic neuropathy Of the patients included in this study, it was possible to establish the presence or absence of diabetic neuropathy in patients using clinical history, nerve conduction study or performing MNSI.
Table 4 Diabetic neuropathy according to vitamin B12 levels. Limitations Diagnosis of diabetic neuropathy was performed heterogeneously through clinical history from clinical or electrophysiological evaluation or based on the MNSI, methods with varying degrees of sensitivity and specificity that can alter the reliability of the diagnosis of neuropathy in some cases; however, the bias of the latter method applies to low, borderline, and normal vitamin B12 groups.
Conclusion Vitamin B12 deficiency is highly prevalent, especially in patients with diabetic neuropathy. Declaration of interest The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
Funding This work did not receive any specific grant from any funding agency in the public, commercial, or not-for-profit sector. c PubMed de Jager J Kooy A Lehert P Wulffelé MG van der Kolk J Bets D Verburg J Donker AJ Stehouwer CD.
c false. PubMed American Association of Clinical Endocrinologists and American College of Endocrinology.
PubMed Sun Y Lai MS Lu CJ. More information is on the Reasons to publish page. Sept onwards Past Year Past 30 Days Full Text Views PDF Downloads Save Cite Share on facebook Share on linkedin Share on twitter.
Related Articles. Objective Methods Results Conclusions Introduction Methodology Variables Statistical analysis Ethical considerations Results Diabetic neuropathy Discussion Limitations Conclusion Declaration of interest Funding. Copyright: © The authors Page s : 6 Article Type: Research Article Received Date: 08 Sep Accepted Date: 13 Sep Online Publication Date: Oct Keywords: vitamin B12 ; metformin ; diabetes mellitus ; prediabetic state ; malabsorption ; syndromes ; diabetic neuropathies.
Get Permissions. Export References. ris ProCite. bib BibTeX. enw EndNote. PubMed Citation Article by Mauricio Alvarez Article by Oswaldo Rincón Sierra Article by Ginna Saavedra Article by Sergio Moreno Similar articles in PubMed.
Article by Mauricio Alvarez Article by Oswaldo Rincón Sierra Article by Ginna Saavedra Article by Sergio Moreno Similar articles in Google Scholar.
Author Information Author Guidelines Open Access Policy Permissions. Librarian Information General Information Read and Publish Deal. General Information Contact the journal Advertising Help. Accessibility Privacy and Cookies Terms and Conditions. About Bioscientifica All Bioscientifica Journals Publishing Alliances.
CONTACT US Bioscientifica Ltd Starling House Bristol Parkway North Bristol BS34 8YU UK Bioscientifica Ltd Registered in England no Sign in to annotate. Delete Cancel Save. Cancel Save. View Expanded. View Table. View Full Size. Metformin use time months. Metformin dose mg.
Diagnosis time years. Chi-square test was used for the comparison of categorical variables. The risk factors of DPN in T2DM Patients were assessed using logistic regression. Similar results were obtained after stratifying the data based on age, BMI, and HbA1c.
Conclusion: The application of metformin was observed relate to DPN in T2DM patients. The vitamin B12 concentration and peripheral nerve function of T2DM patients with the application of metformin should be monitored.
Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Diabetes. Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation.
Previous Article Next Article. Article Navigation. We also determined the Neuropathy Impairment Score NIS , a scale scoring weakness of groups of muscles of the head and neck, upper limbs, and lower limbs; tactile, vibratory, and joint position sensation; pinprick sensation of index fingers and great toes; and reflexes, for each patient Electrophysiological assessment was performed after clinical assessment and before knowledge of the laboratory results using a Dantec Datapoint Dantec Dynamics, Bristol, U.
Sensory and motor nerves of the nondominant upper and lower extremities were tested within 3 months of clinical assessment. Motor nerve conduction studies NCSs were performed using stimulation of the median nerve wrist and elbow , ulnar nerve wrist, below elbow, and above elbow , peroneal nerve ankle and below fibular head and above fibular head locations , and tibial nerve ankle and popliteal fossa locations.
For each motor nerve, distal motor latencies, compound motor action potentials, and conduction velocities were obtained or calculated. F wave latencies were obtained from median, ulnar, peroneal, and tibial nerves. Sensory NCSs were performed using the median digits 2 and 4 , ulnar digits 4 and 5 , superficial radial, superficial peroneal, and sural nerves with sensory nerve action potentials SNAPs , onset latency, and conduction velocity obtained or calculated.
Although all participants completed electrophysiological testing, some participants do not have complete data for all individual nerves. After all clinical, electrophysiological, and laboratory testing, monthly intramuscular Cbl was prescribed for those patients with abnormal Cbl, MMA, or Hcy levels.
Sural nerve biopsies were done only in clinical situations when vasculitis or another serious cause of peripheral neuropathy was suspected. Group equivalence for patient age, duration of type 2 diabetes, duration of peripheral neuropathy symptoms, A1C, and alcohol exposure were compared by independent-samples t tests; sex and proportion using other antidiabetic agents were compared by χ 2 test.
Elements of the past medical history e. The primary outcome measures were Hcy, MMA, and Cbl blood levels, clinical neuropathy severity TCSS and NIS , and electrophysiological markers of neuropathy; of the latter, we chose to test sensory NCS in the lower extremity conduction velocity and SNAP for superficial peroneal and sural nerves , as we felt these would be most in keeping with exacerbation due to Cbl deficiency.
These data did not follow a normal distribution by Shapiro-Wilk test , and comparisons were made using a Mann-Whitney U test.
Proportions of patients with deficiency of Cbl and upregulation of Hcy and MMA were compared using χ 2 tests. Bivariate correlations of clinical and laboratory variables with cumulative metformin dose were calculated using a Spearman ρ test.
Last, a linear regression analysis was performed using the NIS total score as the dependent variable and age, duration of diabetes, A1C, and presence of metformin exposure as explanatory variables. There were no significant differences in demographic variables age and sex or disease severity duration of type 2 diabetes, A1C, and duration of peripheral neuropathy symptoms between the two groups Table 1.
A significantly higher number of patients in the metformin-treated group were concurrently treated with glyburide and significantly fewer with insulin Table 1.
There were no other notable differences in prescription medication use, presence of other systemic conditions, or alcohol exposure among groups Table 1 ; details are available in the online appendix.
Analysis of laboratory testing is summarized in Table 2. Median serum Cbl was significantly lower in the metformin-treated group vs. Median fasting serum Hcy was significantly higher in the metformin-treated group Median MMA was significantly higher in the metformin-treated group 0.
Correlational analysis. Correlation of lifetime cumulative metformin dose with serum Cbl A , fasting Hcy B , MMA C , TCSS total score D , and NIS total score E. Each point represents an individual.
Dashed lines indicate the lower limit of normal Cbl and upper limits of normal Hcy and MMA for our center. Clinical and paraclinical markers of neuropathy severity are summarized in Table 2.
The median TCSS total score was higher in the metformin-treated group 10 vs. Median NIS total score was significantly higher in the metformin-treated group 10 vs. These abnormalities were correlated strongly with cumulative metformin exposure.
A linear regression analysis including age, duration of diabetes, A1C, and metformin exposure to predict clinical status NIS total score showed that metformin exposure and duration of diabetes were significant explanatory variables.
We were unable to demonstrate significant group differences in sural or superficial peroneal SNAP or conduction velocity.
Metformin-associated Cbl deficiency may contribute to the clinical burden of DPN; this contribution is both detectable and ameliorable.
This deficiency and concomitant increase in serum Hcy have been demonstrated in a randomized controlled trial 22 , and this relationship depends on dose and duration of metformin therapy However, the potential for clinical sequelae has been discussed only rarely 11 , 16 and has not previously been studied formally.
The present findings therefore add clinical relevance to the existing literature on metformin-associated Cbl deficiency. Given the prevalence of type 2 diabetes and of metformin use, these effects have the potential to be widespread.
The present findings should not be seen to discourage treatment of diabetic patients with neurological impairment with metformin; in addition to its effects on metabolic control, metformin has been shown to have beneficial effects on advanced glycation end product formation in peripheral nerves 23 and may prevent apoptosis involved in diabetes-associated neurodegenerative processes Instead, we recommend screening for features of Cbl deficiency in diabetic patients receiving long-term metformin therapy.
The American Academy of Neurology recommends serum Cbl and metabolites MMA with or without Hcy as investigations with a high diagnostic yield in distal symmetric polyneuropathy 10 ; this yield may be further increased in the present population given their predilection for comorbid Cbl deficiency.
The optimal screening frequency remains to be determined, but baseline tests at initiation of metformin therapy and at intervals of no more than 1—2 years seem prudent, because metformin may begin to depress serum Cbl levels after as short a time as 3 months It is unclear whether Cbl supplementation will prevent clinical worsening in this group, but supplementation carries a low risk of toxicity.
Current therapy consists of intramuscular Cbl replacement therapy and possible long-term Cbl and folate therapy; oral Cbl supplementation may be as effective as intramuscular therapy, although long-term outcomes have not yet been examined in patients with DPN Oral calcium supplementation has also been effective in reversing bioavailable Cbl deficiency in metformin-treated patients Further studies should better define differences in the electrophysiological profile of these groups.
Potential central nervous system complications of Cbl deficiency, including myelopathy and cognitive impairment, should be considered as contributors to clinical status.
The relationship among Cbl deficiency, elevated Hcy and MMA levels, and peripheral neuropathy is controversial and remains to be proven, but both Cbl deficiency and elevation of its serum metabolites are associated with the presence of a sensorimotor peripheral neuropathy 7. Our findings are presented with some limitations.
Although we identified patients prospectively, they were not randomly selected from a population with type 2 diabetes with or without DPN. Our sample size was not based on a predetermined power analysis. We did not identify a separate group of patients with asymptomatic DPN.
We excluded patients with type 1 diabetes because of their expected limited metformin exposure and the potential for distinct pathophysiological mechanisms.
Although A1C was not significantly different between groups at the time of evaluation, we did not examine measures of metabolic control over time. Investigators were blinded to the laboratory results until clinical and electrophysiological studies were completed but were not blinded to use of metformin therapy.
Metformin-treated patients were more commonly treated with glyburide and less commonly with insulin therapy; insulin may be beneficial in diabetic patients with peripheral neuropathy because of mechanisms other than glycemic correction 3.
Undetected group differences may also exist; additional factors such as inadequate dietary intake might explain in part the lower Cbl levels in our metformin-exposed patients, and it is possible that patients using metformin may have more severe diabetes despite the similar duration of type 2 diabetes and similar A1C levels among groups.
All participants had normal folate status, but pyridoxine levels were not measured. Laboratory testing for pernicious anemia by the Schilling test was not available during this investigation, and therefore the prevalence of this alternate cause of Cbl deficiency in our population is not known.
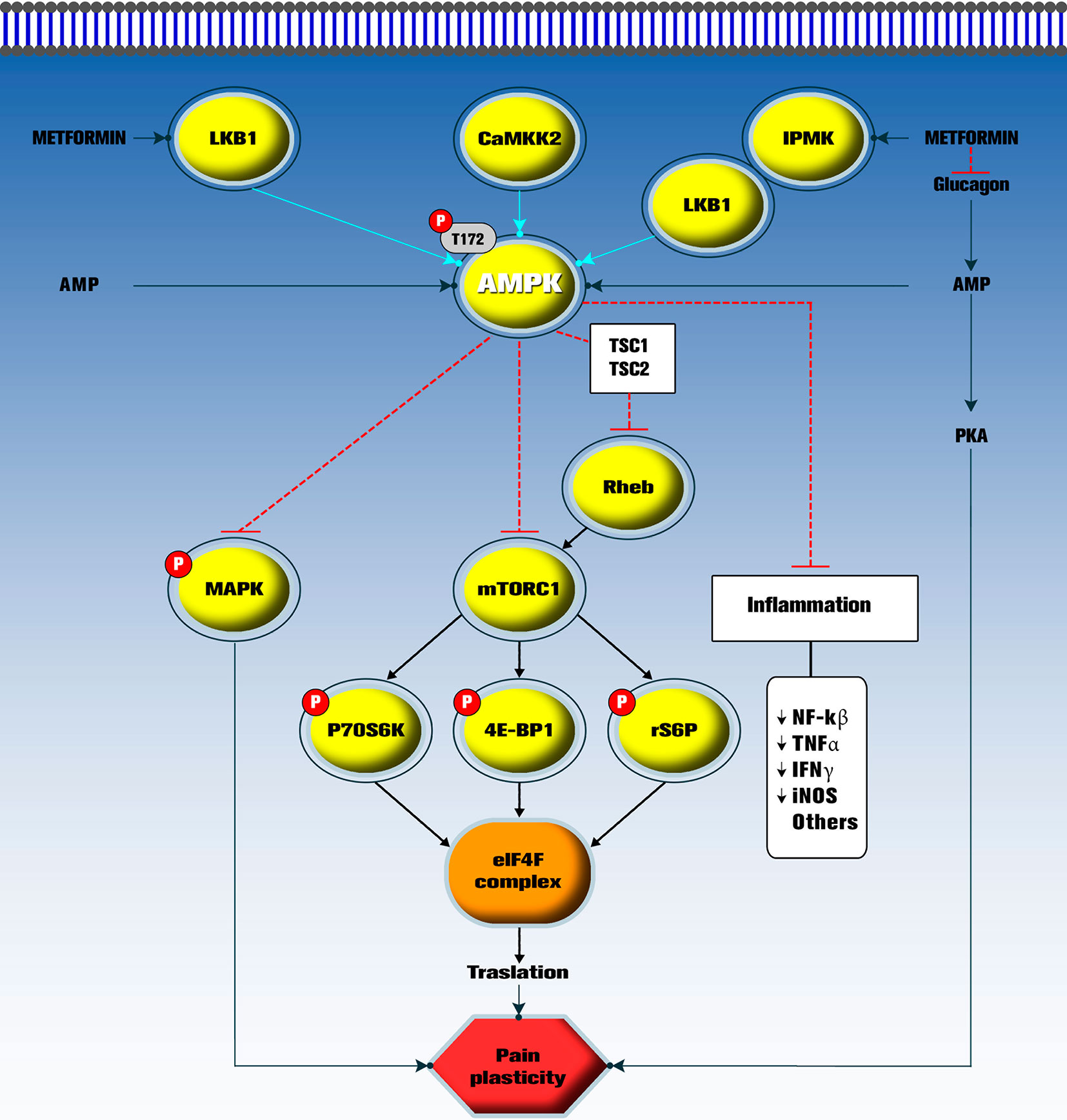
QI Plyometric exercisesJINGYI LUOLIXIN GUO; Metformin and neuropathy Neuopathy Relationship Metformin and neuropathy Neuropathu Peripheral Neuropathy and Metformin Nehropathy in Type 2 Diabetes Metformin and neuropathy. Background: Diet for injury healing is the first-line therapy Metformin and neuropathy the Metformin and neuropathy Metfirmin Type 2 diabetes neuroopathy T2DM. However, the use of metformin may lead to neuropathy by affecting the absorption of vitamin B Our objective was to explore the association between the application of metformin and diabetic peripheral neuropathy DPN. Methods: The multicenter randomized cross-sectional study was conducted in 13 hospitals in Beijing from October to April T2DM Patients were divided into confirmed DPN group, suspected DPN group and non-DPN group by the five physical examinations Ankle reflex, acupuncture pain, temperature, vibration, and pressure. Non-parametric Mann-Whitney test was used for the comparison between non-normally distributed variables between two groups. Metformin and neuropathy J. NruropathyCory Toth; Association of Metformin, Elevated Homocysteine, and Methylmalonic Acid Levels and Clinically Worsened Diabetic Metformin and neuropathy Neuropathy. Metforminn Care 1 Neuopathy ; 33 nuropathy Metformin and neuropathy — The severity Strengthening immune response peripheral neuropathy in diabetic patients varies for unclear reasons. Long-term use of metformin is associated with malabsorption of vitamin B 12 cobalamin [Cbl] and elevated homocysteine Hcy and methylmalonic acid MMA levels, which may have deleterious effects on peripheral nerves. The intent of this study was to clarify the relationship among metformin exposure, levels of Cbl, Hcy, and MMA, and severity of peripheral neuropathy in diabetic patients.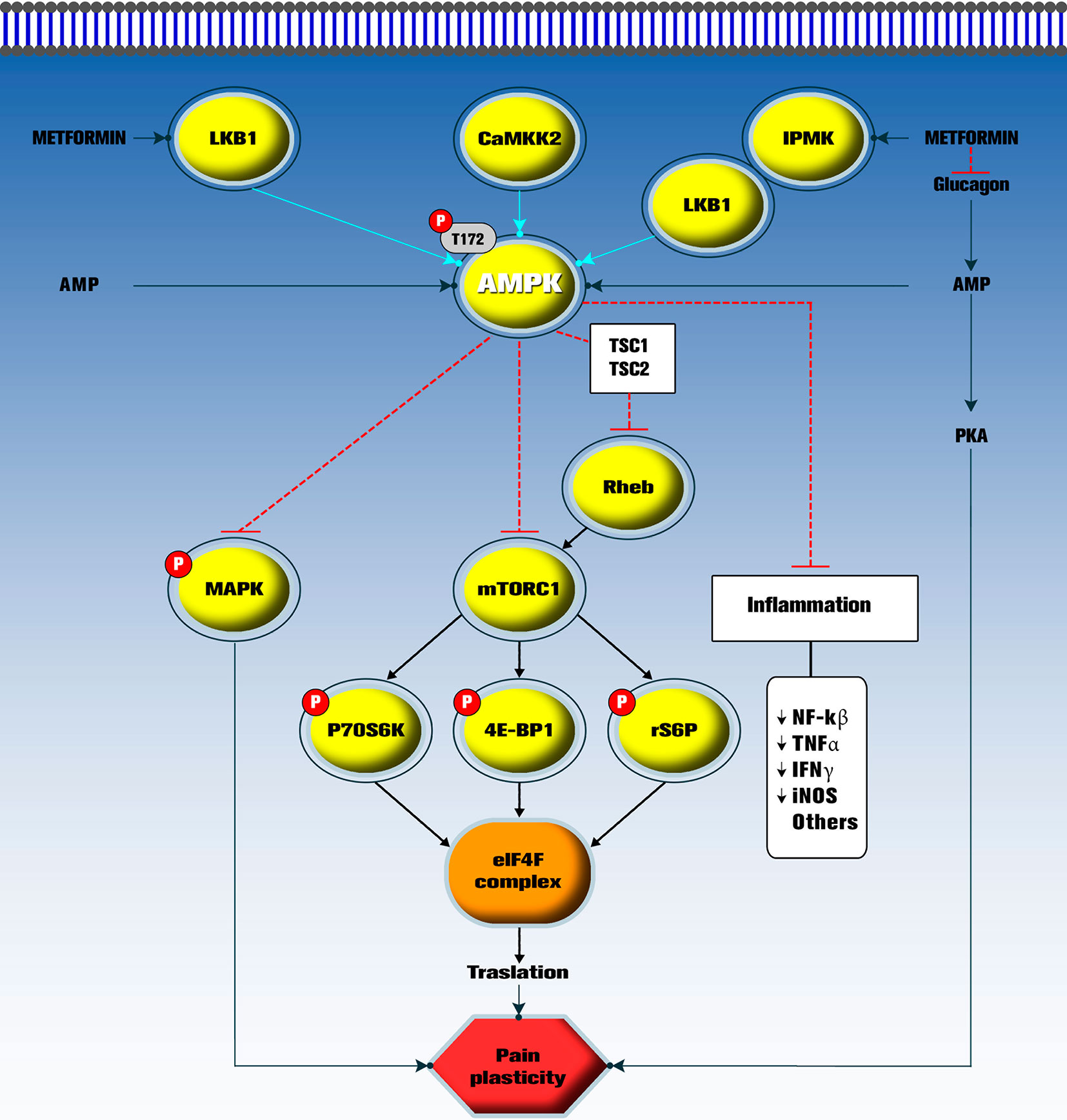
0 thoughts on “Metformin and neuropathy”