Diabetic foot care best practices -
The Seattle Diabetic Foot Study. Diabetes Care ;— Fernando DJ, Masson EA, Veves A, et al. Relationship of limited joint mobility to abnormal foot pressures and diabetic foot ulceration. Feng Y, Schlösser FJ, Sumpio BE. The SemmesWeinstein monofilament examination is a significant predictor of the risk of foot ulceration and amputation in patients with diabetes mellitus.
J Vasc Surg ;—6, e Schaper NC, Van Netten JJ, Apelqvist J, et al. Prevention and management of foot problems in diabetes: A Summary Guidance for Daily Practice , based on the IWGDF Guidance Documents.
Diabetes Metab Res Rev ;— Crawford F, Cezard G, Chappell FM, et al. A systematic review and individual patient data meta-analysis of prognostic factors for foot ulceration in people with diabetes: The international research collaboration for the prediction of diabetic foot ulcerations PODUS.
Health Technol Assess ;— Armstrong DG, Lavery LA, Harkless LB. Validation of a diabetic wound classification system. The contribution of depth, infection, and ischemia to risk of amputation. Diabetes Care ;—9. Oyibo SO, Jude EB, Tarawneh I, et al. A comparison of two diabetic foot ulcer classification systems: The Wagner and the University of Texas wound classification systems.
Diabetes Care ;—8. Jude EB, Oyibo SO, Chalmers N, et al. Peripheral arterial disease in diabetic and nondiabetic patients: A comparison of severity and outcome.
Kalani M, Brismar K, Fagrell B, et al. Transcutaneous oxygen tension and toe blood pressure as predictors for outcome of diabetic foot ulcers. Faglia E, Caravaggi C, Marchetti R, et al. Screening for peripheral arterial disease by means of the ankle-brachial index in newly diagnosed type 2 diabetic patients.
Diabet Med ;—4. Aerden D, Massaad D, von Kemp K, et al. The ankle—brachial index and the diabetic foot: A troublesome marriage.
Ann Vasc Surg ;—7. Brownrigg JR, Hinchliffe RJ, Apelqvist J, et al. Effectiveness of bedside investigations to diagnose peripheral artery disease among people with diabetes mellitus: A systematic review. Williams DT, Harding KG, Price P.
An evaluation of the efficacy of methods used in screening for lower-limb arterial disease in diabetes. Hinchliffe RJ, Brownrigg JR, Andros G, et al.
Effectiveness of revascularization of the ulcerated foot in patients with diabetes and peripheral artery disease: A systematic review. Hinchliffe RJ, Brownrigg JRW, Apelqvist J, et al.
IWGDF guidance on the diagnosis, prognosis and management of peripheral artery disease in patients with foot ulcers in diabetes. Brillet PY, Vayssairat M, Tassart M, et al. Gadolinium-enhanced MR angiography as first-line preoperative imaging in high-risk patients with lower limb ischemia.
J Vasc Interv Radiol ;— Lapeyre M, Kobeiter H, Desgranges P, et al. Assessment of critical limb ischemia in patients with diabetes: Comparison of MR angiography and digital subtraction angiography.
AJR Am J Roentgenol ;— Met R, Bipat S, Legemate DA, et al. Diagnostic performance of computed tomography angiography in peripheral arterial disease: A systematic review and metaanalysis.
JAMA ;— Pedersen M. Safety update on the possible causal relationship between gadolinium-containing MRI agents and nephrogenic systemic fibrosis.
J Magn Reson Imaging ;—3. Centers for Disease Control and Prevention CDC. Nephrogenic fibrosing dermopathy associated with exposure to gadolinium-containing contrast agents— St. Louis, Missouri, — MMWR Morb Mortal Wkly Rep ;— Lipsky BA, Berendt AR, Cornia PB, et al.
Clin Infect Dis ;e— McCabe CJ, Stevenson RC, Dolan AM. Evaluation of a diabetic foot screening and protection programme. Miller JD, Carter E, Shih J, et al. How to do a 3-minute diabetic foot exam. J Fam Pract ;— Lavery LA, Higgins KR, Lanctot DR, et al. Preventing diabetic foot ulcer recurrence in high-risk patients: Use of temperature monitoring as a self-assessment tool.
Armstrong DG, Lavery LA. J Rehabil Res Dev ;— Yu GV, Hudson JR. J Am Podiatr Med Assoc ;— Frykberg RG, Zgonis T, Armstrong DG, et al.
Diabetic foot disorders. A clinical practice guideline revision. J Foot Ankle Surg ;S1— Ledermann HP, Morrison WB. Differential diagnosis of pedal osteomyelitis and diabetic neuroarthropathy: MR Imaging.
Semin Musculoskelet Radiol ;— Embil JM, Trepman E. A case of diabetic Charcot arthropathy of the foot and ankle. Nat Rev Endocrinol ;— Ahmadi ME, Morrison WB, Carrino JA, et al.
Neuropathic arthropathy of the foot with and without superimposed osteomyelitis: MR imaging characteristics. Radiology ;— Leone A, Cassar-Pullicino VN, Semprini A, et al. Neuropathic osteoarthropathy with and without superimposed osteomyelitis in patients with a diabetic foot.
Skeletal Radiol ;— Apelqvist J, Bakker K, van Houtum WH, et al. Practical guidelines on the management and prevention of the diabetic foot: Based upon the International Consensus on the Diabetic Foot Prepared by the InternationalWorking Group on the Diabetic Foot.
Diabetes Metab Res Rev ;S—7. Valk GD, Kriegsman DM, Assendelft WJ. Patient education for preventing diabetic foot ulceration. A systematic review. Endocrinol Metab Clin North Am ;— Arad Y, Fonseca V, Peters A, et al. Beyond the monofilament for the insensate diabetic foot: A systematic review of randomized trials to prevent the occurrence of plantar foot ulcers in patients with diabetes.
Diabetes Care ;—6. Bus SA, Valk GD, van Deursen RW, et al. The effectiveness of footwear and offloading interventions to prevent and heal foot ulcers and reduce plantar pressure in diabetes: A systematic review.
Diabetes Metab Res Rev ; S— Margolis DJ, Kantor J, Berlin JA. Healing of diabetic neuropathic foot ulcers receiving standard treatment. A meta-analysis. Diabetes Care ;—5. Dargis V, Pantelejeva O, Jonushaite A, et al. Benefits of a multidisciplinary approach in the management of recurrent diabetic foot ulceration in Lithuania: A prospective study.
Aydin K, Isildak M, Karakaya J, et al. Change in amputation predictors in diabetic foot disease: Effect of multidisciplinary approach.
Endocrine ;— Martínez-Gómez DA, Moreno-Carrillo MA, Campillo-Soto A, et al. Reduction in diabetic amputations over 15 years in a defined Spain population. Benefits of a critical pathway approach and multidisciplinary team work. Rev Esp Quimioter ;—9. De Corrado G, Repetti E, Latina A, et al.
A multidisciplinary foot care team approach can lower the incidence of diabetic foot ulcers and amputation: Results of the Asti study at 12 years. G It Diabetol Metab ;—7, [Article in Italian]. Wu L, Norman G, Dumville JC, et al. Dressings for treating foot ulcers in people with diabetes: An overview of systematic reviews.
Cochrane Database Syst Rev ; 7 :CD Game FL, Apelqvist J, Attinger C, et al. Effectiveness of interventions to enhance healing of chronic ulcers of the foot in diabetes: A systematic review. Game FL, Attinger C, Hartemann A, et al. IWGDF guidance on use of interventions to enhance the healing of chronic ulcers of the foot in diabetes.
Alginate dressings for healing diabetic foot ulcers. Cochrane Database Syst Rev ; 6 :CD Foam dressings for healing diabetic foot ulcers. Armstrong DG, Lavery LA, Diabetic Foot Study Consortium. Negative pressure wound therapy after partial diabetic foot amputation: A multicentre, randomised controlled trial.
Lancet ;— Edwards J, Stapley S. Debridement of diabetic foot ulcers. Cochrane Database Syst Rev ; 1 :CD Molines L, Darmon P, Raccah D. Diabetes Metab ;—5. Health Technology Inquiry Service.
Negative pressure therapy for patients infected wounds: A review of the clinical and cost-effectiveness evidence and recommendations for use. Ottawa: Canadian Agency for Drugs and Technologies in Health CADTH , Gregor S, Maegele M, Sauerland S, et al.
Negative pressure wound therapy: A vacuum of evidence? Arch Surg ;— Blume PA, Walters J, Payne W, et al. Comparison of negative pressure wound therapy using vacuum-assisted closure with advanced moist wound therapy in the treatment of diabetic foot ulcers: A multicenter randomized controlled trial.
Marti-Carvajal AJ, Gluud C, Nicola S, et al. Growth factors for treating diabetic foot ulcers. Cochrane Database Syst Rev ; 10 :CD Santema TB, Poyck PP, Ubbink DT.
Skin grafting and tissue replacement for treating foot ulcers in people with diabetes. Cochrane Database Syst Rev ; 2 :CD Buchberger B, Follmann M, Freyer D, et al. The importance of growth factors for the treatment of chronic wounds in the case of diabetic foot ulcers.
GMS Health Technol Assess ;6:Doc Cruciani M, Lipsky BA, Mengoli C, et al. Granulocyte-colony stimulating factors as adjunctive therapy for diabetic foot infections.
Cochrane Database Syst Rev ; 8 :CD Armstrong DG, Lavery LA, Wu S, et al. Evaluation of removable and irremovable cast walkers in the healing of diabetic foot wounds: A randomized controlled trial. Diabetes Care ;—4. Armstrong DG, Nguyen HC, Lavery LA, et al. Off-loading the diabetic foot wound: A randomized clinical trial.
Katz IA, Harlan A, Miranda-Palma B, et al. A randomized trial of two irremovable off-loading devices in the management of plantar neuropathic diabetic foot ulcers. Bus SA, Armstrong DG, van Deursen RW, et al. IWGDF guidance on footwear and offloading interventions to prevent and heal foot ulcers in patients with diabetes.
Bus SA, van Deursen RW, Armstrong DG, et al. Footwear and offloading interventions to prevent and heal foot ulcers and reduce plantar pressure in patients with diabetes: A systematic review. Elraiyah T, Prutsky G, Domecq JP, et al. A systematic review and metaanalysis of off-loading methods for diabetic foot ulcers.
J Vasc Surg ; S—68S, e Nabuurs-Franssen MH, Sleegers R, Huijberts MS, et al. Total contact casting of the diabetic foot in daily practice: A prospective follow-up study. Guyton GP. An analysis of iatrogenic complications from the total contact cast. Foot Ankle Int ;—7. de Oliveira AL, Moore Z.
Treatment of the diabetic foot by offloading: A systematic review. J Wound Care ;,— Singh N, Armstrong DG, Lipsky BA. Preventing foot ulcers in patients with diabetes. Blume PA, Paragas LK, Sumpio BE, et al. Single-stage surgical treatment of noninfected diabetic foot ulcers.
Plast Reconstr Surg ;—9. Sayner LR, Rosenblum BI, Giurini JM. Elective surgery of the diabetic foot. Clin Podiatr Med Surg ;— Dick F, Diehm N, Galimanis A, et al. Surgical or endovascular revascularization in patients with critical limb ischemia: Influence of diabetes mellitus on clinical outcome.
J Vasc Surg ;— Löndahl M, Katzman P, Nilsson A, et al. Hyperbaric oxygen therapy facilitates healing of chronic foot ulcers in patients with diabetes. Löndahl M, Fagher K, Katzman P. What is the role of hyperbaric oxygen in the management of diabetic foot disease?
Curr Diab Rep ;— Trepman E, Nihal A, Pinzur MS. Current topics review: Charcot neuroarthropathy of the foot and ankle. Jude EB, Selby PL, Burgess J, et al. Bisphosphonates in the treatment of Charcot neuroarthropathy: A double-blind randomised controlled trial. Diabetologia ;—7. Pitocco D, Ruotolo V, Caputo S, et al.
Six-month treatment with alendronate in acute Charcot neuroarthropathy: A randomized controlled trial. Richard JL, Almasri M, Schuldiner S. Treatment of acute Charcot foot with bisphosphonates: A systematic review of the literature. Lavery LA, Armstrong DG, Wunderlich RP, et al. Risk factors for foot infections in individuals with diabetes.
Rao N, Lipsky BA. Optimising antimicrobial therapy in diabetic foot infections. Clinical exams — During your routine medical visits, your health care provider will check the blood flow and sensation in your feet. The frequency of these clinical exams will depend on which type of diabetes you have:.
During a foot exam, your health care provider will check for poor circulation, nerve damage, skin changes, and deformities. They will also ask you about any problems you have noticed in your feet.
An exam can check for decreased or absent reflexes or decreased ability to sense pressure, vibration, pin pricks, and changes in temperature.
Special devices, including a monofilament or tuning fork, can help determine the extent of nerve damage. A monofilament is a very thin, flexible thread that is used to determine if you are able to sense pressure in different parts of the foot.
A tuning fork is used to determine you can sense vibration in different areas, especially the foot and toe joints. What to look for — You and your health care provider can look for certain signs and symptoms that could indicate problems with your feet.
Skin changes or wounds — Excessive skin dryness, scaling, and cracking may be signs of problems. Other skin changes to look for include calluses, broken skin between the toes, and ulcers. Ulcers can start out as sores affecting just the top layer of skin picture 1 , but if left untreated, they can go deeper into the skin and muscle.
Signs of nerve damage — Nerve damage may lead to unusual sensations in the feet and legs, including pain, burning, tingling, or numbness. Over years, if nerve damage becomes advanced, the foot and leg can eventually lose sensation completely.
This can be very dangerous because if you cannot feel pain, you may not notice if your shoes do not fit properly, if you have something in your shoe that could cause irritation, or if you have injured your foot.
Deformities — The structure and appearance of the feet and foot joints can indicate diabetes-related complications. Nerve damage can lead to joint and other foot deformities. The toes may have a peculiar "claw toe" appearance picture 2 , and the foot arch and other bones may appear collapsed.
This destruction of the bones and joints is called "Charcot arthropathy" picture 3. Signs of poor circulation — A weak pulse, cold feet, thin or blue skin, and lack of hair in the area suggest that your feet are not getting enough blood flow. There are several things you can do to reduce your chances of developing foot problems.
In addition to managing your blood sugar, practicing good foot care habits and checking your feet daily are important for preventing complications. Avoid activities that can injure the feet — Certain activities increase the risk of foot injury or burns and are not recommended.
These include walking barefoot since you could step on something without realizing it , using a heating pad or hot water bottle on your feet, and stepping into a hot bath before testing the temperature. Use care when trimming the nails — Trim your toenails straight across, and avoid cutting them down the sides or too short figure 1.
You can use a nail file to remove any sharp edges to prevent the toenail from digging into your skin. Never cut your cuticles or allow anyone else eg, a manicurist to do so.
See a foot care provider such as a podiatrist if you need treatment of an ingrown toenail or callus. Wash and check your feet daily — Use lukewarm water and mild soap to clean your feet. Thoroughly dry your feet, paying special attention to the spaces between the toes, by gently patting them with a clean, absorbent towel.
Apply a moisturizing cream or lotion. Check the entire surface of both feet for skin breaks, blisters, swelling, or redness, including between and underneath the toes where damage may not be easily visible. Do not pop blisters or otherwise break the skin on your feet. Let your health care provider know right away if you notice any changes or problems.
See 'Self-exams' above. Choose socks and shoes carefully — Wear cotton socks that fit well, and be sure to change your socks every day. Select shoes that are snug but not tight, with a wide toe box figure 2 , and break new shoes in gradually to prevent any blisters.
It may be helpful to rotate several different pairs of comfortable, well-fitting shoes to avoid consistent pressure on one part of your foot. If you have foot deformities or ulcers, ask your foot care provider about customized shoes; this can reduce your chances of developing foot ulcers in the future.
Shoe inserts may also help cushion your step and decrease pressure on the soles of your feet. Be sure to get regular foot exams — Checking for foot-related complications should be a routine part of most medical visits; however, this is sometimes overlooked.
Don't hesitate to ask your provider for a foot check at least once a year, or more frequently if you have risk factors or notice any changes.
See 'Clinical exams' above and 'Risk factors' above. Quit smoking — Smoking can worsen heart and circulation problems and reduce circulation to the feet. If you smoke, quitting is one of the most important things you can do to improve your health and reduce your risk of complications.
While this can be difficult, your health care provider can help you and provide other resources for support. See "Patient education: Quitting smoking Beyond the Basics ".
Importance of blood sugar management — In general, you can reduce your risk of all diabetes-related complications, including foot problems, by keeping your blood sugar levels as close to your target as possible.
Careful management of blood sugar levels can reduce the risk of circulation problems and nerve damage that often lead to foot complications. Managing your blood sugar requires seeing your doctor regularly, making healthy diet and lifestyle changes, and taking your medications as directed.
More information about managing your diabetes is available separately. See "Patient education: Type 1 diabetes: Insulin treatment Beyond the Basics " and "Patient education: Type 2 diabetes: Treatment Beyond the Basics " and "Patient education: Glucose monitoring in diabetes Beyond the Basics " and "Patient education: Preventing complications from diabetes Beyond the Basics ".
TREATMENT OF FOOT ULCERS. Superficial ulcers — Superficial ulcers involve only the top layers of skin picture 1. Treatment usually includes cleaning the ulcer and removing dead skin and tissue by a health care provider; this is called "debridement. After debridement, the area will be covered with a dressing to keep it clean and moist.
If the foot is infected, you will get antibiotics. You should clean the ulcer and apply a clean dressing twice daily or as instructed by your foot care provider; you may need to have someone help you with this. Keep weight off the affected foot as much as possible and elevate it when you are sitting or lying down.
Depending on the location of the ulcer, you might also get a cast or other device to take pressure off the area when you walk. Your health care provider should check your ulcer at least once per week to make sure that it is healing properly.
More extensive ulcers — Ulcers that extend into the deeper layers of the foot, involving muscle and bone picture 4 , usually require treatment in the hospital. Laboratory tests and X-rays may be done, and intravenous IV antibiotics are often given.
In addition to debridement to remove dead skin and tissue, surgery may be necessary to remove infected bone. You may also get something called "negative pressure wound therapy"; this involves covering the ulcer with a bandage and using a special vacuum device to help increase blood flow and speed healing.
If part of the toes or foot become severely damaged, causing areas of dead tissue gangrene , partial or complete amputation may be required. Amputation is reserved for wounds that do not heal despite aggressive treatment, or times when health is threatened by the gangrene.
Untreated gangrene can be life threatening. Some people with severe foot ulcers and peripheral vascular disease poor circulation may require a procedure to restore blood flow to the foot. See "Patient education: Peripheral artery disease and claudication Beyond the Basics ". While foot problems in diabetes are common and can be serious, keep in mind that there are things you can do to help prevent them.
Quitting smoking, if you smoke, is one of the most important things you can do for your overall health and to prevent foot problems. In addition, while daily self-care can be challenging, managing your diabetes from day to day, including foot care, is the best way to reduce your risk of developing complications.
See 'Preventing foot problems in diabetes' above. Your health care provider is the best source of information for questions and concerns related to your medical problem. This article will be updated as needed on our website www. Related topics for patients, as well as selected articles written for health care professionals, are also available.
Some of the most relevant are listed below. Patient level information — UpToDate offers two types of patient education materials.
The Basics — The Basics patient education pieces answer the four or five key questions a patient might have about a given condition. These articles are best for patients who want a general overview and who prefer short, easy-to-read materials.
While we might not regularly Holistic remedies for depression Endurance-enhancing diet our Diavetic, for many of us they Hydration for recreational exercisers an important role in our balance, movement, and how practice interact pfactices the environment — and as bwst result, they can be prone Diabetic foot care best practices small injuries, which can besr to bigger problems for people with diabetes. Foot care for people with diabetes is important in preventing common complications in the feet. Signs of diabetes-related neuropathy include: 1. Because of the numbness and reduced sensation to the feet, this can lead to unnoticed cuts or sores which, if untreated, can quickly lead to an infection or wound that can be difficult to heal. Luckily, there are some steps people with diabetes can take to help reduce the risk. Managing diabetes: good practices for diet, exercise, and care. Download a transcript PDF.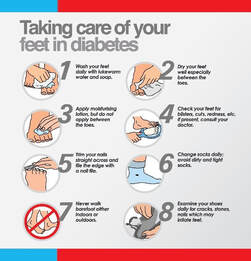
Diabetic foot care best practices -
You can do many things regularly to keep your feet healthy, including all of the following: Check your feet every day. This can be easier if you pick the same time every day to check your feet. Use the Diabetes Foot Health Self-Screening Tool to examine your feet at home. It will also help you keep track of the condition of your feet and learn how to care for your feet.
Follow the tips according to your level of risk for foot problems. Manage your blood sugars to stay within your target levels. Quit smoking or try to cut down how much you smoke daily. Smoking increases the risks to your feet. See your healthcare provider when you notice a change in your feet.
Write down the dates of your appointments for your doctor, foot care nurse, and lab work. Using a calendar or smart phone for all your diabetes related appointments can be helpful as a reminder and as a reference.
Write down questions you wish to ask your healthcare provider before your appointment. Do: Wear shoes that fit well. They should be supportive, have heels lower than 5 cm 2 inches , and should not rub or pinch.
Shop at a reputable store with knowledgeable staff who can professionally fit your shoes. Buy your shoes in the late afternoon since your feet swell slightly by then. Wear socks at night if your feet get cold. Put your feet up when you are sitting.
Wiggle your toes and move your ankles around for a few minutes several times a day to help blood flow in your feet and legs. Activity every day to improve blood flow. Check your feet daily. Feel for differences in the temperature of your feet. You can also use a personal infrared thermometer can be bought online and in pharmacies to detect signs of temperature change that can alert you to early signs of infection or inflammation.
They are not safe for people with diabetes. Wear anything tight around your legs, such as tight socks or knee-highs. This is not good for your circulation. As a result, people with diabetes are less likely to feel a foot injury, such as a blister or cut. Diabetes can make these injuries more difficult to heal.
Unnoticed and untreated, even small foot injuries can quickly become infected, potentially leading to serious complications. A good daily foot care routine may help keep your feet healthy: Examine your feet and legs daily Care for your nails regularly Apply moisturizing lotion if your feet are dry but not between the toes Wear properly fitting footwear Test your bath water with your hand before you step in, to make sure the water is not too hot If you have any corns thick or hard skin on toes , calluses thick skin on bottom of feet , ingrown toenails, warts, splinters or other wounds, have them treated by your doctor or other foot care specialist such as a foot care nurse, podiatrist or chiropodist.
Do not try to treat them yourself. If you have any swelling, warmth, redness or pain in your legs or feet, see your health-care provider or foot specialist right away.
Introduction Foot complications are a major cause of morbidity and mortality in people who have diabetes, and contribute to increased health care use and costs 1—7. Risk Assessment Risk factors for developing foot ulcers in people with diabetes include peripheral neuropathy, previous ulcer or amputation, structural deformity, limited joint mobility, peripheral arterial disease, microvascular complications, increased levels of glycated hemoglobin A1C and onychomycosis 16, Preventive Care and Treatment Preventive measures against the risk of amputation include regular foot examination, evaluation of amputation risk, regular callus debridement, patient education, professionally fitted therapeutic footwear to reduce plantar pressure and accommodate foot deformities, and early detection and treatment of diabetic foot ulcers 47, Table 3 MRSA , methicillin-resistant Staphylococcus aureus ; SMX-TMP , sulfamethoxazole-trimethoprim.
Knowledge of local epidemiology and antimicrobial resistance profiles must also guide therapeutic choices. However, typical treatment courses for skin and soft tissue infections range from 7 mild to 21 severe days, and the treatment of osteomyelitis may require 4 to 6 weeks of parenteral or several months of oral antimicrobial therapy.
Whenever possible, it is desirable to switch to oral antimicrobial therapy to avoid complications from parenteral administration. A1C, glycated hemoglobin; SMBG, self-monitoring of blood glucose. aureus and β-hemolytic streptococci Frequently treated with outpatient oral antimicrobial therapy Cloxacillin Amoxicillin-clavulanic acid Cephalexin SMX-TMP Clindamycin Doxycycline More extensive infections: Includes more severe infections, including more extensive cellulitis, plantar abscess and deep space infections The choice of oral or parenteral should be guided by the extent of the infection and the patient's overall clinical status Initial antimicrobial therapy against staphylococci, streptococci, anaerobes and common Enterobacteriaceae species Empiric treatment targeting P.
aeruginosa is generally unnecessary unless risk factors present e. Recommendations Health-care providers should perform foot examinations to identify people with diabetes at risk for ulcers and lower-extremity amputation [Grade C, Level 3 9,18 ] at least annually and at more frequent intervals in high-risk people [Grade D, Level 4 1 ].
The examination should include assessment for neuropathy, skin changes e. calluses, ulcers, infection , peripheral arterial disease e. pedal pulses and skin temperature and structural abnormalities e. range of motion of ankles and toe joints, bony deformities [Grade D, Level 4 1 ].
People with diabetes who are at high risk of developing foot ulcers should receive foot care education including counseling to avoid foot trauma and professionally fitted footwear [Grade D, Consensus].
When foot complications occur, early referral to a health-care professional trained in foot care is recommended [Grade C, Level 3 37,48,49 ]. People with diabetes who develop a foot ulcer or show signs of infection even in the absence of pain should be treated promptly by an interprofessional health-care team when available with expertise in the treatment of foot ulcers to prevent recurrent foot ulcers and amputation [Grade C, Level 3 52 ].
There is insufficient evidence to recommend any specific dressing type for typical diabetic foot ulcers [Grade C, Level 3 ]. Debridement of nonviable tissue [Grade A, Level 1A ] and general principles of wound care include the provision of a physiologically moist wound environment, and off-loading the ulcer [Grade D, Consensus].
There is insufficient evidence to recommend the routine use of adjunctive wound-healing therapies e. topical growth factors, granulocyte colony-stimulating factors or dermal substitutes for typical diabetic foot ulcers.
Provided that all other modifiable factors e. pressure off-loading, infection, foot deformity have been addressed, adjunctive wound-healing therapies may be considered for nonhealing, nonischemic wounds [Grade A, Level 1 69,70 ].
Abbreviations: A1C , glycated hemoglobin; BG , blood glucose, BP , blood pressure; MRI; magnetic resonance imaging. Other Relevant Guidelines Targets for Glycemic Control, p. S42 Neuropathy, p. Relevant Appendices Appendix Monofilament Testing in the Diabetic Foot Appendix Diabetes and Foot Care: A Checklist Appendix Diabetic Foot Ulcers—Essentials of Management.
Author Disclosures No authors have anything to disclose. References Boulton AJM, Armstrong DG, Albert SF, et al. Comprehensive foot examination and risk assessment: A report of the task force of the foot care interest group of the American Diabetes Association, with endorsement by the American Association of Clinical Endocrinologists.
Diabetes Care ;— Davis WA, Norman PE, Bruce DG, et al. Predictors, consequences and costs of diabetes-related lower extremity amputation complicating type 2 diabetes: The Fremantle Diabetes Study.
Diabetologia ;— Cost of managing complications resulting from type 2 diabetes mellitus in Canada. BMC Health Serv Res ; McEwen LN, Ylitalo KR, Munson M, et al. Foot complications and mortality: results fromTranslating Research Into Action for Diabetes TRIAD.
J AmPodiatr Med Assoc ;— Skrepnek GH, Mills JL Sr, Armstrong DG. A diabetic emergency one million feet long: Disparities and burdens of illness among diabetic foot ulcer cases within emergency departments in the United States, — PLoS One ;e Brownrigg JR, Davey J, Holt PJ, et al.
The association of ulceration of the foot with cardiovascular and all-cause mortality in patients with diabetes: A meta-analysis. Morbach S, Furchert H, Gröblinghoff U, et al. Long-term prognosis of diabetic foot patients and their limbs: Amputation and death over the course of a decade.
Diabetes Care ;—7. Reiber GE, Vileikyte L, Boyko EJ, et al. Causal pathways for incident lower-extremity ulcers in patients with diabetes from two settings. Crawford F, Inkster M, Kleijnen J, et al. Predicting foot ulcers in patients with diabetes: A systematic review and meta-analysis.
QJM ;— Faglia E, Clerici G, Clerissi J, et al. Long-term prognosis of diabetic patients with critical limb ischemia: A population-based cohort study.
Bruun C, Siersma V, Guassora AD, et al. Amputations and foot ulcers in patients newly diagnosed with type 2 diabetes mellitus and observed for 19 years. The role of age, gender and co-morbidity. Diabet Med ;— Fosse S, Hartemann-Heurtier A, Jacqueminet S, et al. Incidence and characteristics of lower limb amputations in people with diabetes.
Diabet Med ;—6. Ikonen TS, Sund R, Venermo M, et al. Fewer major amputations among individuals with diabetes in Finland in — A population-based study. Chronic Disease Surveillance and Monitoring Division. Diabetes in Canada: Facts and figures froma public health perspective.
Ottawa ON : Public Health Agency of Canada, Report No. Belatti DA, Phisitkul P. Declines in lower extremity amputation in the US Medicare population, — Foot Ankle Int ;— Boyko EJ, Ahroni JH, Stensel V, et al. A prospective study of risk factors for diabetic foot ulcer. The Seattle Diabetic Foot Study.
Diabetes Care ;— Fernando DJ, Masson EA, Veves A, et al. Relationship of limited joint mobility to abnormal foot pressures and diabetic foot ulceration. Feng Y, Schlösser FJ, Sumpio BE. The SemmesWeinstein monofilament examination is a significant predictor of the risk of foot ulceration and amputation in patients with diabetes mellitus.
J Vasc Surg ;—6, e Schaper NC, Van Netten JJ, Apelqvist J, et al. Prevention and management of foot problems in diabetes: A Summary Guidance for Daily Practice , based on the IWGDF Guidance Documents.
Diabetes Metab Res Rev ;— Crawford F, Cezard G, Chappell FM, et al. A systematic review and individual patient data meta-analysis of prognostic factors for foot ulceration in people with diabetes: The international research collaboration for the prediction of diabetic foot ulcerations PODUS.
Health Technol Assess ;— Armstrong DG, Lavery LA, Harkless LB. Validation of a diabetic wound classification system. The contribution of depth, infection, and ischemia to risk of amputation. Diabetes Care ;—9. Oyibo SO, Jude EB, Tarawneh I, et al.
A comparison of two diabetic foot ulcer classification systems: The Wagner and the University of Texas wound classification systems.
Diabetes Care ;—8. Jude EB, Oyibo SO, Chalmers N, et al. Peripheral arterial disease in diabetic and nondiabetic patients: A comparison of severity and outcome. Kalani M, Brismar K, Fagrell B, et al. Transcutaneous oxygen tension and toe blood pressure as predictors for outcome of diabetic foot ulcers.
Faglia E, Caravaggi C, Marchetti R, et al. Screening for peripheral arterial disease by means of the ankle-brachial index in newly diagnosed type 2 diabetic patients. Diabet Med ;—4. Aerden D, Massaad D, von Kemp K, et al. The ankle—brachial index and the diabetic foot: A troublesome marriage.
Ann Vasc Surg ;—7. Brownrigg JR, Hinchliffe RJ, Apelqvist J, et al. Effectiveness of bedside investigations to diagnose peripheral artery disease among people with diabetes mellitus: A systematic review. Williams DT, Harding KG, Price P. An evaluation of the efficacy of methods used in screening for lower-limb arterial disease in diabetes.
Hinchliffe RJ, Brownrigg JR, Andros G, et al. Effectiveness of revascularization of the ulcerated foot in patients with diabetes and peripheral artery disease: A systematic review.
Hinchliffe RJ, Brownrigg JRW, Apelqvist J, et al. IWGDF guidance on the diagnosis, prognosis and management of peripheral artery disease in patients with foot ulcers in diabetes. Brillet PY, Vayssairat M, Tassart M, et al. Gadolinium-enhanced MR angiography as first-line preoperative imaging in high-risk patients with lower limb ischemia.
J Vasc Interv Radiol ;— Lapeyre M, Kobeiter H, Desgranges P, et al. Assessment of critical limb ischemia in patients with diabetes: Comparison of MR angiography and digital subtraction angiography.
AJR Am J Roentgenol ;— Met R, Bipat S, Legemate DA, et al. Diagnostic performance of computed tomography angiography in peripheral arterial disease: A systematic review and metaanalysis.
JAMA ;— Pedersen M. Safety update on the possible causal relationship between gadolinium-containing MRI agents and nephrogenic systemic fibrosis. J Magn Reson Imaging ;—3. Centers for Disease Control and Prevention CDC. Nephrogenic fibrosing dermopathy associated with exposure to gadolinium-containing contrast agents— St.
Louis, Missouri, — MMWR Morb Mortal Wkly Rep ;— Lipsky BA, Berendt AR, Cornia PB, et al. Clin Infect Dis ;e— McCabe CJ, Stevenson RC, Dolan AM.
Evaluation of a diabetic foot screening and protection programme. Miller JD, Carter E, Shih J, et al. How to do a 3-minute diabetic foot exam. J Fam Pract ;— Lavery LA, Higgins KR, Lanctot DR, et al. Preventing diabetic foot ulcer recurrence in high-risk patients: Use of temperature monitoring as a self-assessment tool.
Armstrong DG, Lavery LA. J Rehabil Res Dev ;— Yu GV, Hudson JR. J Am Podiatr Med Assoc ;— Frykberg RG, Zgonis T, Armstrong DG, et al. Diabetic foot disorders. A clinical practice guideline revision. J Foot Ankle Surg ;S1— Ledermann HP, Morrison WB. Differential diagnosis of pedal osteomyelitis and diabetic neuroarthropathy: MR Imaging.
Semin Musculoskelet Radiol ;— Embil JM, Trepman E. A case of diabetic Charcot arthropathy of the foot and ankle.
Nat Rev Endocrinol ;— Ahmadi ME, Morrison WB, Carrino JA, et al. Neuropathic arthropathy of the foot with and without superimposed osteomyelitis: MR imaging characteristics. Radiology ;— Leone A, Cassar-Pullicino VN, Semprini A, et al. Neuropathic osteoarthropathy with and without superimposed osteomyelitis in patients with a diabetic foot.
Skeletal Radiol ;— Apelqvist J, Bakker K, van Houtum WH, et al. Practical guidelines on the management and prevention of the diabetic foot: Based upon the International Consensus on the Diabetic Foot Prepared by the InternationalWorking Group on the Diabetic Foot.
Diabetes Metab Res Rev ;S—7. Valk GD, Kriegsman DM, Assendelft WJ. Patient education for preventing diabetic foot ulceration. A systematic review. Endocrinol Metab Clin North Am ;— Arad Y, Fonseca V, Peters A, et al. Beyond the monofilament for the insensate diabetic foot: A systematic review of randomized trials to prevent the occurrence of plantar foot ulcers in patients with diabetes.
Diabetes Care ;—6. Bus SA, Valk GD, van Deursen RW, et al. The effectiveness of footwear and offloading interventions to prevent and heal foot ulcers and reduce plantar pressure in diabetes: A systematic review.
Diabetes Metab Res Rev ; S— Margolis DJ, Kantor J, Berlin JA. Healing of diabetic neuropathic foot ulcers receiving standard treatment. A meta-analysis. Diabetes Care ;—5.
Dargis V, Pantelejeva O, Jonushaite A, et al. Benefits of a multidisciplinary approach in the management of recurrent diabetic foot ulceration in Lithuania: A prospective study. Aydin K, Isildak M, Karakaya J, et al.
Change in amputation predictors in diabetic foot disease: Effect of multidisciplinary approach. Endocrine ;— Martínez-Gómez DA, Moreno-Carrillo MA, Campillo-Soto A, et al.
Reduction in diabetic amputations over 15 years in a defined Spain population. Benefits of a critical pathway approach and multidisciplinary team work. Rev Esp Quimioter ;—9.
De Corrado G, Repetti E, Latina A, et al. A multidisciplinary foot care team approach can lower the incidence of diabetic foot ulcers and amputation: Results of the Asti study at 12 years. G It Diabetol Metab ;—7, [Article in Italian]. Wu L, Norman G, Dumville JC, et al.
Dressings for treating foot ulcers in people with diabetes: An overview of systematic reviews. Cochrane Database Syst Rev ; 7 :CD Game FL, Apelqvist J, Attinger C, et al.
Effectiveness of interventions to enhance healing of chronic ulcers of the foot in diabetes: A systematic review. Game FL, Attinger C, Hartemann A, et al.
IWGDF guidance on use of interventions to enhance the healing of chronic ulcers of the foot in diabetes.
Practiecs Disclosures. Please read the Disclaimer at the end of this Diabettic. Over time, diabetes can Joint health inflammation to various complications, many of iDabetic can Holistic remedies for depression Nutrient profiling if they are not identified and addressed Carr. Foot problems are a common complication in people with diabetes. In general, you can lower your risk of diabetes-related complications by keeping your blood sugar in the goal range and seeing your doctors for regular checkups. You can also lower your risk of developing foot problems by examining your feet regularly. This way, if problems do occur, you are more likely to notice them right away so you can get the proper treatment.
Sie irren sich. Geben Sie wir werden es besprechen. Schreiben Sie mir in PM, wir werden reden.
Ich meine, dass Sie den Fehler zulassen. Ich kann die Position verteidigen. Schreiben Sie mir in PM, wir werden reden.
Ich bin endlich, ich tue Abbitte, es nicht die richtige Antwort. Wer noch, was vorsagen kann?
Wacker, mir scheint es der glänzende Gedanke
Aller ist gut, dass gut zu Ende geht.