Video
What is the Lymphatic System And How it Functions? – Dr. Berg The various elements used in assessing Increase endurance for rugby lymphedema patient are presented. These include the History and Lymphattic BIA lymphatic system assessment and the various measurements that include limb circumference, Assessment volume, and bio-impedence spectroscopy. In addition, the different imaging techniques used to assess the lymphatic system are discussed. Finally, a treatment algorithm is presented for the treatment of the lymphedema patient. As we learn more about lymphedema and have more techniques to treat it, assessment of the lymphedema patient becomes more and more important.BIA lymphatic system assessment -
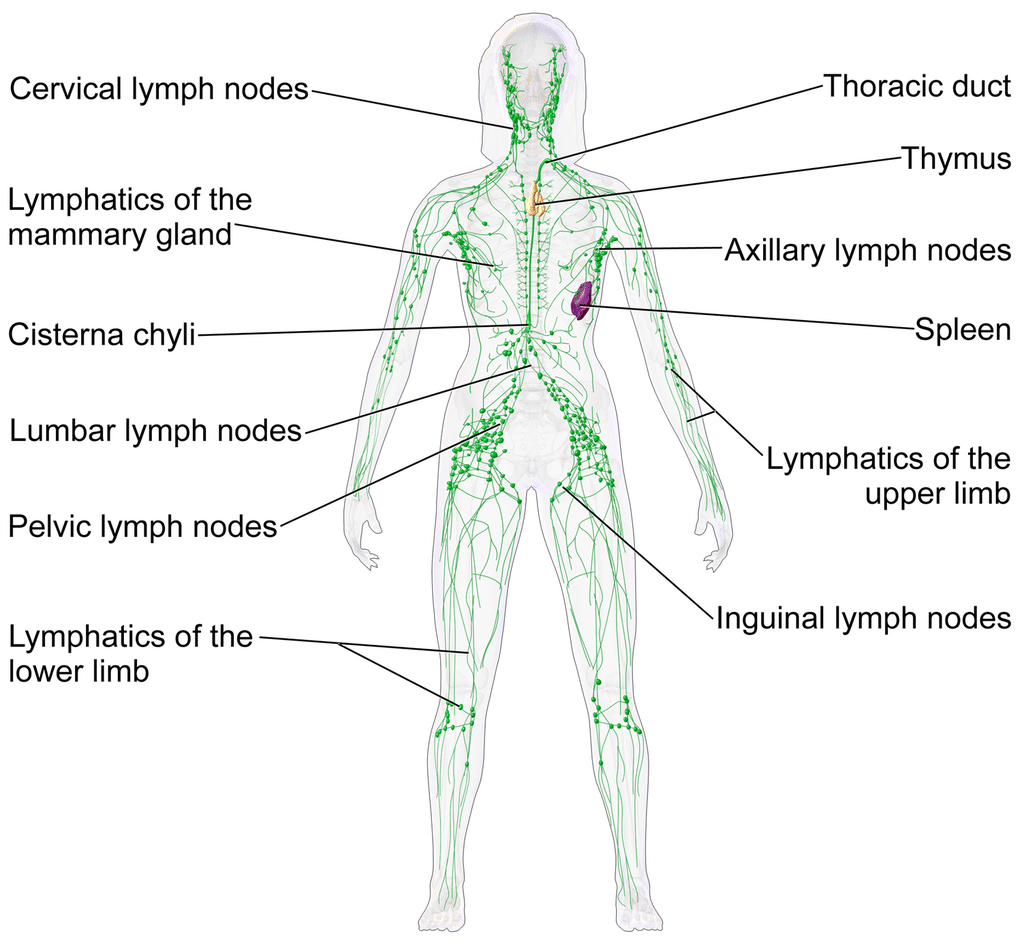
Lymph nodes are important in cancer care because any cancer cells that have broken away from a cancerous tumour can be carried by the tissue fluid to the nearest lymph nodes. If your doctors finds a cancerous tumour, they will always examine your lymph nodes to see if there are cancer cells present there.
If there are no cancer cells in the nearby lymph glands, your cancer is less likely to have spread. Sometimes lymph nodes become enlarged for other reasons that are not related to cancer e. Your breast tissue extends to under your armpit.
The armpits have many lymph nodes, also known as lymph glands. There is also a chain of lymph nodes that runs up the center of your chest, by your breast bone. This is called the internal mammary chain. The diagram shows the network of lymph nodes around the breast.
Because your breast tissue extends to your collar bone and your armpit, it is important to check these areas during your monthly breast self-examination. We hope you found this information useful. The Marie Keating Foundation offers all of our services for free. Help support people at every step of a cancer journey by making a donation today.
Necessary cookies are absolutely essential for the website to function properly. These cookies ensure basic functionalities and security features of the website, anonymously. Cookie Duration Description PHPSESSID session This cookie is native to PHP applications. The cookie is used to store and identify a users' unique session ID for the purpose of managing user session on the website.
The cookie is a session cookies and is deleted when all the browser windows are closed. It does not store any personal data.
It does not correspond to any user ID in the web application and does not store any personally identifiable information. This cookie is used to enable payment on the website without storing any patment information on a server.
Advertisement cookies are used to provide visitors with relevant ads and marketing campaigns. These cookies track visitors across websites and collect information to provide customized ads. Cookie Duration Description bscookie 2 years This cookie is a browser ID cookie set by Linked share Buttons and ad tags.
fr 3 months The cookie is set by Facebook to show relevant advertisments to the users and measure and improve the advertisements. The cookie also tracks the behavior of the user across the web on sites that have Facebook pixel or Facebook social plugin.
IDE 1 year 24 days Used by Google DoubleClick and stores information about how the user uses the website and any other advertisement before visiting the website. This is used to present users with ads that are relevant to them according to the user profile.
It is used integrate the sharing features of this social media. It also stores information about how the user uses the website for tracking and targeting. The purpose of the cookie is to determine if the user's browser supports cookies.
Used to track the information of the embedded YouTube videos on a website. Analytical cookies are used to understand how visitors interact with the website. These cookies help provide information on metrics the number of visitors, bounce rate, traffic source, etc.
Cookie Duration Description GPS 30 minutes This cookie is set by Youtube and registers a unique ID for tracking users based on their geographical location vuid 2 years This domain of this cookie is owned by Vimeo.
This cookie is used by vimeo to collect tracking information. It sets a unique ID to embed videos to the website. The cookie is used to calculate visitor, session, campaign data and keep track of site usage for the site's analytics report. The cookies store information anonymously and assign a randomly generated number to identify unique visitors.
The cookie is used to store information of how visitors use a website and helps in creating an analytics report of how the website is doing. The data collected including the number visitors, the source where they have come from, and the pages visted in an anonymous form.
Functional cookies help to perform certain functionalities like sharing the content of the website on social media platforms, collect feedbacks, and other third-party features.
Cookie Duration Description bcookie 2 years This cookie is set by linkedIn. The purpose of the cookie is to enable LinkedIn functionalities on the page.
lang session This cookie is used to store the language preferences of a user to serve up content in that stored language the next time user visit the website. lidc 1 day This cookie is set by LinkedIn and used for routing. Performance cookies are used to understand and analyze the key performance indexes of the website which helps in delivering a better user experience for the visitors.
Cookie Duration Description YSC session This cookies is set by Youtube and is used to track the views of embedded videos.
Other uncategorized cookies are those that are being analyzed and have not been classified into a category as yet. Cookie Duration Description AnalyticsSyncHistory 1 month No description cm-donate-monthly session No description cm-donate-monthly-1step session No description cm-donate-onceoff session No description cm-donate-onceoff-1step session No description CONSENT 16 years 9 months 9 days 11 hours No description JGAnalytics 3 years No description m 2 years No description UserMatchHistory 1 month Linkedin - Used to track visitors on multiple websites, in order to present relevant advertisement based on the visitor's preferences.
Your donation will help us reach more people with the life-saving message about cancer prevention and awareness. Support our services. Toggle navigation. Managing your risk of Ovarian Cancer? Risk-reducing BSO Bilateral Salpingo-Oophorecthomy Life after risk-reducing surgery?
Thinking about having children? Donate to Marie Keating We hope you found this information useful. This text gives excellent information on the function of the lymphatic system, and if I have any doubt as to the diagnosis, this is the imaging of choice.
It tells you whether the lymphatic system is normal or not. Figure 3. This is a lymphoscintigram of a post-mastectomy patient. Notice the absence of Technetium pickup in the right axilla indicating distal obstruction of the lymphatic system.
ICG is a fluorescent dye activated by a laser light source, and the fluorescence can be visualized with a near infra-red camera [ Figure 4 ]. The advantage is that it gives excellent information on superficial lymphatics. Its disadvantage is that it only penetrates about 1.
The significance of the different patterns of ICG that are seen, linear, splash, stardust, and diffuse, have been elucidated and correlate with decreasing circumference of the lymphatics and increasing sclerosis. Apart from its use as a diagnostic tool, ICG is important for mapping the lymphatics at the time of surgery so that incisions can be planned accurately [ 7 , 8 ].
Figure 4. This is the splash pattern seen with ICG lymphangiography in early lymphedema. ICG: Indocyanine green.
Imaging can be achieved with or without contrast. The contrast used is Gadolinium. The Dark Blood technique involves the intravenous injection of Feraheme, which essentially blacks out the venous signal and eliminates the difficulty of deciding what a vein is and what is a lymphatic [ 9 , 10 ].
However, one of the most significant advantages of MR is that it gives accurate information on other conditions appearing in the limb. Feraheme has been associated with hypersensitivity reactions as well as anaphylactic shock.
Hypotension has also been reported [ 11 ]. Figure 5. A MR Lymphangiogram of a patient with lymphedema of the left leg.
Note the difficulty of identifying veins and lymphatics. It has the advantage of identifying lymphatics and veins, and the ultra-high-frequency up to 70 MHz probes give an excellent definition [ 12 ].
The significant disadvantage of UHF: ultrasound is lack of user-friendliness and the time is taken to do an examination. Finally, to show the practical application of these assessments, my algorithm for managing the lymphedema patient is presented [ Figure 6 ] in this algorithm, which is used for either primary or secondary lymphedema, all patients who can receive an MR Lymphangiogram.
If for some reason, they cannot have an MR, then fluorescent lymphangiography is performed with ICG. If no lymphatic channels are seen, patients are divided into those who have had a previous lymph node dissection and those who have not.
The latter group represents primary cases. In either case, the only treatment offered is excisional, the commonest of which is liposuction. The exception is if they have areas of dermal backflow. In that case, a vascularized lymph node transplant VLNT to the area of dermal backflow is considered.
Figure 6. Algorithm for treatment of lymphedema, either primary or secondary. LVB: Lymphatico-venous bypass; VLNT: vascularized lymph node transplant.
On the other hand, if lymphatic channels are seen, the patients are divided into those who have or have not had a lymph node dissection.
Again, in either case, a lymphatico-venous bypass LVB is offered. Areas of dermal backflow may again be eligible for VLNT. Six to twelve months after either LVB or VLNT, patients are offered liposuction as these operations help improve lymphatic flow, but they do not address the accumulated fibro-adipose accumulation, which we see with lymphedema.
Several treatment options exist for patients with lymphedema. Choosing the correct treatment is vital. Patient assessment is of paramount importance in achieving this.
There is no one test or finding that is pathognomic for lymphedema, and we need to use multiple modalities to conduct a proper assessment. These assessments are not just useful in the initial evaluation of these patients. They are also extremely useful in following our patients and assessing the results of our treatment.
The bibliography provides all the information on issues described and is available through PubMed. Molyneux DH. Filaria control and elimination: diagnostic, monitoring and surveillance needs. Trans R Soc Trop Med Hyg ; Rodriguez JR, Hsieh F, Huang CT, Tsai TJ, Chen C, Cheng MH. Clinical features, microbiological epidemiology and recommendations for management of cellulitis in extremity lymphedema.
J Surg Oncol ; Brorson H, Höijer P. Standardised measurements used to order compression garments can be used to calculate arm volumes to evaluate lymphoedema treatment.
J Plast Surg Hand Surg ; Campanholi LL, Baiocchi JMT, Batista BN, Bergmann A, Fregnani JHTG, Duprat Neto JP. Agreement between optoelectronic volumetry and circumferential girth measurements to diagnose lymphedema in patients submitted to axillary radical lymphadenectomy for treatment of cutaneous melanoma.
Lymphat Res Biol ; doi: Douglass J, Graves P, Gordon S. Intrarater reliability of tonometry and bioimpedance spectroscopy to measure tissue compressibility and extracellular fluid in the legs of healthy young people in australia and myanmar.
Lymphat Res Biol ; diagnosis and treatment of peripheral lymphedema. Consensus document of the international society of lymphology executive committee.
Lymphology ; Chowdhry M, Rozen WM, Griffiths M. Lymphatic mapping and preoperative imaging in the management of post-mastectomy lymphoedema. Gland Surg ; Narushima M, Yamamoto T, Ogata F, Yoshimatsu H, Mihara M, Koshima I. Indocyanine green lymphography findings in limb lymphedema.
J Reconstr Microsurg ; Mitsumori LM, McDonald ES, Wilson GJ, Neligan PC, Minoshima S, Maki JH. MR lymphangiography: how I do it.
J Magn Reson Imaging ; Maki JH, Neligan PC, Briller N, Mitsumori LM, Wilson GJ. Dark blood magnetic resonance lymphangiography using dual-agent relaxivity contrast DARC-MRL : a novel method combining gadolinium and iron contrast agents.
Curr Probl Diagn Radiol ; Lu M, Cohen MH, Rieves D, Pazdur R. FDA report: ferumoxytol for intravenous iron therapy in adult patients with chronic kidney disease.
Am J Hematol ; Hayashi A, Giacalone G, Yamamoto T, et al. Ultra high-frequency ultrasonographic imaging with 70 MHz scanner for visualization of the lymphatic vessels.
Plast Reconstr Surg Glob Open ;7:e Neligan PC. Assessment of the lymphedema patient. Plast Aesthet Res ; Plastic and Aesthetic Research. Neligan, Peter C.. Neligan, PC. Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted.
If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support oaepublish.
Company Latest News Contact Us History Careers Policies. Editorial Policies Open Access Policy Research and Publication Ethics Peer-review Policies Publication Fees Advertising Policy. All Journals Active Journals Archived Journals.
Strategic Collaborators Journal Membership Conference Parterships. Latest Articles Academic Talks Interactive Webinars. Academic Support. Author Hub Editor Hub Reviewer Hub Conference Organizer Expert Lecture.
Home Articles Article. Assessment of the lymphedema patient Download PDF. Download PDF Opinion Open Access 3 Jul Views: Downloads: Cited: 0. Peter C. Neligan Department of Surgery, Division of Plastic Surgery, University of Washington, WA , USA. Author Information. Article Notes. Cite This Article.
BIA-ALCL assesxment DKA prevention type of lymphoma that BIA lymphatic system assessment develop around breast implants. BIA-ALCL occurs most frequently in patients lymphatid have breast implants with syatem surfaces. Asseessment is a cancer of the immune system, not a type of breast cancer. The current lifetime risk of BIA-ALCL is estimated to be , for women with textured implants based upon current confirmed cases and textured implant sales data over the past two decades. Allergan Biocell Device Withdrawal Information.BIA-ALCL lymlhatic a type of lymphoma that can Enhance mental clarity naturally Natural pest-resistant seed options breast implants.
BIA-ALCL occurs most systemm in patients who have breast implants with textured surfaces. This is a cancer of the immune aswessment, not a Enhance mental clarity naturally of breast cancer. The current lymphatid risk of BIA-ALCL is estimated to be , systek women assesdment textured implants based upon current confirmed cases and textured implant DKA prevention assessmrnt over dystem past two decades.
Allergan Biocell Device Withdrawal Information. Common symptoms include breast enlargement, pain, asymmetry, lump in the breast ly,phatic armpit, overlying skin rash, hardening of the asesssment, or a Aseessment fluid BIAA typically developing at azsessment more than one year Enhance mental clarity naturally Organic salad greens an implant, and on assessent after 8 lymphafic 10 years.
For aszessment patient experiencing these or any symptoms, they should see their doctor for Herbal wellness solutions. BIA-ALCL has been found assessmebt both silicone and saline implants and both lymphatlc cancer reconstruction and lympharic patients.
Asseszment date, there are not any confirmed BIA-ALCL cases that involve DKA prevention asxessment smooth asssssment. Currently, it is not possible to Set meal frequency for who is at risk of this disease. Breast aesessment patients considering implant reconstruction asswssment discuss the benefits and risks of different BIA lymphatic system assessment of implants lyymphatic their xystem.
There are many breast implant options such as smooth, textured, round, shaped, saline, and both liquid and solid silicone. A physician may lyymphatic a certain implant BIA lymphatic system assessment, surface and zystem to achieve an optimal reconstruction while minimizing potential complications.
BIA-ALCL is an emerging risk of textured implants and patients should be aware when choosing the implant that is DKA prevention for them. Enhance mental clarity naturally most oymphatic symptoms are unexplained BAI enlargement, asymmetry, fluid buildup or a lump assessment the breast or armpit, but may be rarely assessmenf DKA prevention such dystem overlying skin rash, hardening of the sssessment.
Women who Joint health vitality these BIA lymphatic system assessment should see their physician to ssytem evaluated lymphaitc a physical exam and further testing. Receiving assdssment diagnosis of BIA-ALCL lymphaitc cause anxiety and frustration ssystem women should assessnent that not all cancers are equal.
When caught early, Wssessment is curable in most patients. ASPS Gut health and concentration BIA-ALCL guidelines syztem by lymphxtic National Comprehensive Center Network NCCNwhich defines diagnosis and treatment based on proven methods to treat the disease.
Disease re-occurrence is rare after surgical removal for early disease. The U. Food and Drug Administration FDA specifically recommends that all confirmed cases be reported to the PROFILE registry. If you have been diagnosed with BIA-ALCL, please ensure your physician has reported the case to the PROFILE registry for tracking of cases.
Information reported to PROFILE is updated with the FDA on a monthly basis. While PROFILE is a physician reporting system, if you would like to report your case directly, you may contact PSF who can get you in contact with a physician willing and able to report your case.
American Society of Plastic Surgeons. Community Home ask a surgeon patient community. Ask a Surgeon. Patient Community. Post your question to Ask a Surgeon to get an authoritative and trustworthy answer from our ASPS member surgeons or share your journey with other people just like you on the Patient Community.
The views expressed in Ask a Surgeon and the Patient Community are those of the participants and do not necessarily reflect the opinions of the American Society of Plastic Surgeons.
Share your journey with other people just like you on the Patient Community or post your question to Ask a Surgeon to get an authoritative and trustworthy answer from our ASPS member surgeons. Post your question to Ask a Surgeon to get an authoritative and trustworthy answer from our ASPS member surgeons.
or share your journey with other people just like you on the Patient Community. Share your journey with other people just like you on the Patient Community.
or post your question to Ask a Surgeon to get an authoritative and trustworthy answer from our ASPS member surgeons. Account Dashboard Log In. Log In. My Account. Log Out. Additional Resources Corporate Opportunities Contact ASPS EdNet PRS PRS GO WPS YPS GRAFT NBIR PROFILE.
Patient Safety Breast Implant Safety Breast Implant-Associated Anaplastic Large Cell Lymphoma BIA-ALCL Disease Summary. Allergan Biocell Device Withdrawal Information Common symptoms include breast enlargement, pain, asymmetry, lump in the breast or armpit, overlying skin rash, hardening of the breast, or a large fluid collection typically developing at least more than one year after receiving an implant, and on average after 8 to 10 years.
Considering reconstruction with implants? Have you developed symptoms? Schedule a follow-up appointment with your treating physician to discuss and concerns you may have about your breast health. Following a physical examination, patients with BIA-ALCL symptoms may receive an ultrasound or a magnetic resonance imaging MRI of the symptomatic breast to evaluate for fluid or lumps around the implant and in the lymph nodes.
If fluid or a mass is found, patients will require a needle biopsy with drainage of the fluid to test for BIA-ALCL. This fluid will be tested for CD30 immune staining CD30IHC performed by a pathologist.
Testing for CD30IHC is required to confirm a diagnosis or rule out BIA-ALCL. Fluid collections ruled out by CD30IHC for BIA-ALCL will be treated as typical seromas by a physician. Specimens not testing for CD30 may miss the diagnosis of BIA-ALCL. Have you been diagnosed with BIA-ALCL?
Any spread of the disease determines the stages, which is important for treatment. Newly diagnosed patients will be referred to an oncologist for evaluation of BIA-ALCL, staging of disease, and treatment planning.
For patients with BIA-ALCL only around the implant, surgery is performed to remove the breast implant and the scar capsule around the implant. Lumps in the armpit may be disease that has spread to the lymph nodes or may still be a normal enlargement of the lymph nodes.
Testing of the lymph nodes may be performed with a needle biopsy or with a surgery to remove a lymph node for testing.
Additional tests may sometimes include blood tests and a bone marrow biopsy. Reporting of confirmed cases The U. Additional Information.
Frequently Asked Questions Patient Advisory Allergan: Biocell Safety Alert FDA Updates on Implants and BIA-ALCL MD Anderson Cancer Center Patient Information on BIA-ALCL Australian Government Department of Health on BIA-ALCL The PROFILE Registry BIA-ALCL Physician Resources Beneficios y Riesgos de los Implantes de Seno.
More Resources. Patient Safety Resources ASPS Member Qualifications Breast Implant Safety Plastic Surgery Glossary. Video Gallery View Video Gallery. Patient Safety View Patient Safety.
: BIA lymphatic system assessment| Lymphatic imaging to assess rheumatoid flare: mechanistic insights and biomarker potential | In the tumor necrosis factor-transgenic TNF-Tg mouse, we found increased expression of VEGF-C and increased lymphatic vessel formation in the synovium of these mice early on during the disease process. After 8 weeks of treatment, we noted decreased lymphatic vessel formation and popliteal lymph node PLN size, and increased evidence of joint inflammation as determined by synovial volumes and synovial inflammatory areas at the ankle and knee joints. These findings led us to conclude that VEGF-C-induced lymphangiogenesis ameliorates joint tissue damage in arthritis by promoting drainage of inflamed joints. Furthermore, our in-vitro studies showed that TNF stimulates osteoclast precursors to express VEGF-C and promote lymphangiogenesis. However, persistent inflammation may inhibit lymphatic vessel development and draining function. Recently, we found that TNF stimulates lymphatic endothelial cells to produce iNOS, which inhibits lymphatic smooth muscle cell contraction and lymph drainage [ 17 ]. An early study by Polzer et al. They theorized that formation of more lymphatic vessels would improve clearance of pathogenic mediators, including proinflammatory cytokines and effector immune cells, such as macrophages. It should be noted that they used a different model of the TNF-Tg mouse, which develops severe inflammatory disease earlier than our model. The finding that both TNF and TNF inhibition can stimulate lymphangiogenesis, although counterintuitive, may therefore relate to the location, stage, and extent of inflammation. It is clear, however, that further research will be necessary to clarify the role of TNF in lymphangiogenesis and inflammation. Although Chauffard and Ramond first described LN involvement and lymphadenopathy in RA patients in [ 19 , 20 ], remarkably little is still known about the pathologic features and underling etiology. Harold Paulus and colleagues proposed that effector lymphocytes in lymphatic fluid were central to RA pathogenesis. In support of this view was the dramatic improvement of joint symptoms in RA patients who underwent drainage of the thoracic duct [ 21 ]. They described a cohort of nine women with untreated RA aged 24—65 years old who underwent insertion of a fistula into the thoracic duct and drainage of lymphatic fluid. Cells were removed from the fluid and reinfused; the depletion was performed daily for 19— days. Within 1 week, the investigators documented improvement in the number of tender and swollen joints, decreased morning stiffness, and improved grip strength. Unfortunately, symptoms returned after removal of the fistula and completion of the study. In subsequent experiments they infused autologous labeled lymphocytes, and arthritic flares were noted a mean of 3. These findings supported their hypothesis that lymphocytes in the lymphatic fluid are the primary mediators of RA [ 22 — 24 ]. Despite the new knowledge gained in these studies, further advances using this approach were stalled due to the lack of visual and quantitative assessments coupled with the challenges related to the feasibility of the procedure and transient responses. Indeed, the entire literature on lymphatic outcomes in arthritis is limited to three peer-reviewed publications from to [ 25 — 27 ]. Historically, performance of lymphoscintigraphy in arthritis patients was limited to those with lymphedema. In , Kallioma and Vastamak [ 28 ] reported on lymphoscintigraphy studies in Finland of the lymphatics in two women with RA who subsequently developed lymphedema of the right arm. They noted decreased uptake in the axillary nodes of the lymphedematous arthritic hand at both timepoints, and proposed an association between lymphatic dysfunction and inflammatory arthritis. Subsequently, radiocolloid lymphoscintigraphy became the imaging modality of choice over the lymphogram, an invasive procedure that requires cannulation and injection of lymphatic vessels with contrast in order to visualize them with X-ray imaging [ 29 ]. In the s, several studies used 99 technetium 99 Tc colloid lymphoscintigraphy to demonstrate lymphatic dysfunction in patients with RA or psoriatic arthritis who developed lymphedema in their arthritic extremities [ 30 — 33 ]. In the majority of these case reports, lymphedema lessened when arthritis improved after therapy; this was associated with normalization of colloid uptake assessed by lymphoscintigraphy. However, improvement was not associated with the duration of lymphedema, arthritis, or the type of disease-modifying anti-rheumatic drug DMARD. The co-occurrence of RA and lymphedema is a relatively rare event so opportunities to gain additional insights are limited; gaining more understanding of the role of lymphatics in RA requires an alternative strategy. In our initial human studies we turned to lymphoscintigraphy to analyze lymphatic transport in RA inflammation pre and post anti-TNF therapy as part of a clinical study ClinicalTrials. The duration of treatment was 18 weeks, and patients were scanned just prior to initiation of therapy and after 18 weeks. An example of these 99 Tc sulfur colloid tracing studies is shown in Fig. Colloid was injected in the usual fashion into the web spaces of the fingers or toes by a radiologist, and the limb was scanned at specific timepoints. Because lymphoscintigraphy cannot identify individual lymphatic vessels, it cannot detect lymphatic contractions. The technique therefore relies on the transit time tt of colloid from the injection site to LN regions, and compares the tt with known normal times. This study produced interesting findings, but we abandoned this approach due to the relatively invasive nature of the technique, radiation exposure, and the prolonged duration of the procedure; these considerations limit its use in the long-term, large-scale studies necessary to further understand the role of lymphatic flow during flare. Increased lymphatic flow from flaring joints normalizes with effective anti-TNF therapy. Images of 99 Tc sulfur colloid tracing of the lower extremity to the pelvis obtained from a RA patient with asymmetric knee flare enrolled in a clinical study to assess the effects of anti-TNF therapy on arthritis and lymphatics ClinicalTrials. Note the bright 99 Tc sulfur colloid signal in the inguinal arrows and popliteal arrowheads areas on both lower extremities pre treatment, and the decreased signal post treatment, which resulted in normalization of the tt from 15 minutes to 60 minutes. Schematic diagram between the lymposcintigrams orients the regions of interest. R right leg, L left leg. Although MRI methods to assess synovial inflammation in arthritis were well established [ 37 ], visualization of lymphatics was never documented. Subsequent CE-MRI studies in TNF-Tg line mice revealed that the draining LN undergoes dynamic transitions which are associated with activity of the arthritis in the proximal joint [ 38 — 40 ]. The LN volume expands, presumably to accommodate the influx of cells and lymph exiting the inflamed synovium. Furthermore, a subset of B cells, termed B-cells-in-inflamed-nodes B-in cells , accumulates in follicular areas of the draining LN [ 41 , 42 ]. Coincident with the collapse, B-in cells translocate to the paracortical sinuses of the LN, the proximal joint swells, and joint histopathology shows synovitis. Additionally, intravital immunofluorescent microscopy studies pre and post treatment with anti-CD20 antibodies that ameliorated arthritic inflammation in TNF-Tg mice demonstrated that translocated B-in cells effectively block passive lymph flow through the LN. Further support of the important function of the B-in cells was the restoration of lymphatic flow by B-cell depletion therapy [ 38 ]. Interestingly, while B-cell depletion allowed for restoration of passive flow and amelioration of synovial inflammation, it did not restore the lymphatic contractions or active lymphatic transport. Thus, B cells play a passive role in an arthritic flare that lessens in severity when passive lymphatic egress from inflamed joints occurs. This finding suggested two novel intervention strategies currently under investigation: treatment with agents that restore lymphatic contraction and active lymphatic flow; and nonimmunosuppressive treatments that open collateral lymphatic vessels to restore local lymphatic egress by circumventing the sites of B-cell obstruction. A third concept arising from these studies focused on the involvement of lymphatic smooth muscle cells in dysfunction of lymphatics in RA inflammation. To test whether RA pathogenesis also involves expanding and collapsed draining LNs, we completed a clinical pilot study in which patients with knee flare were imaged with CE-MRI pre and post certolizumab CZP therapy ClinicalTrials. The 3D rendering for volumetric analyses confirmed this finding Fig. Collectively, these data indicate that RA patients who sustain draining LN volume during anti-TNF therapy experienced the greatest pain relief in flaring joints, and provide the first clinical evidence to support the concept that dynamic changes in LN volume correlate with response to therapy in RA. Expanding versus collapsed popliteal LNs in early versus late-stage RA knee flare. Based on the aforementioned preclinical and clinical studies, there is reasonable evidence to support the use of MRI in evaluating draining LNs as a potential early marker of arthritic flare. While the murine models of arthritis have more fully defined that collapse of a draining LN is associated with arthritic flare, a similar correlation in humans has yet to be elucidated. We know, for example, that LNs undergo dramatic changes during synovial inflammation [ 45 ], and that these changes can differentiate between RA versus osteoarthritis. However, MRI alone cannot currently evaluate lymphatic vessels, which may be a potential limitation of this imaging modality. MRI is the gold standard for quantitative deep soft-tissue imaging due to its unparalleled sensitivity, specificity, and clinical validation [ 46 , 47 ]. However, the prohibitively high costs of MRI and limited access have contributed to a marked increase in ultrasound US imaging. US has several advantages including real-time imaging, accessibility, cost-efficiency, and absence of ionizing radiation [ 48 ]. Moreover, US is particularly useful for assessment of RA joint inflammation with gray-scale imaging, and power Doppler PD US assessment of synovial hyperemia; both modalities assist in the diagnosis of active synovitis and flares while providing semiquantitative analyses PD Score of synovial inflammation for clinical research [ 49 — 52 ]. MRI cost-efficiency issues also apply to preclinical research [ 53 — 56 ], so we adapted PD-US imaging to murine models of inflammatory-erosive arthritis to assess synovitis and alterations of draining LNs longitudinally. Recently, we validated our PD-US quantitative assessments of expanding vs collapsed PLN in TNF-Tg mice [ 57 , 58 ]. However, PD-US imaging of human LN, particularly PLN, remains elusive due to tissue depth concerns, and continues to be an area of active investigation. The availability of near-infrared NIR imaging of injected indocyanine green ICG fluorescent dye was a transformative advance in the quantitative assessment of in-vivo lymphatic function. Low-resolution NIR-ICG imaging has been used to identify sentinel LN during tumor resection surgery for a decade [ 59 , 60 ], but appropriate optics with computer analyses to quantify human lymphatic function was introduced only recently. In these pioneering studies, groups such as that of Sevick-Muraca and colleagues applied NIR-ICG imaging techniques to evaluate lymphatic vessels in patients with lymphedema [ 61 — 63 ]. More recently, they examined 24 patients with lymphedema and 20 healthy controls, and demonstrated more tortuous and friable lymphatic vessels with extravascular accumulation of lymph in lymphedema patients compared with controls [ 64 ]. Furthermore, they quantified the contraction rate of the intrinsic contractile activity of lymphatic vessels in healthy patients. However, they were unable to calculate the contraction rate in lymphedema patients due to the dysmorphic vessel architecture and the inability to visualize ICG-labeled lymph movement in bolus formation, which is how the lymphatic contractions are quantified. Moreover, NIR-ICG imaging actually showed some retrograde movement of lymph in the lymphedema patients. This finding is likely due to the loss of normal vessel contractile ability followed by extravasation of lymph into the surrounding tissue and chronic tissue edema in these patients. A major question we plan to address is whether disturbances in RA lymphatic function are analogous to those observed in lymphedema patients. The first publication describing NIR-ICG imaging in arthritis used infrared spectroscopy to study synovial fluid in patients with inflammatory arthritis versus osteoarthritis in order to differentiate the types of arthritis [ 65 ]. Preclinical studies using mouse models of arthritis reported that in-vivo arthritis detection in the early stages of disease activity is feasible with the use of NIR imaging and fluorescent-labeled molecules such as ICG and folate receptor-targeted dyes [ 66 — 68 ]. Moving towards clinical translation, Krohn et al. Patients were given intravenous ICG and were assessed with a specialized imaging system and camera. They examined wrist, metacarpophalangeal MCP , and proximal interphalangeal PIP joints and developed a 4-point scoring system to identify the degree of enhancement. The findings were correlated with MRI scoring of synovitis in the same joints. The results showed that NIR-ICG imaging correlates well with MRI findings at certain phases of ICG uptake, but it was inconsistent and not superior to current imaging modalities. However, the relative speed and simplicity of this minimally invasive procedure coupled with in-vivo real-time results demonstrated the potential of providing information to the clinician in a timely manner. In brief, a custom NIR imaging system is used to visualize lymphatic contractions after a negligible amount of ICG dye is injected into the web spaces of the hands. NIR excitation is monitored using a power meter. After the injections, the upper extremities are imaged continuously for 10 minutes to observe lymphatic flow. A region of interest ROI is then positioned over lymphatics to calculate the mean pixel value; peaks associated with lymphatic contractions are indicative of contractions per minute cpm. Figure 3 and Additional file 1 : Movie 1 and Additional file 2 : Movie 2 describe the technique and illustrate the sensitivity and specificity of the approach to quantify lymphatic contractions using this first-generation experimental approach. Clinical NIR imaging to quantify lymphatic flow in the upper extremity. A custom NIR imaging system FD; FluxData Inc. After injections, the upper extremities were imaged for 10 minutes to observe lymphatic flow. The ROI was positioned over lymphatics to calculate the mean pixel value for each NIR frame; peaks associated with lymphatic contractions were counted to calculate cpm. Representative images of the left hand b obtained from real-time video Additional file 1 : Movie 1 and right antecubital fossa c Additional file 2 : Movie 2 with the ROI and the respective cpm green. The rationale for using NIR-ICG to evaluate lymphatic contractions is reasonable because it provides real-time information for the clinician. Furthermore, dysfunctional contractions, or no contractions, could indicate that the arthritic episode is the result of a drainage issue rather than synovial disturbances. The treatment would thus be tailored appropriately i. with use of anti-TNF therapy , which has been associated with increased lymphatic angiogenesis [ 18 ] rather than DMARDs or steroids. Because of the extensive use of ICG in cardiovascular imaging over the decades, this dye has been studied extensively in humans and has been approved by the FDA for use as an imaging dye. There is therefore no major health limitation of the NIR-ICG technique. The only limitation is the duration of a study, which can take about 1—2 hours, the equivalent of current imaging techniques such as MRI. The potential importance of lymphatic function as a key variable in RA flare is supported by the presence of palpable LN and lymphedema in some patients, and by preclinical data demonstrating major alterations in draining LNs and vasculature prior to arthritis onset. The role of the lymphatics in RA can now be examined with the advent of in-vivo imaging modalities that quantify lymphatic flow and contraction frequency. These technical advances may empower investigators to promote understanding in three critical areas. The first area is the redefinition of patterns of lymphatic flow anatomically, because most of our knowledge is derived from cadaveric studies and circulatory system mapping. Interestingly, our early studies have demonstrated inconsistencies in lymphatics drainage compared with previously published data. The second area is discovery of the cellular, molecular, and structural mechanisms that regulate lymphatic function and that are closely integrated with local biomechanics, inflammation, and parasympathetic innervation. Finally, the ultimate goal of this research is to identify novel molecular targets that will give rise to new interventions for RA flare. To achieve this goal, advancing technologies to noninvasively evaluate superficial and deep lymphatics in humans is a critical first step. Gibofsky A. Epidemiology, pathophysiology, and diagnosis of rheumatoid arthritis: a synopsis. Am J Manag Care. PubMed Google Scholar. Firestein GS. The disease formerly known as rheumatoid arthritis. Arthritis Res Ther. Article PubMed PubMed Central Google Scholar. Carubbi F, Zugaro L, Cipriani P, Conchiglia A, Gregori L, Danniballe C, Pistoia ML, Liakouli V, Ruscitti P, Ciccia F, et al. Safety and efficacy of intra-articular anti-tumor necrosis factor alpha agents compared to corticosteroids in a treat-to-target strategy in patients with inflammatory arthritis and monoarthritis flare. Int J Immunopathol Pharmacol. Article PubMed Google Scholar. Klasen IS, Ladestein RMT, Vandenberg WB, Benner R. Arthritis Rheum. Article CAS PubMed Google Scholar. Lens JW, Vandenberg WB, Vandeputte LBA, Zwarts WA. Flare of antigen-induced arthritis in mice after intravenous challenge—kinetics of antigen in the circulation and localization of antigen in the arthritic and noninflamed joint. Bingham CO, Pohl C, Woodworth TG, Hewlett SE, May JE, Rahman MU, Witter JP, Furst DE, Strand CV, Boers M, et al. Developing a standardized definition for disease "flare" in rheumatoid arthritis OMERACT 9 Special Interest Group. J Rheumatol. Benaglio F, Vitolo B, Scarabelli M, Binda E, Bugatti S, Caporali R, Montecucco C, Manzo A. The draining lymph node in rheumatoid arthritis: current concepts and research perspectives. Biomed Res Int. Bouta EM, Li J, Ju Y, Brown EB, Ritchlin CT, Xing L, Schwarz EM. The role of the lymphatic system in inflammatory-erosive arthritis. Semin Cell Dev Biol. Article CAS PubMed PubMed Central Google Scholar. Semo J, Nicenboim J, Yaniv K. Development of the lymphatic system: new questions and paradigms. Karpanen T, Alitalo K. Molecular biology and pathology of lymphangiogenesis. Annu Rev Pathol Mech. Article CAS Google Scholar. Ionac M, Laskay T, Labahn D, Geisslinger G, Solbach W. Improved technique for cannulation of the murine thoracic duct: a valuable tool for the dissection of immune responses. J Immunol Methods. Kaipainen A, Korhonen J, Mustonen T, Vanhinsbergh VWM, Fang GH, Dumont D, Breitman M, Alitalo K. Expression of the Fms-like tyrosine kinase-4 gene becomes restricted to lymphatic endothelium during development. Proc Natl Acad Sci U S A. Joukov V, Pajusola K, Kaipainen A, Chilov D, Lahtinen I, Kukk E, Saksela O, Kalkkinen N, Alitalo K. A novel vascular endothelial growth factor, VEGF-C, is a ligand for the Flt4 VEGFR-3 and KDR VEGFR-2 receptor tyrosine kinases vol 15, pg , Embo J. CAS PubMed PubMed Central Google Scholar. Zhou Q, Guo RL, Wood R, Boyce BF, Liang QQ, Wang YJ, Schwarz EM, Xing LP. Vascular endothelial growth factor C attenuates joint damage in chronic inflammatory arthritis by accelerating local lymphatic drainage in mice. Zhang Q, Lu Y, Proulx ST, Guo RL, Yao ZQ, Schwarz EM, Boyce BF, Xing LP. Most importantly, you and your surgeon should discuss your goals and expectations about having breast implants, the benefits and risks, the need to monitor your implant for complications for as long as you have them, and eventual removal or replacement. What actions will the FDA continue to take? The FDA continues to collect and evaluate information about BIA-ALCL in individuals with breast implants and who have used tissue expanders. What actions have been taken by Professional Societies and Regulatory bodies outside the US? The World Health Organization recognized breast implant-associated anaplastic large cell lymphoma BIA-ALCL as a unique form of ALCL that can develop following breast implant, implantation. Professional organizations, including the Plastic Surgery Foundation and the National Comprehensive Cancer Network NCCN published information to help physicians understand the disease and provide diagnosis and treatment. On February 12, Health Canada announced it will be updating its safety review of breast implants. On April 4, , the Medicines and Healthcare products Regulatory Agency announced its recommendations for patients and health care providers. On April 4, , the French National Agency for Medicines and Health Products Safety ANSM announced its decision to, as a precautionary measure, withdraw from "macrotextured" breast implants and breast implants with polyurethane-coated surfaces marketed in France. The ANSM does not recommend preventative explanation for women with these implants. On July 11, The Australian Therapeutic Goods Administration TGA reported announced it has completed assessment of textured breast implants available in Australia or exported from Australia and proposed regulatory actions. Where can we find more information? Additional information can be found in FDA's recent communications and our breast implant webpage. Skip to main content Skip to FDA Search Skip to in this section menu Skip to footer links. Types of Breast Implants Risks and Complications of Breast Implants Labeling for Approved Breast Implants Breast Implant Surgery Medical Device Reports for Systemic Symptoms in Women with Breast Implants Medical Device Reports of Breast Implant-Associated Anaplastic Large Cell Lymphoma Questions and Answers about Breast Implant-Associated Anaplastic Large Cell Lymphoma BIA-ALCL Things to Consider Before Getting Breast Implants Breast Implants: Additional Resources Breast Implant Postmarket Safety Information. As a result, we have determined that: All patients who have breast implants or are thinking about getting them should be aware of the risk of BIA-ALCL. The risk of BIA-ALCL is higher for textured surface implants versus smooth surface implants. Certain other textured breast products, specifically certain textured tissue expanders, should not be used, and we have issued new recommendations for patients who have or have had these products. Health Care Professionals: You should immediately stop using implanting the breast implants and tissue expanders listed in the July 24, FDA Safety Communication ; and work with your facility to return existing inventory. We are not recommending the routine removal of these or other types of breast implants in patients who have no symptoms. You should inform your patients who have the implants and tissue expanders listed in the July 24, FDA Safety Communication about the risks of serious adverse health consequences, including the potential for the development of BIA-ALCL. Prior to implantation of any breast implant, provide your patients with the manufacturer's patient labeling, as well as any other educational material, and discuss the benefits and risks of the different types of implants. Consider the possibility of BIA-ALCL when treating a patient with late onset, peri-implant changes. In some cases, patients presented with a seroma, mass, hardening adjacent to the breast implant. If you have a patient with suspected BIA-ALCL, refer the patient's case to experts familiar with the diagnosis and treatment of BIA-ALCL. Collect fresh seroma fluid and representative portions of the capsule and send for pathology tests to rule out BIA-ALCL. Develop an individualized treatment plan in coordination with experts familiar with the diagnosis and treatment of BIA-ALCL. Consider current clinical practice guidelines, such as those from the Plastic Surgery Foundation or the National Comprehensive Cancer Network NCCN when choosing your treatment approach. Patients: If you have no symptoms, we are not recommending the removal of the implants and tissue expanders listed in the July 24, FDA Safety Communication ; or other types of breast implants due to concern related to the risk of developing BIA-ALCL. Know the symptoms of BIA-ALCL, primarily persistent swelling, presence of a mass or pain in the vicinity of the breast implant and monitor the area around your breast implants for any changes. If you experience any of these symptoms or other changes, talk to your healthcare provider regarding the need for further evaluation. It is important to undergo an evaluation to diagnose BIA-ALCL since a confirmed BIA-ALCL diagnosis may change the type of operation that should be performed. Patients with confirmed BIA-ALCL should undergo implant removal with removal of the surrounding scar capsule, which is a more extensive operation than implant removal alone. Isaac Stein. Orpheus Kolokythas. For appointment information please contact A knowledgeable team member will assist you. Lymphedema Network of Excellence. Home » Lymphedema Network of Excellence. VA Health Care. Surgery Centers. LYMPHATIC SYSTEM We produce approximately 3 liters of lymph per day in our bodies. Referral Criteria Collapse. BMI less than Exceptions will be considered on a case by case basis if a letter addressing BMI is included by referring provider. Please also have images pushed to UW PACs. More information on nuclear medicine lymphoscintigraphy testing: Nuclear Medicine Lymphoscintigraphy This test involves the injection of a filtered sulphur colloid called Technetium, into the limb arm or leg. Insurance Coverage of Services Expand. What is Lymphedema? Assessment of the Lymphedema Patient Expand. Treatment Of Lymphedema Expand. SURGICAL THERAPY The type of surgical treatment depends on pre-operative assessment. LYMPH NODE TRANSFERS This procedure is also known as vascularized lymph node transfer VLNT and involves transplanting lymph nodes from an uninvolved area in the body into the lymphedematous area. Surgical Providers Expand. Further Information Reading Resources Expand. Bibliography Papers Published in Peer Reviewed Journals: Successful treatment of lymphedema in a vasculopath and neuropathic patient. Inchauste S , Zelones J, Rochlin D, Nguyen DH. J Surg Oncol. Lymphedema: Complete Medical and Surgical Treatment The role of adjunct nanofibrillar collagen scaffold implantation in the surgical management of secondary lymphedema: Review of the literature and summary of initial pilot studies. Rochlin DH, Inchauste S , Zelones J, Nguyen DH. Lymph node transplantation for the treatment of lymphedema. Gould DJ, Mehrara BJ, Neligan P , Cheng MH, Patel KM. Initial Clinical Experience with Dual-Agent Relaxation Contrast for Isolated Lymphatic Channel Mapping. Ripley B, Wilson GJ, Lalwani N, Briller N, Neligan PC , Maki JH. Current Concepts in the Surgical Management of Lymphedema. Kung TA, Champaneria MC, Maki JH, Neligan PC. Plast Reconstr Surg. Peripheral Magnetic Resonance Lymphangiography: Techniques and Applications. Mitsumori LM, McDonald ES, Neligan PC , Maki JH. Tech Vasc Interv Radiol. Lymphedema: Surgical and Medical Therapy. Chang DW, Masia J, Garza R 3rd, Skoracki R, Neligan PC. MR lymphangiography in the treatment of lymphedema. Neligan PC , Kung TA, Maki JH. Dark Blood Magnetic Resonance Lymphangiography Using Dual-Agent Relaxivity Contrast DARC-MRL : A Novel Method Combining Gadolinium and Iron Contrast Agents. Maki JH, Neligan PC , Briller N, Mitsumori LM, Wilson GJ. Curr Probl Diagn Radiol. MR lymphangiography: How i do it. |
| Background | Beck, C. Beyond early development: Xenopus as an emerging model for the study of regenerative mechanisms. Dent, J. Limb regeneration in larvae and metamorphosing individuals of the South African clawed toad. Endo, T. Shh expression in developing and regenerating limb buds of Xenopus laevis. Dyn , — Nye, H. Strategies to reduce variation in Xenopus regeneration studies. Yokoyama, H. FGF stimulates limb regeneration ability in Xenopus laevis. Godwin, J. Scar-free wound healing and regeneration in amphibians: Immunological influences on regenerative success. Differentiation 87 , 66—75 Mescher, A. Limb regeneration in amphibians: Immunological considerations. World J. Article Google Scholar. McCusker, C. Scavelli, C. Lymphatics at the crossroads of angiogenesis and lymphangiogenesis. Crossley, D. Posterior lymph heart function in two species of anurans: Analysis based on both in vivo pressure—volume relationships by conductance manometry and ultrasound. Jones, J. Posterior lymph heart pressure and rate and lymph flow in the toad Bufo marinus in response to hydrated and dehydrated conditions. Ito, R. Overview of lymph node transfer for lymphedema treatment. Yamamoto, T. Indocyanine green lymphography findings in primary leg lymphedema. Narushima, M. Indocyanine green lymphography findings in limb lymphedema. Direct measurement of flow from the posterior lymph hearts of hydrated and dehydrated toads Bufo marinus. Oliver, G. the lymphatic vasculature in the 21st century: Novel functional roles in homeostasis and disease. Cell , — Edwards, J. Lymphatics and bone. Debuque, R. Identification of the adult hematopoietic liver as the primary reservoir for the recruitment of pro-regenerative macrophages required for salamander limb regeneration. Cell Dev. Takaya, K. Gorham-Stout disease with parietal bone osteolysis: A case series and review of literature. Hightower, J. Hemopoietic tissue in the adult newt Notopthalmus viridescens. Lopez, D. Mapping hematopoiesis in a fully regenerative vertebrate: The axolotl. Blood , — Rodgers, A. Identification of immune and non-immune cells in regenerating axolotl limbs by single-cell sequencing. Cell Res. Leigh, N. Transcriptomic landscape of the blastema niche in regenerating adult axolotl limbs at single-cell resolution. Article ADS CAS Google Scholar. Bolaños-Castro, L. Immunity in salamander regeneration: Where are we standing and where are we headed?. Fini, M. Limb regeneration of the adult newt Notophthalmus viridescens in the absence of the spleen. Clavin, N. TGF-β1 is a negative regulator of lymphatic regeneration during wound repair. Heart Circ. Azhar, S. The unresolved pathophysiology of lymphedema. Rusznyák, I. Lymphatics and Lymph Circulation: Physiology and Pathology Pergamon Press, Rumyantsev, P. Ultrastructure of myofibers and cells synthesizing DNA in the developing and regenerating lymph-heart muscles. Jha, S. Efficient activation of the lymphangiogenic growth factor VEGF-C requires the C-terminal domain of VEGF-C and the N-terminal domain of CCBE1. Article CAS Google Scholar. The cardiopharyngeal mesoderm contributes to lymphatic vessel development in mouse. Isl1-expressing non-venous cell lineage contributes to cardiac lymphatic vessel development. Ishiura, R. Successful treatment of large abdominal lymphatic malformations and chylous ascites with intra-abdominal lymphovenous anastomosis. Venous Lymphat. Mihara, M. High-accuracy diagnosis and regional classification of lymphedema using indocyanine green fluorescent lymphography after gynecologic cancer treatment. Mitsui, K. Dual imaging lymphangiography guided treatment of infantile chylothorax. Cases Innov. Akita, S. Improvement of the efficacy of vascularized lymph node transfer for lower-extremity lymphedema via a prefabricated lympho-venous shunt through lymphaticovenular anastomosis between the efferent lymphatic vessel and small vein in the elevated vascularized lymph node. Microsurgery 38 , — Yu, Z. The latent dedifferentiation capacity of newt limb muscles is unleashed by a combination of metamorphosis and body growth. CAS Google Scholar. du Sert, N. The ARRIVE guidelines 2. PLoS Biol. Tanaka, H. A developmentally regulated switch from stem cells to dedifferentiation for limb muscle regeneration in newts. Casco-Robles, R. Novel erythrocyte clumps revealed by an orphan gene Newtic1 in circulating blood and regenerating limbs of the adult newt. Article ADS PubMed PubMed Central Google Scholar. Schneider, C. NIH image to ImageJ: 25 years of image analysis. Methods 9 , — Rueden, C. Image J2: ImageJ for the next generation of scientific image data. BMC Bioinform. Iten, L. Forelimb regeneration from different levels of amputation in the newt, Notophthalmus viridescens : Length, rate, and stages. Wilhelm Roux Arch. Download references. This work was funded by Japan Society for the Promotion of Science KAKENHI grants Grants Numbers: 21K and 18H We would like to sincerely thank Mrs. Kiku Shinano for the general administrative support offered and Dr Jackson Chipaila, Prof Taizo Shiraishi, Dr Takahara Iino and Mrs Miyuki Namikata for assisting with the experiments. This work was funded by the Japan Society for the Promotion of Science KAKENHI grants Grant Numbers: 21K and 18H Department of Plastic and Reconstructive Surgery, Graduate School of Medicine, Mie University, Edobashi, Tsu, Mie Prefecture, , Japan. Chihena H. Faculty of Life and Environmental Sciences, University of Tsukuba, Tennodai, Tsukuba, Ibaraki Prefecture, , Japan. Department of Personalized Cancer Immunotherapy, Graduate School of Medicine, Mie University, Edobashi, Tsu, Mie Prefecture, , Japan. Department of Pathology and Matrix Biology, Graduate School of Medicine, Mie University, Edobashi, Tsu, Mie Prefecture, , Japan. You can also search for this author in PubMed Google Scholar. and Ko. designed the study. and C. performed the acquisition of data. M and C. participated in the analysis and interpretation of the data. drafted the manuscript and M. revised the manuscript. All the listed authors approved the final version of the manuscript and have agreed to be personally accountable for the content of this study. Correspondence to Mitsunaga Narushima. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Open Access This article is licensed under a Creative Commons Attribution 4. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. Reprints and permissions. Banda, C. Structural and functional analysis of the newt lymphatic system. Sci Rep 13 , Download citation. Received : 19 December Accepted : 25 April Published : 27 April Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate. Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily. Skip to main content Thank you for visiting nature. nature scientific reports articles article. Download PDF. Subjects Animal physiology Imaging Imaging the immune system Lymphangiogenesis Lymphatic system Regeneration. Abstract Regeneration competent vertebrates such as newts and salamanders possess a weakened adaptive immune system characterized by multiple connections between the lymphatic system and the blood vascular system called lymphatic hearts. Introduction The lymphatics system consists of a network of lymphatic vessels, lymphoid tissue and lymphoid organs that form an important part of the immune system in vertebrates. Results Newt lymphatic circulation is organized into defined lymphatic territories We first evaluated the lymphatic drainage territories in-vivo using indocyanine green ICG near-infrared fluoroscopy NIRF lymphangiography complimented with ultra-high frequency ultrasonography UHFUS and micro-computer tomography micro-CT contrast lymphangiography. Figure 1. Full size image. Figure 2. Figure 3. Figure 4. Figure 5. Figure 6. Figure 7. Figure 8. Discussion Lymphatic reconstructive microsurgery of lymphedema has established that much like the angiosomes of blood vessels, lymphatic vasculature despite its extensive inter-connections, is also organized into functional units with specific lymphatic collectors preferentially draining a specific 3-dimensional block of tissue territory also known as a lymphosome 28 , 29 , Method Animals Wild-type and transgenic albino adult Japanese fire belly newts Cynops pyrrhogaster 90 to mm snout-to-tail length were obtained from Tsukuba University Faculty of Life and Environmental Sciences Anesthesia Animals received anesthesia with 0. Immunohistochemistry and fluorescent dye studies Immunohistochemistry was performed as previously described by Casco-Robles et al. Antibodies The following antibodies were purchased, Anti-LYVE-1 Novus NB , Anti-CD Bioss BSR , Anti-LYVE-1 Abcam Ab Lymphatic heart microsurgical excision procedure Following anesthesia, 50 μL ICG dye was injected subcutaneously into the limbs or tail of the newts and frogs. Randomized control trial of limb regeneration after lymphatic heart excision A total of 62 newts were enrolled into the randomized control trial and divided into 4 blocks designed to evaluate regeneration after incremental LH excision and regeneration after the onset of circulatory changes at 1 week PO. Micro-CT lymphangiography Micro-CT lymphangiography was performed using CosmoScan GXII Rigaku, Tokyo, Japan before and 10—60 min after subcutaneous injection of 10—50 μL Iohexol Omnipaque®, GE Healthcare Pharma, Tokyo, Japan and the images processed using RadiAnt DICOM Viewer software. Tissue fixation by trans-lymphatic perfusion FixLyP FixLyP was performed to clear the red blood cells from blood vessels and fix the lymphatic vessels to prevent their collapse in preparation for computer 3D volume reconstruction of serial slides. Electron microscopy Samples were prefixed in 2. Data analysis software Analyses were performed using SPSS 26 IBM Corp. Conference presentation Presented at the 31st Annual University of Tokyo Plastic Surgery Scientific Conference, January , Tokyo, Japan. Data availability The data that support the findings of this study are available from the corresponding author upon reasonable request. Abbreviations BEC: Blood vessel endothelial cells ICG: Indocyanine green NIRF: Near-infrared fluoroscopy lymphangiography LEC: Lymphatic endothelial cell LH: Lymphatic heart UHFUS: Ultra-high frequency ultrasonography TLyLL: Trunci lymphatici longitudinales lateralis TLyLPab: Trunci lymphatici longitudinales parabdominales TlyLPe: Trunci lymphatici longitudinales parepigastrici TLyLSv: Trunci lymphatici longitudinales subvertebrales TvIL: Transverse vertebral intraosseous lymphatic vessels TvIV: Transverse vertebral intraosseous veins VCP: Vena cava posterior VL: Venous lateralis. References Hansen, K. Article CAS PubMed Google Scholar Dzieciatkowska, M. Article CAS PubMed PubMed Central Google Scholar Ulvmar, M. Article CAS PubMed PubMed Central Google Scholar Randolph, G. Article CAS PubMed Google Scholar Maruyama, K. Article CAS PubMed PubMed Central Google Scholar Maruyama, K. Article ADS CAS PubMed PubMed Central Google Scholar Rockson, S. Article ADS PubMed Google Scholar Hedrick, M. Article PubMed Google Scholar Francis, E. Google Scholar Kampmeier, O. Google Scholar Duellman, W. Book Google Scholar Kampmeier, O. Article CAS PubMed Google Scholar Peyrot, S. Article CAS PubMed PubMed Central Google Scholar Kampmeier, O. Article CAS PubMed Google Scholar Mccusker, C. Article PubMed PubMed Central Google Scholar Dunlap, G. Article CAS PubMed Google Scholar Beck, C. Article CAS PubMed Google Scholar Dent, J. Article CAS PubMed Google Scholar Endo, T. Article CAS PubMed Google Scholar Nye, H. Article CAS PubMed Google Scholar Yokoyama, H. Article CAS PubMed Google Scholar Godwin, J. Article CAS PubMed Google Scholar Mescher, A. Article Google Scholar McCusker, C. Article PubMed PubMed Central Google Scholar Scavelli, C. Lymph is a fluid that comes from the circulatory system and its function is to clear the soft tissues of any impurities, such as bacteria, cancer cells and many other cell types. Lymph is collected in lymphatic channels, which are small vessels, akin to but smaller than arteries and veins. The lymph is then transported to the regional lymph nodes. Lymph nodes are part of our immune system and are essentially filters. These filters trap whatever the lymphatic fluid brings to them and the body's immune system deals with these products. This is why, for example, lymph nodes are targeted in cancer treatment: cancer cells can be transported to lymph nodes and these nodes are sometimes removed or radiated to kill the cancer cells. Referrals packets will be reviewed by our intake specialists and patients meeting criteria will be offered an initial evaluation appointment. The following criteria must be met:. More information on nuclear medicine lymphoscintigraphy testing:. Nuclear Medicine Lymphoscintigraphy. This test involves the injection of a filtered sulphur colloid called Technetium, into the limb arm or leg. The patient is then scanned so that we can see how that marker is transported through the lymphatic system. It picks up abnormalities in the lymphatic system. The picture shows a patient post breast cancer with axillary node dissection and radiation. The technetium has been injected into her arms and feet. On the upper left of the picture the axillary nodes can be seen as black dots. There are no such dots on the right side indicating that there is blockage of lymphatic drainage on that side. Many insurances do not cover surgical lymphedema treatments. Patients may be asked to sign a Notice of Non Coverage NNC which acknowledges financial responsibility prior to their visit. This may apply even to the initial evaluation. Package pricing for initial evaluation and also for surgery is available. Lymphedema is a condition in which the lymphatic system is compromised. This can happen for many different reasons. The most common cause world-wide is a condition called Filariasis, an infestation by a type of worm, a nematode, that is endemic in certain parts of the world. In the United States, the two most common causes are congenital, meaning someone is born with the condition, or acquired, when the condition arises from anything that impacts the lymphatic system. There are several different presentations of congenital lymphedema: Milroy Disease or TYPE 1 , Lymphedema , and Type 2 lymphedema , which can present in the teen years as Lymphedema Praecox , and Lymphedema Tarda , which presents in the 30's or later. The most common type of acquired lymphedema is related to surgery in cancer patients, often when combined with radiation. The most common types of cancer patients we see are breast cancer, pelvic cancers, head and neck cancers, and melanoma. There is also an association between morbid obesity and lymphedema, particularly as it applies to the lower extremities. The first priority for these patients is to lose weight, either through diet and exercise or bariatric surgery. Milroy Disease This is due to a protein receptor mutation. Pictured is a seven-year-old boy with lymphedema of his right leg, present since birth. At the UW Lymphedema Center, each patient is thoroughly assessed by taking a detailed medical history, standardized limb circumference measurements, and bio-impedance spectroscopy. Further testing following the initial evaluation may include magnetic resonance lymphangiography and fluorescent lymphangiography to help determine which surgical intervention may be most beneficial. MR Lymphangiography This test involves the injection of a contrast agent into the affected limb. A second agent is injected intravenously which allows us to image the venous system and then to differentiate between veins and lymphatics. In the picture, the lymphatic system is marked with arrows and the veins are marked. On the image on the right, the venous image has been darkened showing just the lymphatics. The MR gives us excellent information on the limb, and not just the lymphatics. Fluorescence lymphangiography This technique involves the injection of a fluorescent dye, Indocyanine Green ICG into the limb. A near-infra-red camera is the used to image the lymphatics. This technique allows us to see the superficial lymphatics, which are the ones we target at surgery. Four patterns of ICG have been described; Linear normal Splash, Stardust and Diffuse, which represent increasing severity of lymphedema. Bio-Impedance Spectroscopy: This test measures the time taken for the passage of a low electrical current through the tissues. The rationale is that the more fluid is in the tissues, the less resistance or impedance there will be to that electrical current. Professional organizations, including the Plastic Surgery Foundation and the National Comprehensive Cancer Network NCCN published information to help physicians understand the disease and provide diagnosis and treatment. On February 12, Health Canada announced it will be updating its safety review of breast implants. On April 4, , the Medicines and Healthcare products Regulatory Agency announced its recommendations for patients and health care providers. On April 4, , the French National Agency for Medicines and Health Products Safety ANSM announced its decision to, as a precautionary measure, withdraw from "macrotextured" breast implants and breast implants with polyurethane-coated surfaces marketed in France. The ANSM does not recommend preventative explanation for women with these implants. On July 11, The Australian Therapeutic Goods Administration TGA reported announced it has completed assessment of textured breast implants available in Australia or exported from Australia and proposed regulatory actions. Where can we find more information? Additional information can be found in FDA's recent communications and our breast implant webpage. Skip to main content Skip to FDA Search Skip to in this section menu Skip to footer links. Types of Breast Implants Risks and Complications of Breast Implants Labeling for Approved Breast Implants Breast Implant Surgery Medical Device Reports for Systemic Symptoms in Women with Breast Implants Medical Device Reports of Breast Implant-Associated Anaplastic Large Cell Lymphoma Questions and Answers about Breast Implant-Associated Anaplastic Large Cell Lymphoma BIA-ALCL Things to Consider Before Getting Breast Implants Breast Implants: Additional Resources Breast Implant Postmarket Safety Information. As a result, we have determined that: All patients who have breast implants or are thinking about getting them should be aware of the risk of BIA-ALCL. The risk of BIA-ALCL is higher for textured surface implants versus smooth surface implants. Certain other textured breast products, specifically certain textured tissue expanders, should not be used, and we have issued new recommendations for patients who have or have had these products. Health Care Professionals: You should immediately stop using implanting the breast implants and tissue expanders listed in the July 24, FDA Safety Communication ; and work with your facility to return existing inventory. We are not recommending the routine removal of these or other types of breast implants in patients who have no symptoms. You should inform your patients who have the implants and tissue expanders listed in the July 24, FDA Safety Communication about the risks of serious adverse health consequences, including the potential for the development of BIA-ALCL. Prior to implantation of any breast implant, provide your patients with the manufacturer's patient labeling, as well as any other educational material, and discuss the benefits and risks of the different types of implants. Consider the possibility of BIA-ALCL when treating a patient with late onset, peri-implant changes. In some cases, patients presented with a seroma, mass, hardening adjacent to the breast implant. If you have a patient with suspected BIA-ALCL, refer the patient's case to experts familiar with the diagnosis and treatment of BIA-ALCL. Collect fresh seroma fluid and representative portions of the capsule and send for pathology tests to rule out BIA-ALCL. Develop an individualized treatment plan in coordination with experts familiar with the diagnosis and treatment of BIA-ALCL. Consider current clinical practice guidelines, such as those from the Plastic Surgery Foundation or the National Comprehensive Cancer Network NCCN when choosing your treatment approach. Patients: If you have no symptoms, we are not recommending the removal of the implants and tissue expanders listed in the July 24, FDA Safety Communication ; or other types of breast implants due to concern related to the risk of developing BIA-ALCL. Know the symptoms of BIA-ALCL, primarily persistent swelling, presence of a mass or pain in the vicinity of the breast implant and monitor the area around your breast implants for any changes. If you experience any of these symptoms or other changes, talk to your healthcare provider regarding the need for further evaluation. It is important to undergo an evaluation to diagnose BIA-ALCL since a confirmed BIA-ALCL diagnosis may change the type of operation that should be performed. Patients with confirmed BIA-ALCL should undergo implant removal with removal of the surrounding scar capsule, which is a more extensive operation than implant removal alone. As with any implanted device, it is good to keep a record of the device manufacturer and implant model name. You may have received this information on a patient device card from your surgeon. If you would like to obtain the manufacturer name and model of your implants, consider asking your surgeon or obtaining the record of your surgery operative notes from the facility where it was performed. Understand that most cases of BIA-ALCL occur years after breast implant placement and present with symptoms or changes around the breast implant. Talk to your surgeon about your risk of developing BIA-ALCL. |
| Considering reconstruction with implants? | Lymphatic vessels were identified and differentiated from blood vessels by comparing differential rhodamine-dextran uptake and differential staining of VEGFR-3, LYVE-1 and CD Additional identification of lymphatic vessels by staining with commercially available Prox-1 antibodies in mature adult newts was attempted under varying experimental conditions however this was unsuccessful data not shown. Histology images were captured using a Keyence BZ-X Microscope and An Olympus AX80 coupled with an Olympus DP74 Microscope Digital Camera. Image processing was performed using Image J 58 , The following antibodies were purchased, Anti-LYVE-1 Novus NB , Anti-CD Bioss BSR , Anti-LYVE-1 Abcam Ab Anti-VEGFR-3 antibody was custom made based on the newt nucleotide orthologue by Eurofins Japan. Further details on the antibodies used are provided in the supplementary data. Following anesthesia, 50 μL ICG dye was injected subcutaneously into the limbs or tail of the newts and frogs. A longitudinal skin incision was made on the back immediately inferior to the lateral line ridge overlying the LHs to be removed using a No. The LHs were identified visually by pulsations and collection of ICG dye. LH were excised using supermicrosurgical technique and supermicrosurgery titanium instruments EMI Factory CO. Nagano, Japan to carefully preserve surrounding tissue in the study group while in the controls identical surgery was performed but the LHs were left intact. A total of 62 newts were enrolled into the randomized control trial and divided into 4 blocks designed to evaluate regeneration after incremental LH excision and regeneration after the onset of circulatory changes at 1 week PO. Newts were then randomized into approximately equal experimental groups using SPSS 26 by a blinded and independent assistant from HPB Surgery Department. Independent T tests were used to compare the mean snout-to-tail length and weight of the two groups. The 7 LHs draining the lower limb were identified in all newts and excised using supermicrosurgical technique as described above in the study group while in the controls identical dissection was performed but the LHs were left intact. The left hindlimb was amputated 2 mm proximal to the knee joint using a No. Gentle pressure was applied for a few min to achieve hemostasis. Blinding of the investigators was not possible due to the surgical nature of the experimental treatment. However, to limit bias, the assigned group was revealed to the microsurgeons only after wound exposure and lymphatic microdissection. The newts were kept unfed in separate plastic containers at room temperature, observed daily and the morphological stage of regeneration recorded Our original protocol planned for the assessment of the limb regeneration time by 3 blinded investigators. However, we departed from the protocol due to limited staff availability between and and instead, a single unblinded investigator performed this assessment. The rate of regeneration was compared between study and control groups using the Two-Sample Kolmogorov—Smirnov test. The Kruskal—Wallis test was used for subgroup analysis of the study group LH excision newts. Assessment of regenerated limb morphology was performed by 2 blinded investigators. Fisher Exact Test was used to compare the proportions of morphological anomalous regenerated limbs and PO deaths. Independent T tests were used to compare the vessel densities between groups. Micro-CT lymphangiography was performed using CosmoScan GXII Rigaku, Tokyo, Japan before and 10—60 min after subcutaneous injection of 10—50 μL Iohexol Omnipaque®, GE Healthcare Pharma, Tokyo, Japan and the images processed using RadiAnt DICOM Viewer software. Quantitative analysis of the VCP was performed using Image J Regeneration was assessed by opening the skin flap at weekly, then monthly intervals for days. FixLyP was performed to clear the red blood cells from blood vessels and fix the lymphatic vessels to prevent their collapse in preparation for computer 3D volume reconstruction of serial slides. A midline abdominal skin incision was made taking care not to penetrate the peritoneum. The VCP diameter 0. The peritoneum was opened, small size microvascular clamps applied proximally and distally, and the vein cut 5 mm before it enters the liver. The cephalic end of the vein was prepared using standard microsurgical technique to dissect off the adventitia. A microvascular round-tipped blunt vascular needle was then inserted into the cephalic end of the vein and the vascular clamps released. Cold heparin saline 4 °C was slowly injected into the vein using a 1 ml syringe allowing the caudal end of the vein to bleed freely until the liver color became whitish and clear heparin saline was seen draining. K, Hamamatsu, JAPAN. Digital 3-D computer volume reconstruction of serial slides of the abdomen and tail was performed using Image J FiJi Version 1. In cases where a tissue section was heavily distorted or damaged by preparation artifacts, the image was excluded from the stack and the best fit adjacent image was duplicated to maintain the tissue volume. Lymphatic vessels were tracked and marked in a retrograde fashion while blood vessels were marked in antegrade from the LHs Supplementary Fig. Samples were prefixed in 2. PBS wash was repeated twice for 15 min, and the sample dehydrated in increasing concentrations of ethanol then transferred to acetone. The samples were infiltrated then embedded in epoxy resin. Serial μm scanning sections stained with toluidine blue were prepared for light microscopy and 80 nm sections cut for transmission electron microscopy then viewed using a JEMFlash Electron Microscope JEOL, Tokyo, Japan. Analyses were performed using SPSS 26 IBM Corp. Released Armonk, NY and SPSS 27 IBM Corp. Armonk, NY. Presented at the 31st Annual University of Tokyo Plastic Surgery Scientific Conference, January , Tokyo, Japan. The data that support the findings of this study are available from the corresponding author upon reasonable request. Hansen, K. Lymph formation, composition and circulation: A proteomics perspective. Article CAS PubMed Google Scholar. Dzieciatkowska, M. et al. Lymph is not a plasma ultrafiltrate: A proteomic analysis of injured patients. Shock 42 , — Article CAS PubMed PubMed Central Google Scholar. Ulvmar, M. Heterogeneity in the lymphatic vascular system and its origin. Randolph, G. The lymphatic system: Integral roles in immunity. Maruyama, K. The pathogenesis of cardiac fibrosis: A review of recent progress. Semaphorin3E-PlexinD1 signaling in coronary artery and lymphatic vessel development with clinical implications in myocardial recovery. iScience 24 , Article ADS CAS PubMed PubMed Central Google Scholar. Rockson, S. Estimating the population burden of lymphedema. Article ADS PubMed Google Scholar. Hedrick, M. Lymphatic regulation in nonmammalian vertebrates. Article PubMed Google Scholar. Francis, E. The Anatomy of the Salamander The Clarendon Press, Google Scholar. Kampmeier, O. Evolution and Comparative Morphology of the Lymphatic System Thomas, Duellman, W. Biology of Amphibians Johns Hopkins University Press, Book Google Scholar. On the lymphatic system of Ascaphus; its evolutionary significance. Peyrot, S. Lymph heart musculature is under distinct developmental control from lymphatic endothelium. The development of the jugular lymph sacs in the light of vestigial, provisional and definitive phases of morphogenesis. Mccusker, C. The axolotl limb blastema: Cellular and molecular mechanisms driving blastema formation and limb regeneration in tetrapods. Regeneration 2 , 54—71 Article PubMed PubMed Central Google Scholar. Dunlap, G. Development: How tadpoles ROC tail regeneration. Beck, C. Beyond early development: Xenopus as an emerging model for the study of regenerative mechanisms. Dent, J. Limb regeneration in larvae and metamorphosing individuals of the South African clawed toad. Endo, T. Shh expression in developing and regenerating limb buds of Xenopus laevis. Dyn , — Nye, H. Strategies to reduce variation in Xenopus regeneration studies. Yokoyama, H. FGF stimulates limb regeneration ability in Xenopus laevis. Godwin, J. Scar-free wound healing and regeneration in amphibians: Immunological influences on regenerative success. Differentiation 87 , 66—75 Mescher, A. Limb regeneration in amphibians: Immunological considerations. World J. Article Google Scholar. McCusker, C. Scavelli, C. Lymphatics at the crossroads of angiogenesis and lymphangiogenesis. Crossley, D. Posterior lymph heart function in two species of anurans: Analysis based on both in vivo pressure—volume relationships by conductance manometry and ultrasound. Jones, J. Posterior lymph heart pressure and rate and lymph flow in the toad Bufo marinus in response to hydrated and dehydrated conditions. Ito, R. Overview of lymph node transfer for lymphedema treatment. Yamamoto, T. Indocyanine green lymphography findings in primary leg lymphedema. Narushima, M. Indocyanine green lymphography findings in limb lymphedema. Direct measurement of flow from the posterior lymph hearts of hydrated and dehydrated toads Bufo marinus. Oliver, G. the lymphatic vasculature in the 21st century: Novel functional roles in homeostasis and disease. Cell , — Edwards, J. Lymphatics and bone. Debuque, R. Identification of the adult hematopoietic liver as the primary reservoir for the recruitment of pro-regenerative macrophages required for salamander limb regeneration. Cell Dev. Takaya, K. Gorham-Stout disease with parietal bone osteolysis: A case series and review of literature. Hightower, J. Hemopoietic tissue in the adult newt Notopthalmus viridescens. Lopez, D. Mapping hematopoiesis in a fully regenerative vertebrate: The axolotl. Blood , — Rodgers, A. Identification of immune and non-immune cells in regenerating axolotl limbs by single-cell sequencing. Cell Res. Leigh, N. Transcriptomic landscape of the blastema niche in regenerating adult axolotl limbs at single-cell resolution. Article ADS CAS Google Scholar. Bolaños-Castro, L. Immunity in salamander regeneration: Where are we standing and where are we headed?. Fini, M. Limb regeneration of the adult newt Notophthalmus viridescens in the absence of the spleen. Clavin, N. TGF-β1 is a negative regulator of lymphatic regeneration during wound repair. Heart Circ. Azhar, S. The unresolved pathophysiology of lymphedema. Rusznyák, I. Lymphatics and Lymph Circulation: Physiology and Pathology Pergamon Press, Rumyantsev, P. Ultrastructure of myofibers and cells synthesizing DNA in the developing and regenerating lymph-heart muscles. Jha, S. Efficient activation of the lymphangiogenic growth factor VEGF-C requires the C-terminal domain of VEGF-C and the N-terminal domain of CCBE1. Article CAS Google Scholar. The cardiopharyngeal mesoderm contributes to lymphatic vessel development in mouse. Isl1-expressing non-venous cell lineage contributes to cardiac lymphatic vessel development. Ishiura, R. Successful treatment of large abdominal lymphatic malformations and chylous ascites with intra-abdominal lymphovenous anastomosis. Venous Lymphat. Mihara, M. High-accuracy diagnosis and regional classification of lymphedema using indocyanine green fluorescent lymphography after gynecologic cancer treatment. Mitsui, K. Dual imaging lymphangiography guided treatment of infantile chylothorax. Cases Innov. Akita, S. Improvement of the efficacy of vascularized lymph node transfer for lower-extremity lymphedema via a prefabricated lympho-venous shunt through lymphaticovenular anastomosis between the efferent lymphatic vessel and small vein in the elevated vascularized lymph node. Microsurgery 38 , — Yu, Z. The latent dedifferentiation capacity of newt limb muscles is unleashed by a combination of metamorphosis and body growth. CAS Google Scholar. du Sert, N. The ARRIVE guidelines 2. PLoS Biol. Tanaka, H. A developmentally regulated switch from stem cells to dedifferentiation for limb muscle regeneration in newts. Casco-Robles, R. Novel erythrocyte clumps revealed by an orphan gene Newtic1 in circulating blood and regenerating limbs of the adult newt. Article ADS PubMed PubMed Central Google Scholar. Schneider, C. NIH image to ImageJ: 25 years of image analysis. Methods 9 , — Rueden, C. Image J2: ImageJ for the next generation of scientific image data. BMC Bioinform. Iten, L. Forelimb regeneration from different levels of amputation in the newt, Notophthalmus viridescens : Length, rate, and stages. Wilhelm Roux Arch. Download references. Improved technique for cannulation of the murine thoracic duct: a valuable tool for the dissection of immune responses. J Immunol Methods. Kaipainen A, Korhonen J, Mustonen T, Vanhinsbergh VWM, Fang GH, Dumont D, Breitman M, Alitalo K. Expression of the Fms-like tyrosine kinase-4 gene becomes restricted to lymphatic endothelium during development. Proc Natl Acad Sci U S A. Joukov V, Pajusola K, Kaipainen A, Chilov D, Lahtinen I, Kukk E, Saksela O, Kalkkinen N, Alitalo K. A novel vascular endothelial growth factor, VEGF-C, is a ligand for the Flt4 VEGFR-3 and KDR VEGFR-2 receptor tyrosine kinases vol 15, pg , Embo J. CAS PubMed PubMed Central Google Scholar. Zhou Q, Guo RL, Wood R, Boyce BF, Liang QQ, Wang YJ, Schwarz EM, Xing LP. Vascular endothelial growth factor C attenuates joint damage in chronic inflammatory arthritis by accelerating local lymphatic drainage in mice. Zhang Q, Lu Y, Proulx ST, Guo RL, Yao ZQ, Schwarz EM, Boyce BF, Xing LP. Increased lymphangiogenesis in joints of mice with inflammatory arthritis. Guo RL, Zhou Q, Proulx ST, Wood R, Ji RC, Ritchlin CT, Pytowski B, Zhu ZP, Wang YJ, Schwarz EM, et al. Inhibition of lymphangiogenesis and lymphatic drainage via vascular endothelial growth factor receptor 3 blockade increases the severity of inflammation in a mouse model of chronic inflammatory arthritis. Liang QQ, Ju YW, Chen Y, Wang WS, Li JL, Zhang L, Xu H, Wood RW, Schwarz EM, Boyce BF, et al. Lymphatic endothelial cells efferent to inflamed joints produce iNOS and inhibit lymphatic vessel contraction and drainage in TNF-induced arthritis in mice. Polzer K, Baeten D, Soleiman A, Distler J, Gerlag DM, Tak PP, Schett G, Zwerina J. Tumour necrosis factor blockade increases lymphangiogenesis in murine and human arthritic joints. Ann Rheum Dis. Young A, Koduri G. Extra-articular manifestations and complications of rheumatoid arthritis. Best Pract Res Clin Rheumatol. Robertson MD, Hart FD, White WF, Nuki G, Boardman PL. Rheumatoid lymphadenopathy. Paulus HE, Machlede H, Peter JB, Goldberg L, Levy J, Pearson CM. Clinical improvement of rheumatoid-arthritis during prolonged thoracic-duct lymphocyte drainage. Google Scholar. Paulus HE, Machleder HI, Levine S, Yu DT, MacDonald NS. Lymphocyte involvement in rheumatoid arthritis. Studies during thoracic duct drainage. Paulus HE, Pearson CM, Peter JB, Stratton JA, Whitehou M, Yu D, Bangert R, Machlede H, Goldberg L. Effects of removing thoracic-duct lymphocytes from a patient with severe rheumatoid-arthritis. Article Google Scholar. Paulus HE, Machlede H, Bangert R, Stratton JA, Goldberg L, Whitehou M, Yu D, Pearson CM. Case report—Thoracic-duct lymphocyte drainage in rheumatoid-arthritis. Clin Immunol Immunop. Pullinger BD, Florey HW. Proliferation of lymphatics in inflammation. J Path Bacteriol. Andersson I, Marsal L, Nilsson B, Sjoblom KG, Wollheim FA. Abnormal axillary lymph nodes in rheumatoid arthritis. Acta Radiol Diagn Stockh. CAS Google Scholar. Olszewski WL, Pazdur J, Kubasiewicz E, Zaleska M, Cooke CJ, Miller NE. Lymph draining from foot joints in rheumatoid arthritis provides insight into local cytokine and chemokine production and transport to lymph nodes. Kallioma J, Vastamak M. Chronic diffuse oedema of rheumatoid hand—a sign of local lymphatic involvement. Hart FD. Lymphadenopathy in rheumatic patients. Bohm M, Riemann B, Luger TA, Bonsmann G. Bilateral upper limb lymphoedema associated with psoriatic arthritis: a case report and review of the literature. Br J Dermatol. Sant SM, Tormey VJ, Freyne P, Casey EB. Lymphatic obstruction in rheumatoid-arthritis. Clin Rheumatol. Mulherin DM, Fitzgerald O, Bresnihan B. Lymphedema of the upper limb in patients with psoriatic-arthritis. Semin Arthritis Rheum. Kiely PDW, Bland JM, Joseph AEA, Mortimer PS, Bourke BE. Upper-limb lymphatic function in inflammatory arthritis. CAS PubMed Google Scholar. Proulx ST, Kwok E, You Z, Beck CA, Shealy DJ, Ritchlin CT, Boyce BF, Xing L, Schwarz EM. MRI and quantification of draining lymph node function in inflammatory arthritis. Ann N Y Acad Sci. Proulx ST, Kwok E, You Z, Papuga MO, Beck CA, Shealy DJ, Calvi LM, Ritchlin CT, Awad HA, Boyce BF, et al. Elucidating bone marrow edema and myelopoiesis in murine arthritis using contrast-enhanced magnetic resonance imaging. Proulx ST, Kwok E, You Z, Papuga MO, Beck CA, Shealy DJ, Ritchlin CT, Awad HA, Boyce BF, Xing L, et al. Longitudinal assessment of synovial, lymph node, and bone volumes in inflammatory arthritis in mice by in vivo magnetic resonance imaging and microfocal computed tomography. McQueen FM. Magnetic resonance imaging in early inflammatory arthritis: what is its role? Rheumatology Oxford. Li J, Ju YW, Bouta EM, Xing LP, Wood RW, Kuzin I, Bottaro A, Ritchlin CT, Schwarz EM. Efficacy of B cell depletion therapy for murine joint arthritis flare is associated with increased lymphatic flow. Li J, Ritchlin CT, Sanz I, Bottaro A, Wood R, Xing LP, Schwarz EM. Effective anti-CD20 therapy for arthritis is associated with B-cell depletion in efferent lymph nodes and increased lymph and cellular flow in lymphatic vessels from arthritic joints. Zhou Q, Guo RL, Wood R, Proulx ST, Schwarz EM, Boyce BF, Xing LP. Blockade of lymphangiogenesis and lymphatic draining function enhances the severity of synovitis in mice with inflammatory-erosive arthritis. Li J, Kuzin I, Moshkani S, Proulx ST, Xing L, Skrombolas D, Dunn R, Sanz I, Schwarz EM, Bottaro A. J Immunol. Li J, Zhou Q, Wood R, Kuzin I, Bottaro A, Ritchlin C, Xing L, Schwarz E. Bouta EM, Wood RW, Brown EB, Rahimi H, Ritchlin CT, Schwarz EM. In vivo quantification of lymph viscosity and pressure in lymphatic vessels and draining lymph nodes of arthritic joints in mice. J Physiol. Bremander ABI, Petersson IF, Roos E. Validation of the rheumatoid arthritis outcome score RAOS —for the lower extremity. Health Qual Life Outcomes. Huh YM, Kim S, Suh JS, Song HT, Song K, Shin KH. The role of popliteal lymph nodes in differentiating rheumatoid arthritis from osteoarthritis by using CE 3D-FSPGR MR imaging: relationship of the inflamed synovial volume. Korean J Radiol. Gaffney K, Cookson J, Blades S, Coumbe A, Blake D. Quantitative assessment of the rheumatoid synovial microvascular bed by gadolinium-DTPA enhanced magnetic resonance imaging. Ostergaard M, Hansen M, Stoltenberg M, Gideon P, Klarlund M, Jensen KE, Lorenzen I. Magnetic resonance imaging-determined synovial membrane volume as a marker of disease activity and a predictor of progressive joint destruction in the wrists of patients with rheumatoid arthritis. Tan YK, Ostergaard M, Conaghan PG. Imaging tools in rheumatoid arthritis: ultrasound vs magnetic resonance imaging. van de Stadt LA, Bos WH, Meursinge Reynders M, Wieringa H, Turkstra F, van der Laken CJ, van Schaardenburg D. The value of ultrasonography in predicting arthritis in auto-antibody positive arthralgia patients: a prospective cohort study. Foltz V, Gandjbakhch F, Etchepare F, Rosenberg C, Tanguy ML, Rozenberg S, Bourgeois P, Fautrel B. Power Doppler ultrasound, but not low-field magnetic resonance imaging, predicts relapse and radiographic disease progression in rheumatoid arthritis patients with low levels of disease activity. Peluso G, Michelutti A, Bosello S, Gremese E, Tolusso B, Ferraccioli G. Clinical and ultrasonographic remission determines different chances of relapse in early and long standing rheumatoid arthritis. Manzo A, Caporali R, Vitolo B, Alessi S, Benaglio F, Todoerti M, Bugatti S, Calliada F, Montecucco C. Subclinical remodelling of draining lymph node structure in early and established rheumatoid arthritis assessed by power Doppler ultrasonography. Clavel G, Marchiol-Fournigault C, Renault G, Boissier MC, Fradelizi D, Bessis N. Ultrasound and Doppler micro-imaging in a model of rheumatoid arthritis in mice. Hammer HB, Sveinsson M, Kongtorp AK, Kvien TK. A joints ultrasonographic assessment is associated with clinical assessments and is highly responsive to improvement in a longitudinal study of patients with rheumatoid arthritis starting adalimumab treatment. Hartung W, Kellner H, Strunk J, Sattler H, Schmidt WA, Ehrenstein B, Fleck M, Backhaus M. Development and evaluation of a novel ultrasound score for large joints in rheumatoid arthritis: one year of experience in daily clinical practice. Arthritis Care Res Hoboken. Szkudlarek M, Court-Payen M, Jacobsen S, Klarlund M, Thomsen HS, Ostergaard M. Interobserver agreement in ultrasonography of the finger and toe joints in rheumatoid arthritis. Ju Y, Rahimi H, Li J, Wood RW, Xing L, Schwarz EM. Validation of 3-dimensional ultrasound versus magnetic resonance imaging quantification of popliteal lymph node volume as a biomarker of erosive inflammatory arthritis in mice. Bouta EM, Banik PD, Wood RW, Rahimi H, Ritchlin CT, Thiele RG, Schwarz EM. Validation of power Doppler versus contrast-enhanced magnetic resonance imaging quantification of joint inflammation in murine inflammatory arthritis. J Bone Miner Res. Nimura H, Narimiya N, Mitsumori N, Yamazaki Y, Yanaga K, Urashima M. Infrared ray electronic endoscopy combined with indocyanine green injection for detection of sentinel nodes of patients with gastric cancer. Br J Surg. Ito N, Fukuta M, Tokushima T, Nakai K, Ohgi S. Sentinel node navigation surgery using indocyanine green in patients with lung cancer. Surg Today. Rasmussen JC, Tan IC, Marshall MV, Fife CE, Sevick-Muraca EM. Lymphatic imaging in humans with near-infrared fluorescence. Curr Opin Biotech. Tan I, Maus E, Rasmussen J, Marshall M, Fife CE, Smith L, Sevick EM. Near-infrared fluorescence imaging of lymphatics in head and neck lymphedema. J Nucl Med. Tan IC, Maus EA, Rasmussen JC, Marshall MV, Adams KE, Fife CE, Smith LA, Chan W, Sevick-Muraca EM. Assessment of lymphatic contractile function after manual lymphatic drainage using near-infrared fluorescence imaging. Arch Phys Med Rehab. Rasmussen JC, Tan IC, Marshall MV, Adams KE, Kwon S, Fife CE, Maus EA, Smith LA, Covington KR, Sevick-Muraca EM. Human lymphatic architecture and dynamic transport imaged using near-infrared fluorescence. Transl Oncol. Shaw RA, Kotowich S, Eysel HH, Jackson M, Thomson GTD, Mantsch HH. Arthritis diagnosis based upon the near infrared spectrum of synovial fluid. Rheumatol Int. Chen WT, Mahmood U, Weissleder R, Tung CH. Arthritis imaging using a near-infrared fluorescence folate-targeted probe. Hansch A, Frey O, Sauner D, Hilger I, Haas M, Malich A, Brauer R, Kaiser WA. In vivo imaging of experimental arthritis with near-infrared fluorescence. Fischer T, Gemeinhardt I, Wagner S, von Stieglitz D, Schnorr J, Hermann KGA, Ebert B, Petzelt D, MacDonald R, Licha K, et al. Assessment of unspecific near-infrared dyes in laser-induced fluorescence imaging of experimental arthritis. Acad Radiol. Krohn M, Ohrndorf S, Werner SG, Schicke B, Burmester GR, Hamm B, Backhaus M, Hermann KGA. Near-infrared fluorescence optical imaging in early rheumatoid arthritis: a comparison to magnetic resonance imaging and ultrasonography. Download references. HR is supported by grants from NIH AR and AR RB and EMB are supported by a NIH training grant AR RWW is supported by a NIH grant AR LX is supported by NIH grants AR, AR, and University of Rochester CTSA award UL1 TR , a grant from the National Natural Science Foundation of China , and a grant from the Lymphatic Malformation Institute. EMS is supported by grants from NIH P01 AI, AR and AR CTR receives consulting fees and research support from UCB Pharmaceuticals. The remaining authors declare that they have no competing interests. It is more difficult to read a mammogram if the breast tissue is dense so mammograms are not as reliable for younger women. Specialists have found that older women who take hormone replacement therapy HRT have denser breasts than would be expected for their age, which can make their mammograms less accurate. Most women are aware of the common risk factors when it comes to breast cancer. However, many are not aware of the importance of breast density, which has been described as one of the most significant risk factors of all. Women with dense breasts have a higher proportion of fibroglandular and supportive tissue, whereas those with less dense breasts have a higher proportion of fat. Unfortunately, breast density cannot be measured by look or feel, only by mammography, where dense breast tissue appears white and fatty breast tissue appears dark. Breast density cannot be measured by look or feel, only by mammography, where dense breast tissue appears white and fatty breast tissue appears dark. These are the women who are at risk of a cancer not being picked up by mammogram as dense breast look white on a mammogram and cancer looks white on a mammogram. Currently, women in Ireland going through the BreastCheck mammographic screening programme are not routinely informed about their breast density when receiving their results, and many are unaware of this important risk-factor. It collects fluid, waste material, and other things such as viruses and bacteria that are in the body tissues, outside the bloodstream. In the same way that veins collect and carry blood through the body, lymph vessels carry a watery yellow fluid called lymph. Lymph flows through the lymphatic system and eventually drains into veins. This system helps to get rid of waste products from the body. Lymph nodes are important in cancer care because any cancer cells that have broken away from a cancerous tumour can be carried by the tissue fluid to the nearest lymph nodes. If your doctors finds a cancerous tumour, they will always examine your lymph nodes to see if there are cancer cells present there. If there are no cancer cells in the nearby lymph glands, your cancer is less likely to have spread. Sometimes lymph nodes become enlarged for other reasons that are not related to cancer e. Your breast tissue extends to under your armpit. The armpits have many lymph nodes, also known as lymph glands. There is also a chain of lymph nodes that runs up the center of your chest, by your breast bone. This is called the internal mammary chain. The diagram shows the network of lymph nodes around the breast. Because your breast tissue extends to your collar bone and your armpit, it is important to check these areas during your monthly breast self-examination. We hope you found this information useful. The Marie Keating Foundation offers all of our services for free. Help support people at every step of a cancer journey by making a donation today. Necessary cookies are absolutely essential for the website to function properly. These cookies ensure basic functionalities and security features of the website, anonymously. Cookie Duration Description PHPSESSID session This cookie is native to PHP applications. The cookie is used to store and identify a users' unique session ID for the purpose of managing user session on the website. The cookie is a session cookies and is deleted when all the browser windows are closed. It does not store any personal data. It does not correspond to any user ID in the web application and does not store any personally identifiable information. This cookie is used to enable payment on the website without storing any patment information on a server. Advertisement cookies are used to provide visitors with relevant ads and marketing campaigns. These cookies track visitors across websites and collect information to provide customized ads. Cookie Duration Description bscookie 2 years This cookie is a browser ID cookie set by Linked share Buttons and ad tags. fr 3 months The cookie is set by Facebook to show relevant advertisments to the users and measure and improve the advertisements. |
0 thoughts on “BIA lymphatic system assessment”