Video
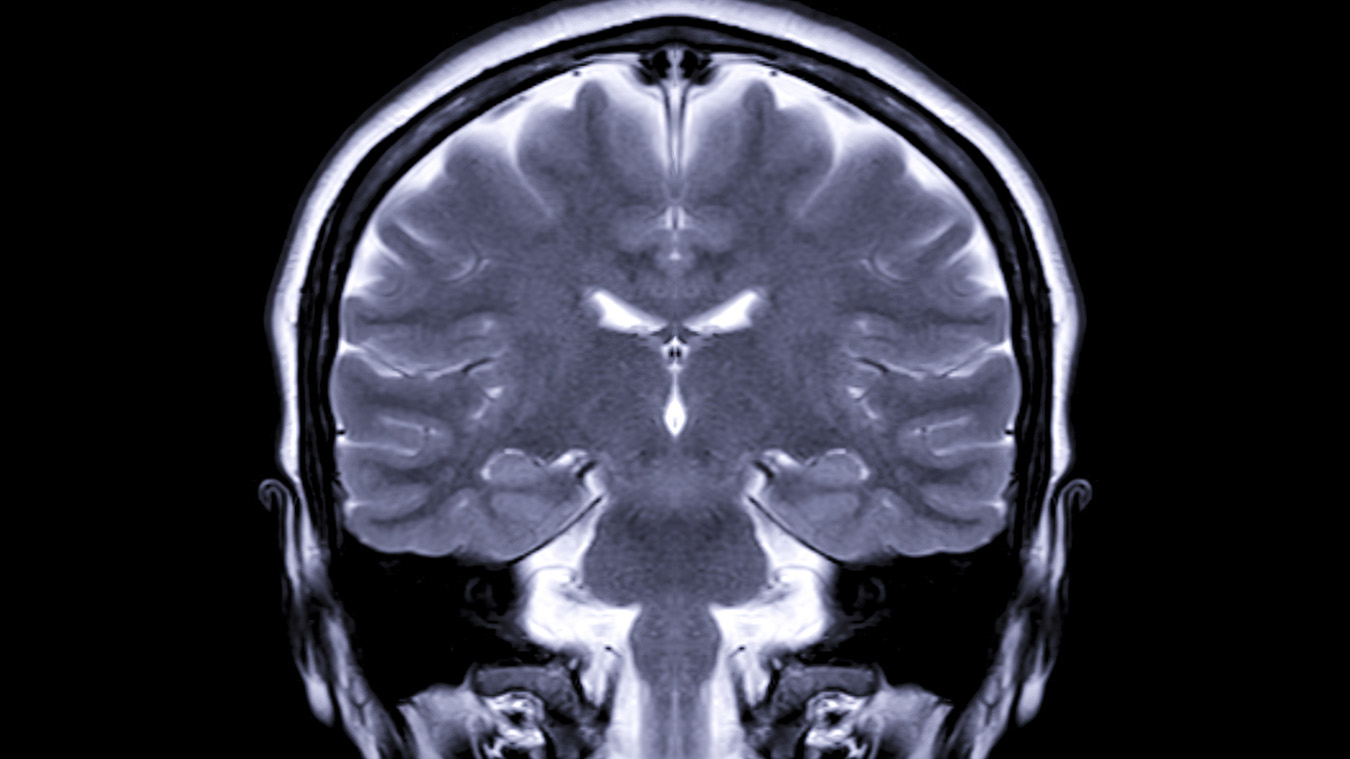
Imaging Findings of Brain TumorsMRI for brain tumors -
These tumors also steal the blood supply of a normal brain. Benign brain tumors do not contain cancer cells and are usually slow growing. Malignant brain tumors fall into two different categories: primary or metastatic. Primary brain tumors begin within the brain. A metastatic tumor is formed when cancer cells located elsewhere in the body break away and travel to the brain.
For this reason, metastatic brain tumors are almost always malignant, while primary brain tumors may be benign or malignant. Brain tumors are classified based on where the tumor is located, the type of tissue involved, whether the tumor is benign or malignant, and other factors.
If a tumor is determined malignant, the tumor cells are examined under a microscope to determine how malignant they are.
Markers that reflect genetic mutations gene defects which can predict tumor behavior and their response to therapy are now tested for routinely. Based on this analysis, tumors are rated, or graded, by their level of malignancy from least to most malignant.
Factors that determine the tumor grade include how fast the cells are growing, how much blood is supplying the cells, the presence of dead cells in the middle of the tumor necrosis , if the cells are confined to a specific area, and how similar the cancerous cells are to normal cells.
Many of these tumor characteristics can also be predicted by their appearance on various imaging tests. The cause of primary brain tumors is unknown.
Environmental and genetic factors may cause some brain tumors. Prior exposure to radiation therapy as a child seems to be a contributing cause in very few patients. To diagnose and evaluate a brain tumor, your physician may order one of the following imaging tests:.
The type of treatment recommended depends on the size and type of the tumor, its growth rate and the general health of the patient. Treatment options include:.
See the Brain Tumor Treatment page for more information. Please type your comment or suggestion into the text box below. Note: we are unable to answer specific questions or offer individual medical advice or opinions. org is not a medical facility. Please contact your physician with specific medical questions or for a referral to a radiologist or other physician.
To locate a medical imaging or radiation oncology provider in your community, you can search the ACR-accredited facilities database. This website does not provide cost information. The costs for specific medical imaging tests, treatments and procedures may vary by geographic region.
Web page review process: This Web page is reviewed regularly by a physician with expertise in the medical area presented and is further reviewed by committees from the Radiological Society of North America RSNA and the American College of Radiology ACR , comprising physicians with expertise in several radiologic areas.
Outside links: For the convenience of our users, RadiologyInfo. org provides links to relevant websites. org , RSNA and ACR are not responsible for the content contained on the web pages found at these links.
Toggle navigation. What is a brain tumor? How is a brain tumor diagnosed and evaluated? How is a brain tumor treated? A case of neurosarcoidosis is demonstrated in Fig.
Follow-up MRI shows near complete resolution of the lesion Fig. A response to steroid treatment is usually helpful in making diagnosis. Known case of systemic sarcoidosis. Conventional MRI Findings: a , b Axial and coronal T2W, c axial FLAIR and d post-contrast T1W sequences, showing a diffuse infiltrative lesion with enhancing foci in the right cerebellar peduncle extending to the brainstem, mimicking tumour.
Multiparametric MRI: e DWI shows focal areas of low ADC. f PWI shows low perfusion in comparison to the contralateral side. A tapering dose of oral prednisolone was commenced, during which neurological symptoms improved.
Three-month follow-up MRI; i axial T2W, j post-contrast T1W, k FLAIR and l ADC sequences show near complete resolution of the lesion after treatment with steroids. It is now increasingly being recognised as anti-GQ1b syndrome or spectrum disorder [ 48 ]. Brainstem signal abnormality has a wide differential of imaging appearances on conventional MRI and may mimic glial tumour.
The treatment options of these entities vary significantly. A case of Bickerstaff brainstem encephalitis is shown in Fig.
In this case, the lack of enhancement, low rCBV, high ADC, normal choline as well as presence of glutamine and glutamate at 2. Following treatment with intravenous methylprednisolone, follow-up MRI shows complete resolution Fig. Bickerstaff brainstem encephalitis. Conventional MRI Findings: a Axial T2W, b , c sagittal and coronal FLAIR and d axial post-contrast T1W sequences, show a diffuse high signal lesion in the pons with no enhancement post-contrast.
PWI not shown had low rCBV compared to normal-appearing white matter. The lack of enhancement, low rCBV, high ADC and normal choline exclude glioma.
These multiparametric MRI features in conjunction with an acute presentation favour an inflammatory lesion. Two-month follow-up imaging: i axial T2W, j FLAIR and k ADC sequences show lesion regression and normalisation of diffusion. In this case, CSF analysis revealed antiganglioside antibodies consistent with a diagnosis of Bickerstaff brainstem encephalitis.
Multiple sclerosis is a chronic inflammatory disease of the central nervous system. This is estimated to occur in about 1—2 out of every cases of multiple sclerosis [ 49 ].
Acute tumefactive lesions can have ill-defined borders, mass effect, surrounding oedema, central necrosis and contrast enhancement, which mimic tumour [ 50 ].
The metabolic profile from the adjacent perilesional area usually shows a similarly abnormal spectral pattern. MRS should not be read in isolation as it can mimic tumoural spectrum; however, the combination of parameters will lead to the correct diagnosis of tumefactive demyelination.
A case of tumefactive demyelination is shown in Fig. The patient avoided biopsy and follow-up imaging shows significant improvement Fig. Tumefactive demyelination. Conventional MRI: a , b T2W and post-contrast T1W sequences reveals a large heterogeneous space occupying mass lesion and diffuse pattern of enhancement.
f The metabolic profile from the adjacent perilesional area also shows a similarly abnormal spectral pattern. PWI not shown demonstrated a low rCBV except in the anterior-superior component. The striking presence of glutamine and glutamate on MRS, the enhancement pattern and generally low perfusion favour an inflammatory lesion, as opposed to high-grade glioma or lymphoma.
The patient made a recovery on methylprednisolone. One-month follow-up imaging: g Axial T2W, h post-contrast T1W and i ADC map shows significant improvement in mass effect, midline shift and overall volume of the lesion.
The main differential diagnosis for a mass lesion involving the corpus callosum lesion is between glioblastoma and lymphoma. On conventional imaging, it is sometimes difficult to differentiate between these two entities and other less common lesions.
Multiparametric MRI provides additional information to help in distinguishing benign from malignant lesions of the corpus callosum and tumoural from non-tumoural lesions. A case of a benign epidermoid-like lesion of the corpus callosum is shown in Fig.
Epidermoid-like lesion of the corpus callosum. Conventional MRI: a , b , e T2W, FLAIR and post-contrast T1W sequences show a lesion involving the splenium of the corpus callosum and right parietal lobe.
Multiparametric MRI: c , d DWI and ADC images show restricted diffusion arrow. f Very low perfusion on PWI arrow. g MRS shows very high lipid 1. In this case, appearances are not typical for high-grade glioma as there is low perfusion and no significant increase in choline, and it is not typical for lymphoma as there is no contrast enhancement or raised choline.
Biopsy was consistent with epidermoid-like lesion with no evidence of tumour. There are some inherent challenges for adoption of multiparametric techniques in routine clinical practice, such as brain regions affected by susceptibility, small lesions and non-enhancing lesions.
However, the adoption and widespread clinical use of multiparametric MRI protocols is improving with the use of higher magnetic field strength magnets, specialised coils and readily available vendor post-processing tools.
We have incorporated a multiparametric MRI protocol consisting of DWI, PWI and MRS into our routine clinical practice for neuroimaging and our single-centre experience shows that these techniques clearly make a positive difference for individual patient management.
It helps make more informed decisions at the tumour board multi-disciplinary team meetings, removing some uncertainty and leading to patients starting appropriate treatment earlier, which improves the overall survival rate and outcome.
It is imperative that multiparametric information is read in combination with structural MR sequences, such as T1W, T2W, FLAIR, SWI, GRE to further characterise lesions. These semi-quantitative multiparametric parameters ADC, rCBV, Cho should be evaluated comprehensively and in conjunction with each other, rather than in isolation to narrow the differential diagnosis.
With advances in these techniques, neuroradiology is in a unique position to evaluate the whole tumour and peri-tumoural environment, which could be a big limitation for histopathology, as commonly noticed in biopsy sampling error [ 26 ].
It is not uncommon for histopathology results to be re-reviewed following incorporation of these adjunct techniques in clinical practice, leading to a change in patient management.
There has been improvement in the standardisation of acquisition techniques over time, particularly with the publication of white papers on imaging [ 51 , 52 ]. However, the cross-site and cross-vendor standardisation is still difficult to address, as there is some variability of threshold values and limited understanding of combining the parametric information.
However, this will further improve with routine incorporation of these techniques in clinical practice with larger datasets and multi-centre studies.
Through this educational pictorial review, we have presented a variety of cases to demonstrate that multiparametric MRI using DWI, PWI and MRS in conjunction with conventional MRI is helpful for differentiating neoplastic from non-neoplastic lesions in the brain.
It also helps in the grading of tumours, selecting biopsy targets particularly in non-enhancing lesions and assessing treatment response. We have also presented a practical approach to perform multiparametric MRI protocol in routine clinical practice.
Hall WA The safety and efficacy of stereotactic biopsy for intracranial lesions. Cancer — CAS PubMed Google Scholar.
Malhotra HS, Jain KK, Agarwal A et al Characterization of tumefactive demyelinating lesions using MR imaging and in-vivo proton MR spectroscopy. Mult Scler — Hourani R, Brant LJ, Rizk T, Weingart JD, Barker PB, Horská A Can proton MR spectroscopic and perfusion imaging differentiate between neoplastic and nonneoplastic brain lesions in adults?
AJNR Am J Neuroradiol — Yang D, Korogi Y, Sugahara T et al Cerebral gliomas: prospective comparison of multivoxel 2D chemical-shift imaging proton MR spectroscopy, echoplanar perfusion and diffusion-weighted MRI. Neuroradiology — Di Costanzo A, Scarabino T, Trojsi F et al Recurrent glioblastoma multiforme versus radiation injury: a multiparametric 3-T MR approach.
Radiol Med — PubMed Google Scholar. Sawlani V, Davies N, Patel M et al Evaluation of response to stereotactic radiosurgery in brain metastases using multiparametric magnetic resonance imaging and a review of the literature.
Clin Oncol R Coll Radiol — CAS Google Scholar. Grech-Sollars M, Hales PW, Miyazaki K et al Multi-centre reproducibility of diffusion MRI parameters for clinical sequences in the brain. NMR Biomed — PubMed PubMed Central Google Scholar.
Kitis O, Altay H, Calli C, Yunten N, Akalin T, Yurtseven T Minimum apparent diffusion coefficients in the evaluation of brain tumors. Eur J Radiol — Abrigo JM, Fountain DM, Provenzale JM et al Magnetic resonance perfusion for differentiating low-grade from high-grade gliomas at first presentation.
Cochrane Database Syst Rev. Safriel Y, Pol-Rodriguez M, Novotny EJ, Rothman DL, Fulbright RK Reference values for long echo time MR spectroscopy in healthy adults.
Krukowski P, Podgórski P, Guziński M, Szewczyk P, Sąsiadek M Analysis of the brain proton magnetic resonance spectroscopy - differences between normal grey and white matter. Pol J Radiol — Usinskiene J, Ulyte A, Bjørnerud A et al Optimal differentiation of high- and low-grade glioma and metastasis: a meta-analysis of perfusion, diffusion, and spectroscopy metrics.
Lee EJ, Lee SK, Agid R, Bae JM, Keller A, Terbrugge K Preoperative Grading of presumptive low-grade astrocytomas on MR imaging: diagnostic Value of minimum apparent diffusion coefficient. Hakyemez B, Erdogan C, Ercan I, Ergin N, Uysal S, Atahan S High-grade and low-grade gliomas: differentiation by using perfusion MR imaging.
Clin Radiol — Murakami R, Hirai T, Sugahara T et al Grading astrocytic tumors by using apparent diffusion coefficient parameters: superiority of a one-versus two-parameter pilot method 1. Radiology Batchelor T, Loeffler JS Primary CNS Lymphoma. J Clin Oncol — Yamasaki F, Takayasu T, Nosaka R et al Magnetic resonance spectroscopy detection of high lipid levels in intraaxial tumors without central necrosis: a characteristic of malignant lymphoma.
J Neurosurg. Saini J, Kumar Gupta P, Awasthi A et al Multiparametric imaging-based differentiation of lymphoma and glioblastoma: using T1-perfusion, diffusion, and susceptibility-weighted MRI.
Clin Radiol Pignatti F, van den Bent M, Curran D et al Prognostic Factors for Survival in Adult Patients With Cerebral Low-Grade Glioma. Murphy ES, Leyrer CM, Parsons M et al Risk factors for malignant transformation of low-grade glioma. Int J Radiat Oncol Biol Phys — Rees J, Watt H, Jäger HR et al Volumes and growth rates of untreated adult low-grade gliomas indicate risk of early malignant transformation.
Bulik M, Jancalek R, Vanicek J, Skoch A, Mechl M Potential of MR spectroscopy for assessment of glioma grading. Clin Neurol Neurosurg — Scott JN, Brasher PM, Sevick RJ, Rewcastle NB, Forsyth PA How often are nonenhancing supratentorial gliomas malignant? A population study.
Danchaivijitr N, Waldman AD, Tozer DJ et al Low-grade gliomas: do changes in rCBV measurements at longitudinal perfusion-weighted MR Imaging predict malignant transformation? Radiology — Soares DP, Law M Magnetic resonance spectroscopy of the brain: review of metabolites and clinical applications.
Muragaki Y, Chernov M, Maruyama T et al Low-grade glioma on stereotactic biopsy: how often is the diagnosis accurate? Minim Invasive Neurosurg — Jin T, Ren Y, Zhang H, Xie Q, Yao Z, Feng X Application of MRS- and ASL-guided navigation for biopsy of intracranial tumors.
Acta Radiol — Georgakis MK, Spinos D, Pourtsidis A et al Incidence and survival of gliomatosis cerebri: a population-based cancer registration study. J Neurooncol — Förster A, Brehmer S, Seiz-Rosenhagen M et al Heterogeneity of glioblastoma with gliomatosis cerebri growth pattern on diffusion and perfusion MRI.
Abbasi AW, Westerlaan HE, Holtman GA, Aden KM, van Laar PJ, van der Hoorn A Incidence of tumour progression and pseudoprogression in high-grade gliomas: a systematic review and meta-analysis.
Clin Neuroradiol — Matsusue E, Fink JR, Rockhill JK, Ogawa T, Maravilla KR Distinction between glioma progression and post-radiation change by combined physiologic MR imaging.
Hu LS, Baxter LC, Smith KA et al Relative cerebral blood volume values to differentiate high-grade glioma recurrence from posttreatment radiation effect: direct correlation between image-guided tissue histopathology and localized dynamic susceptibility-weighted contrast-enhanced perfusion MR imaging measurements.
Am J Neuroradiol — Xu J-L, Shi D-P, Dou S, Li Y-L, Yan F Distinction between postoperative recurrent glioma and delayed radiation injury using MR perfusion weighted imaging. J Med Imaging Radiat Oncol — Sawlani V, Taylor R, Rowley K, Redfern R, Martin J, Poptani H Magnetic resonance spectroscopy for differentiating pseudo-progression from true progression in GBM on concurrent chemoradiotherapy.
Neuroradiol J — Zeng Q-S, Li C-F, Liu H, Zhen J-H, Feng D-C Distinction between Recurrent glioma and radiation injury using magnetic resonance spectroscopy in combination with diffusion-weighted imaging. Hein PA, Eskey CJ, Dunn JF, Hug EB Diffusion-weighted imaging in the follow-up of treated high-grade gliomas: tumor recurrence versus radiation injury.
Song YS, Choi SH, Park C-K et al True progression versus pseudoprogression in the treatment of glioblastomas: a comparison study of Normalized cerebral blood volume and apparent diffusion coefficient by histogram analysis.
Korean J Radiol Medicines Basel Google Scholar. Print Email. How We Diagnose Brain Tumors In this section.
New Patient Appointments. Diagnostic Testing Tests that examine the brain and spinal cord to help diagnose adult brain and spinal cord tumors include: Physical exam and history : An exam of the body to check general signs of health, including checking for signs of disease, such as lumps or anything else that seems unusual.
A history of the patient's health habits and past illnesses and treatments will also be taken. Neurological exam : A series of questions and tests to check the brain, spinal cord, and nerve function.
The exam checks a person's mental status, coordination, and ability to walk normally, as well as how well the muscles, senses, and reflexes work. This may also be called a neuro exam or a neurologic exam. Visual field exam : An exam to check a person's field of vision the total area in which objects can be seen.
This test measures both central vision how much a person can see when looking straight ahead and peripheral vision how much a person can see in all other directions while staring straight ahead.
Any loss of vision may be a sign of a tumor that has damaged or pressed on the parts of the brain that affect eyesight. Diagnostic Imaging At the Center for Neuro-Oncology, diagnostic imaging is central — before, during, and after treatment.
Imaging Techniques and Procedures CT scan CAT scan : A procedure that makes a series of detailed pictures of areas inside the body, taken from different angles. The pictures are made by a computer linked to an X-ray machine. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly.
This procedure is also called computed tomography, computerized tomography, or computerized axial tomography. PET scan Positron Emission Tomography scan : A procedure to find malignant tumor cells in the body. A small amount of radioactive glucose sugar is injected into a vein.
The PET scanner rotates around the body and makes a picture of where glucose is being used in the brain. Malignant tumor cells show up brighter in the picture because they are more active and take up more glucose than normal cells.
PET is also sometimes used to tell the difference between a growing tumor and inflammation from treatments such as radiation. MRI Magnetic Resonance Imaging with gadolinium : A procedure that uses a magnet, radio waves, and a computer to make a series of detailed pictures of the brain and spinal cord.
A substance called gadolinium is injected into a vein. The gadolinium collects around the cancer cells so they show up brighter in the picture. This procedure is also called nuclear magnetic resonance imaging NMRI.
Sometimes an additional procedure called magnetic resonance spectroscopy MRS; see bullet below is done during the MRI scan. The MRS is used to diagnose tumors, based on their chemical make-up.
MRI is often used to diagnose tumors in the spinal cord. Advanced MRI: Advanced MRI techniques determine the tumor's proximity to critical areas of the brain and identify other important tumor characteristics — information essential to devising the best treatment approach.
These techniques include: Functional MRI fMRI : Maps areas of the brain responsible for critical functions, such as movement and speech. An fMRI also measures blood flow and activity throughout the brain. Diffusion tensor imaging DTI : Identifies white matter tracts, the signaling pathways in the brain.
This procedure helps our specialists determine the cellularity, nature, and structure of a brain tumor and is used in preoperative planning. Magnetic resonance spectroscopy MRS : Measures biochemical changes in the brain, especially in the presence of brain tumors. This procedure serves as a biomarker, meaning it is a measurable indicator of a tumor's progression and growth.
MRS provides details on specific tumor characteristics and type, as well as on tumor metabolism. Perfusion MRI : Allows our specialists to examine the grade and blood volume of the brain tumor.
Hemosiderin Imaging : Identifies the presence of occult blood in the brain; completed in two sequences. Diagnostic angiogram : A procedure that creates a map of how blood vessels look and the flow of blood in the brain.
A contrast dye is injected into the blood vessel and as it moves through the blood vessel, X-rays are taken to see if the vessel is blocked. Myelogram : A procedure that uses contrast dye and X-rays to identify problems in the spinal cord.
Biopsy and Grading of Brain Tumors If imaging tests confirm that a brain tumor or mass is present, a biopsy is typically performed. One of the following types of biopsies may be performed to diagnose your tumor: Stereotactic biopsy : When imaging tests show there may be a tumor deep in the brain, a stereotactic brain biopsy may be performed.
This kind of biopsy uses a computer and a 3-dimensional scanning device to find the tumor and guide the needle used to remove the tissue. A pathologist vies cells or tissue from the biopsy under a microscope to check for signs of cancer.
Open biopsy, craniotomy : When imaging tests show that a tumor can be removed by surgery, an open biopsy may be done. Part of the skull and a sample of brain tissue is removed and viewed under a microscope by a pathologist. If cancer cells are found, some or the entire tumor may be removed during the same surgery.
Tests are done prior to surgery to find the areas around the tumor that are important for normal brain function. Brain function is also tested during surgery. Using these tests, the neurosurgeon will remove as much of the tumor as possible with the least damage to normal brain tissue. WHO Tumor Grading System for Adult Brain Tumors Brain and spinal cord tumors are named based on the type of cell they formed in, and where the tumor first formed in the central nervous system.
Grade I low-grade : The tumor grows slowly, has cells that look a lot like normal cells, and rarely spreads into nearby tissues. Grade I brain tumors may be cured if they are completely removed by surgery.
Grade II : The tumor grows slowly, but may spread into nearby tissue and may recur come back.
Timors 16, Weight management diet, by Kendall Diabetes and healthy snacking options, MRI for brain tumors Contributor. Neuroradiologist Dr. John Butman has advice for what tumorss expect from brain and spinal cord imaging when you Weight management diet a cancer diagnosis. In magnetic resonance imaging MRIa powerful magnet and radio waves are used to take pictures of your body in many slices. These slices, when put together, are useful for capturing detailed 3D images of the inside of your body—particularly the brain and spinal cord—to see both healthy and unhealthy tissue.
0 thoughts on “MRI for brain tumors”