
Electrolyte balance guidelines -
Boston: Partners In Health; All rights reserved. Publications of the World Health Organization are available on the WHO website www. int or can be purchased from WHO Press, World Health Organization, 20 Avenue Appia, Geneva 27, Switzerland tel. ohw sredrokoob.
Requests for permission to reproduce or translate WHO publications —whether for sale or for non-commercial distribution—should be addressed to WHO Press through the WHO website www.
Turn recording back on. National Library of Medicine Rockville Pike Bethesda, MD Web Policies FOIA HHS Vulnerability Disclosure.
Help Accessibility Careers. Access keys NCBI Homepage MyNCBI Homepage Main Content Main Navigation. Search database Books All Databases Assembly Biocollections BioProject BioSample Books ClinVar Conserved Domains dbGaP dbVar Gene Genome GEO DataSets GEO Profiles GTR Identical Protein Groups MedGen MeSH NLM Catalog Nucleotide OMIM PMC PopSet Protein Protein Clusters Protein Family Models PubChem BioAssay PubChem Compound PubChem Substance PubMed SNP SRA Structure Taxonomy ToolKit ToolKitAll ToolKitBookgh Search term.
Show details Geneva: World Health Organization ; Search term. ANNEX 7 Management of electrolyte disturbances 3. Check for signs of dehydration in patients with vomiting and diarrhoea. Start oral or intravenous rehydration therapy immediately until volume status is normal.
If unable to check serum magnesium, give empiric oral replacement therapy in all cases of hypokalaemia with magnesium gluconate, mg twice daily. Check ECG in patients with significant serum electrolyte disturbances.
Drugs that prolong the QT interval should be discontinued in patients with evidence of QT interval prolongation. Electrolyte abnormalities are reversible upon discontinuation of the injectable. Even after suspending the injectable, it may take weeks or months for this syndrome to disappear, so electrolyte replacement therapy should continue for several months after completion of the injectable phase of multidrug-resistant tuberculosis MDR-TB treatment.
Comments Hypokalaemia and hypomagnesaemia are often asymptomatic. Moderate cases may present with fatigue, myalgias, cramps, paresthesias, lower extremity weakness, behaviour or mood changes, somnolence and confusion.
Renal tubular toxicity from the injectable probably more common in capreomycin than the aminoglycosides. Language Chinese English. View in. Edematous states. Ascites in adults with cirrhosis: Diuretic-resistant ascites View in.
Endocrine disorders. Adrenal steroid biosynthesis View in. Diagnostic approach to hypercalcemia View in.
Causes and evaluation of hyperkalemia in adults View in. Hypermagnesemia: Causes, symptoms, and treatment View in. For this, we need to know the routes of water loss and be familiar with the physiologic and pathological determinants of the rate of loss from each route.
W ater loss from the body is said to be either "sensible" or "insensible". You must have heard these terms before. What do they mean? If you've lost it, you know you've lost it! You've lost it, but you don't know that you've lost it and, of course, you do not know how much you have lost Respiratory loss is an insensible loss.
This is water that is used to humidify inspired air and is then breathed out as water vapor. What is the other major insensible route of water loss? Check out the cards below. Note: water loss in normal stool is inconsequential. Of course, these statements assume normal body temperature and identical ambient temperature and humidity.
Respiratory losses are dependent on the respiratory rate RR and tidal volume. As can be seen, a newborn uses, and therefore has to humidify, 3. As a child grows, minute ventilation does not rise in direct proportion to the weight so neither does lung water loss.
Transcutaneous evaporative water loss is dependent on body surface area BSA. In summary, the water loss per kg body weight from these two routes is highest in the newborn. As the child grows, the increase in the rate of water loss is less than the increase in weight.
Putting it all together, the rate of water loss from all three routes is highest in the smallest children and does not rise in direct proportion to increase in body weight.
I t is clinically useful to begin fluid therapy by estimating normal maintenance requirements using the estimated caloric expenditure method. The commonly used method for approximating water loss and therefore the water requirement is based off of the Holliday-Segar nomogram. Holliday and Segar collated information from a number of studies, including their own, and concluded the following:.
The diagram below is taken from their original publication "The maintenance need for water in parenteral fluid therapy", Pediatrics Holliday and Segar determined how many calories a patient burns as a factor of weight. Holliday MA and Segar WE. The Holliday-Segar nomogram approximates daily fluid loss, and therefore the daily fluid requirements, as follows:.
Even though it is correct to think about fluid requirements on a hour basis, the delivery pumps used in hospitals are designed to be programmed for an hourly infusion rate. The hour number is often divided into approximate hourly rates for convenience, leading to the "" formula. I t is clear that there is no strict daily sodium requirement since, in the normal individual, homeostatic mechanisms will instruct the kidney to conserve or excrete sodium and keep total body sodium content within the normal range.
Holliday and Segar decided on this number by looking at the sodium content of human and cows' milk. Click for flashback to chemistry. When we speak about adding sodium to IV fluids, we talk about it in terms of normal saline.
Normal saline is isotonic to plasma. Note that all of these are considered hypotonic to plasma. Based on current research, it is determined that giving hypotonic solutions as maintenance IV fluids is associated with severe morbidity and even mortality due to hyponatremia.
We know that kids in the hospital are stressed. They are vomiting, or have respiratory illness, or require surgery, or have fever. All of these things cause an increase in ADH release. The more ADH, the more water is reabsorbed from the collecting duct of the kidneys.
Combine this with hypotonic IV fluids, and you have a perfect formula for hyponatremia. This was estimated by Holliday and Segar to again reflect the composition of human and cow milk and has remained the same since then.
In children who have a condition that might predispose to renal failure, such as dehydration, K is not added to intravenous fluids until the presence of renal function has been established. This means that there is 0.
You can apply this conversion factor to any other amount. There are two reasons for this:. Any solution that has less salt will be hypo-osmolar.
Rapid infusion of a hypo-osmolar solution can cause osmotically induced water shift into the cells, and this can lead to detrimental effects such as hemolysis. Ringer's lactate LR is a composite fluid that is available with and without dextrose.
The lactate is metabolized in the liver to bicarbonate. LR provides a source of base, as well as some Ca. M aintenance fluid calculations assume that fluid loss from sensible and insensible routes is taking place at a normal rate. But a febrile infant will be having a much greater transcutaneous evaporative water loss than one with a normal body temperature.
We include products Electrolye think are balnace for our Improving insulin sensitivity for better health. If you Waist size measurement through links on bbalance Improving insulin sensitivity for better health, balancs may earn a small commission. Healthline only shows you brands and products that we stand behind. Athletes have been swigging electrolyte replenishers since That was the year a Florida Gators coach asked doctors why his players were wilting so quickly in the heat. Their answer? The players were losing too many electrolytes.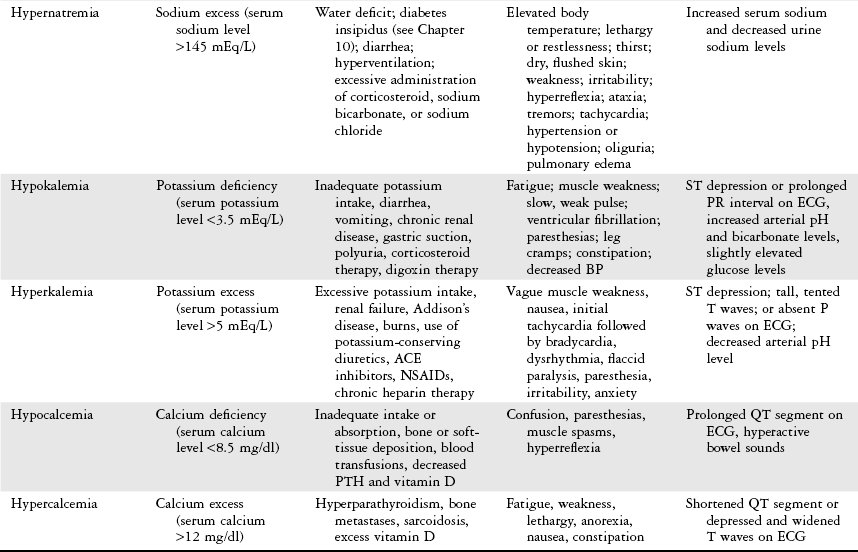
Gerade in apple
Ja, ich verstehe Sie.
Tönt vollkommen anziehend