
Oral medication for gestational diabetes -
Pharmacotherapy eg, metformin , pioglitazone may also have a role in preventing future type 2 diabetes. In a multicenter randomized trial, both intensive lifestyle and metformin therapy reduced the incidence of future diabetes by approximately 50 percent compared with placebo in patients with a history of GDM; metformin was much more effective than lifestyle intervention in parous patients with previous GDM [ ].
This topic is discussed in detail separately. See "Prevention of type 2 diabetes mellitus". Reassessment of glycemic status should be undertaken at a minimum of every three years eg, every one to three years [ 24 ].
More frequent assessment may be important in patients who may become pregnant again, since early detection of diabetes is important to preconception and early prenatal care. More frequent screening every one or two years may also be indicated in patients with other risk factors for diabetes, such as family history of diabetes, obesity, and need for pharmacotherapy during pregnancy.
The best means of follow-up testing has not been defined. The two-hour 75 g oral GTT is the more sensitive test for diagnosis of diabetes and impaired glucose tolerance in most populations, but the fasting plasma glucose is more convenient, specific, and reproducible, and less expensive.
A1C is convenient and the preferred test for patients who have not fasted overnight. See "Screening for type 2 diabetes mellitus", section on 'Screening tests'.
See "Overview of primary prevention of cardiovascular disease". Follow-up of patients not screened for GDM — For patients who did not undergo screening for GDM, but diabetes is suspected postpartum because of newborn outcome eg, hypoglycemia, macrosomia, congenital anomalies , a postpartum GTT may be considered.
A normal postpartum GTT excludes the presence of type 1 or type 2 diabetes or prediabetes; it does not exclude the possibility of GDM during pregnancy and the future risks associated with this diagnosis. Indications for screening and tests used for screening are discussed separately.
See "Screening for type 2 diabetes mellitus". SOCIETY GUIDELINE LINKS — Links to society and government-sponsored guidelines from selected countries and regions around the world are provided separately.
See "Society guideline links: Diabetes mellitus in pregnancy". These articles are best for patients who want a general overview and who prefer short, easy-to-read materials.
Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed. These articles are written at the 10th to 12th grade reading level and are best for patients who want in-depth information and are comfortable with some medical jargon.
Here are the patient education articles that are relevant to this topic. We encourage you to print or e-mail these topics to your patients. You can also locate patient education articles on a variety of subjects by searching on "patient info" and the keyword s of interest. We suggest glucose self-monitoring before breakfast and at one or at two hours after the beginning of each meal.
See 'Glucose monitoring' above. See 'Can the frequency of self-monitoring be reduced? Moderate exercise also improves glycemic control and should be part of the treatment plan for patients with no medical or obstetric contraindications to this level of physical activity. See 'Rationale for treatment' above and 'Exercise' above.
Calories are generally divided over three meals and two to four snacks per day and are composed of approximately 40 percent carbohydrate, 20 percent protein, and 40 percent fat.
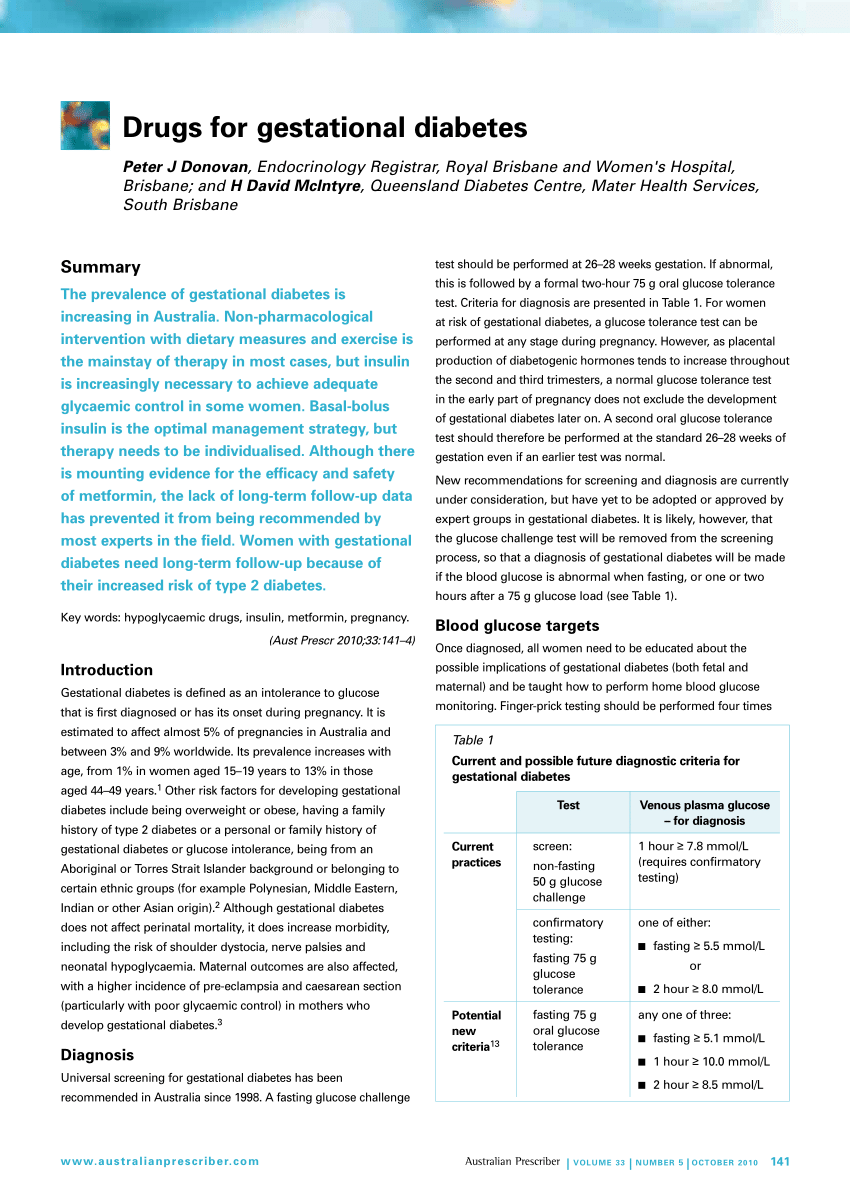
Gestational weight gain recommendations are shown in the table table 1. See 'Medical nutritional therapy' above. Pharmacotherapy can reduce the occurrence of macrosomia and large for gestational age in newborns.
See 'Indications for pharmacotherapy' above. We start with the simplest insulin regimen likely to be effective based on the glucose levels recorded in the patient's blood glucose log and increase the complexity as needed. An alternative approach based on both patient weight and glucose levels is somewhat more complex and likely most appropriate for individuals whose glucose levels are not well managed with simpler paradigms.
See 'Insulin' above. The long-term effects of transplacental passage of noninsulin antihyperglycemic agents are not known. See 'Oral hypoglycemic agents' above. Testing can be performed while the patient is still in the hospital after giving birth. Otherwise it is performed 4 to 12 weeks postpartum and, if results are normal, at least every three years thereafter.
See 'Maternal prognosis' above. Why UpToDate? Product Editorial Subscription Options Subscribe Sign in. Learn how UpToDate can help you. Select the option that best describes you. View Topic.
Font Size Small Normal Large. Gestational diabetes mellitus: Glucose management and maternal prognosis. Formulary drug information for this topic. No drug references linked in this topic. Find in topic Formulary Print Share. View in. Language Chinese English.
Author: Celeste Durnwald, MD Section Editors: David M Nathan, MD Erika F Werner, MD, MS Deputy Editor: Vanessa A Barss, MD, FACOG Contributor Disclosures.
All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Jan This topic last updated: Nov 16, There were no significant maternal or neonatal harms from treatment of GDM.
Insulin Dose — The insulin dose required to achieve target glucose levels varies among individuals, but the majority of studies have reported a total dose ranging from 0.
Follow-up Testing — Long-term follow-up for development of type 2 diabetes is routinely recommended for individuals with GDM, given their high risk for developing the disorder [ 24,43 ]. Electronic address: pubs smfm.
SMFM Statement: Pharmacological treatment of gestational diabetes. Am J Obstet Gynecol ; B2. Catalano PM, McIntyre HD, Cruickshank JK, et al.
The hyperglycemia and adverse pregnancy outcome study: associations of GDM and obesity with pregnancy outcomes. Diabetes Care ; Crowther CA, Hiller JE, Moss JR, et al. Effect of treatment of gestational diabetes mellitus on pregnancy outcomes. N Engl J Med ; HAPO Study Cooperative Research Group, Metzger BE, Lowe LP, et al.
Hyperglycemia and adverse pregnancy outcomes. Han S, Crowther CA, Middleton P. Interventions for pregnant women with hyperglycaemia not meeting gestational diabetes and type 2 diabetes diagnostic criteria.
Cochrane Database Syst Rev ; 1:CD Durnwald CP, Mele L, Spong CY, et al. Glycemic characteristics and neonatal outcomes of women treated for mild gestational diabetes. Obstet Gynecol ; Uvena-Celebrezze J, Fung C, Thomas AJ, et al.
Relationship of neonatal body composition to maternal glucose control in women with gestational diabetes mellitus. J Matern Fetal Neonatal Med ; Catalano PM, Thomas A, Huston-Presley L, Amini SB. Increased fetal adiposity: a very sensitive marker of abnormal in utero development.
Am J Obstet Gynecol ; Moss JR, Crowther CA, Hiller JE, et al. Costs and consequences of treatment for mild gestational diabetes mellitus - evaluation from the ACHOIS randomised trial.
BMC Pregnancy Childbirth ; US Preventive Services Task Force, Davidson KW, Barry MJ, et al. Screening for Gestational Diabetes: US Preventive Services Task Force Recommendation Statement.
JAMA ; Pillay J, Donovan L, Guitard S, et al. Screening for Gestational Diabetes: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force.
Poprzeczny AJ, Louise J, Deussen AR, Dodd JM. The mediating effects of gestational diabetes on fetal growth and adiposity in women who are overweight and obese: secondary analysis of the LIMIT randomised trial. BJOG ; Landon MB, Rice MM, Varner MW, et al. Mild gestational diabetes mellitus and long-term child health.
American Diabetes Association, Bantle JP, Wylie-Rosett J, et al. Nutrition recommendations and interventions for diabetes: a position statement of the American Diabetes Association.
Diabetes Care ; 31 Suppl 1:S Landon MB, Spong CY, Thom E, et al. A multicenter, randomized trial of treatment for mild gestational diabetes. Hernandez TL, Brand-Miller JC. Nutrition Therapy in Gestational Diabetes Mellitus: Time to Move Forward.
Yamamoto JM, Kellett JE, Balsells M, et al. Gestational Diabetes Mellitus and Diet: A Systematic Review and Meta-analysis of Randomized Controlled Trials Examining the Impact of Modified Dietary Interventions on Maternal Glucose Control and Neonatal Birth Weight.
Han S, Middleton P, Shepherd E, et al. Different types of dietary advice for women with gestational diabetes mellitus. Cochrane Database Syst Rev ; 2:CD Hernandez TL, Mande A, Barbour LA. Nutrition therapy within and beyond gestational diabetes.
Diabetes Res Clin Pract ; Feinman RD, Pogozelski WK, Astrup A, et al. Dietary carbohydrate restriction as the first approach in diabetes management: critical review and evidence base. Nutrition ; Jovanovic-Peterson L, Peterson CM.
Dietary manipulation as a primary treatment strategy for pregnancies complicated by diabetes. J Am Coll Nutr ; Reece EA, Hagay Z, Caseria D, et al.
Do fiber-enriched diabetic diets have glucose-lowering effects in pregnancy? Am J Perinatol ; Okesene-Gafa KA, Moore AE, Jordan V, et al. Probiotic treatment for women with gestational diabetes to improve maternal and infant health and well-being.
Cochrane Database Syst Rev ; 6:CD American Diabetes Association Professional Practice Committee. Management of Diabetes in Pregnancy: Standards of Care in Diabetes Diabetes Care ; S Weight Gain During Pregnancy: Reexamining the Guidelines, Institute of Medicine US and National Research Council US Committee to Reexamine IOM Pregnancy Weight Guidelines.
Ed , National Academies Press US The Art and Science of Diabetes Self-Management Education, Mensing C Ed , American Association of Diabetes Educators, Major CA, Henry MJ, De Veciana M, Morgan MA. The effects of carbohydrate restriction in patients with diet-controlled gestational diabetes. Peterson CM, Jovanovic-Peterson L.
Percentage of carbohydrate and glycemic response to breakfast, lunch, and dinner in women with gestational diabetes. Diabetes ; 40 Suppl Viana LV, Gross JL, Azevedo MJ. Dietary intervention in patients with gestational diabetes mellitus: a systematic review and meta-analysis of randomized clinical trials on maternal and newborn outcomes.
Cheng YW, Chung JH, Kurbisch-Block I, et al. Gestational weight gain and gestational diabetes mellitus: perinatal outcomes. Franz MJ, Bantle JP, Beebe CA, et al. Evidence-based nutrition principles and recommendations for the treatment and prevention of diabetes and related complications. Brown J, Ceysens G, Boulvain M.
Exercise for pregnant women with gestational diabetes for improving maternal and fetal outcomes. Laird J, McFarland KF. Fasting blood glucose levels and initiation of insulin therapy in gestational diabetes. Endocr Pract ; Weisz B, Shrim A, Homko CJ, et al.
One hour versus two hours postprandial glucose measurement in gestational diabetes: a prospective study. J Perinatol ; Moses RG, Lucas EM, Knights S. Gestational diabetes mellitus. At what time should the postprandial glucose level be monitored?
Aust N Z J Obstet Gynaecol ; Sivan E, Weisz B, Homko CJ, et al. One or two hours postprandial glucose measurements: are they the same? de Veciana M, Major CA, Morgan MA, et al. Postprandial versus preprandial blood glucose monitoring in women with gestational diabetes mellitus requiring insulin therapy.
Hawkins JS, Casey BM, Lo JY, et al. Weekly compared with daily blood glucose monitoring in women with diet-treated gestational diabetes. Metzger BE, Buchanan TA, Coustan DR, et al. Summary and recommendations of the Fifth International Workshop-Conference on Gestational Diabetes Mellitus.
Diabetes Care ; 30 Suppl 2:S Mendez-Figueroa H, Schuster M, Maggio L, et al. Gestational Diabetes Mellitus and Frequency of Blood Glucose Monitoring: A Randomized Controlled Trial. Raman P, Shepherd E, Dowswell T, et al.
Different methods and settings for glucose monitoring for gestational diabetes during pregnancy. Cochrane Database Syst Rev ; CD Hofer OJ, Martis R, Alsweiler J, Crowther CA. Different intensities of glycaemic control for women with gestational diabetes mellitus.
ACOG Practice Bulletin No. Obstet Gynecol ; e Hernandez TL, Friedman JE, Van Pelt RE, Barbour LA. Patterns of glycemia in normal pregnancy: should the current therapeutic targets be challenged? Griffiths RJ, Vinall PS, Stickland MH, Wales JK. Haemoglobin A1c levels in normal and diabetic pregnancies.
Eur J Obstet Gynecol Reprod Biol ; Jovanovic L, Savas H, Mehta M, et al. Frequent monitoring of A1C during pregnancy as a treatment tool to guide therapy.
Mosca A, Paleari R, Dalfrà MG, et al. Reference intervals for hemoglobin A1c in pregnant women: data from an Italian multicenter study. Clin Chem ; Lurie S, Mamet Y. Red blood cell survival and kinetics during pregnancy. Bunn HF, Haney DN, Kamin S, et al. The biosynthesis of human hemoglobin A1c.
Slow glycosylation of hemoglobin in vivo. J Clin Invest ; Bergenstal RM, Gal RL, Connor CG, et al. Racial Differences in the Relationship of Glucose Concentrations and Hemoglobin A1c Levels. Ann Intern Med ; Pinto ME, Villena JE. Diabetic ketoacidosis during gestational diabetes.
A case report. Diabetes Res Clin Pract ; e Graham UM, Cooke IE, McCance DR. A case of euglyacemic diabetic ketoacidosis in a patient with gestational diabetes mellitus.
Obstet Med ; Robinson HL, Barrett HL, Foxcroft K, et al. Prevalence of maternal urinary ketones in pregnancy in overweight and obese women.
Stehbens JA, Baker GL, Kitchell M. Outcome at ages 1, 3, and 5 years of children born to diabetic women. Churchill JA, Berendes HW, Nemore J. Neuropsychological deficits in children of diabetic mothers. A report from the Collaborative Sdy of Cerebral Palsy. Rizzo T, Metzger BE, Burns WJ, Burns K.
Correlations between antepartum maternal metabolism and intelligence of offspring. Naeye RL, Chez RA. Effects of maternal acetonuria and low pregnancy weight gain on children's psychomotor development.
Knopp RH, Magee MS, Raisys V, Benedetti T. Metabolic effects of hypocaloric diets in management of gestational diabetes. Langer O, Levy J, Brustman L, et al.
Glycemic control in gestational diabetes mellitus--how tight is tight enough: small for gestational age versus large for gestational age? Kjos SL, Schaefer-Graf U, Sardesi S, et al. A randomized controlled trial using glycemic plus fetal ultrasound parameters versus glycemic parameters to determine insulin therapy in gestational diabetes with fasting hyperglycemia.
Nicholson WK, Wilson LM, Witkop CT, et al. Therapeutic management, delivery, and postpartum risk assessment and screening in gestational diabetes. Evid Rep Technol Assess Full Rep ; Harrison RK, Cruz M, Wong A, et al.
The timing of initiation of pharmacotherapy for women with gestational diabetes mellitus. Balsells M, García-Patterson A, Gich I, Corcoy R. Ultrasound-guided compared to conventional treatment in gestational diabetes leads to improved birthweight but more insulin treatment: systematic review and meta-analysis.
Acta Obstet Gynecol Scand ; Though gastrointestinal side effects were more common with Acarbose, the study showed that there were no appreciable differences between acarbose and insulin in fasting or postprandial glucose levels.
Even other studies indicated that acarbose is less successful than glyburide at establishing glycemic control, it also showed that acarbose had a reduced incidence of hypoglycemia and macrosomia, making it an appealing drug for further investigations on the treatment of GDM.
Acarbose was deemed an efficient option for GDM control and appeared to be well-tolerated in a subsequent research by Jayasingh, et al. In the research trials, feto-maternal outcomes in pregnant GDM patients treated with insulin or acarbose were compared.
Recurring infections, preeclampsia, premature membrane rupture, delivery methods, postoperative random levels of blood glucose, fasting blood glucose level at day 7, fasting blood glucose level after six weeks, and mean birth weight of offspring were not significantly changed between the two groups.
Recent investigations have not found a markedly greater risk of liver damage following acarbose medication, despite the fact that acarbose has been associated with hepatic failure and abnormal liver enzymes in diabetic persons [51]. Acarbose can pass the placenta and is not teratogenic at dosages up to 32 times greater than those used in humans, according to animal studies.
However, the medication has the ability to induce labour by causing stomach cramping and increasing prostaglandin E levels. Research is currently being done to determine whether vitamin and mineral supplements are useful for GDM sufferers. Vitamin E, vitamin D, and magnesium levels have been discovered to be low in GDM patients, despite the fact that these nutrients have been favorably associated with controlled glucose metabolism, anti-inflammatory effects, and decreased oxidative stress when taken as supplements.
Li, et al. most recent meta-analysis backs up these conclusions. Additionally, it has been discovered that providing GDM women with Mg-Zn-Ca-vitamin D co-supplements for six weeks reduces oxidative stress and inflammation.
According to Wang, et al. vitamin D supplementation can enhance glycemic management and decrease negative feto-maternal outcomes, such as Caesarean sections, postpartum hemorrhages, hospitalization of mothers, newborn hyperbilirubinemia, big children, fetal distress, polyhydramnios, and preterm birth [52].
Most women with GDM can attain normoglycemia with dietary changes and lifestyle changes, especially when it comes to the kind and quantity of dietary carbs. When taken soon after the diagnosis of GDM, myoinositol, a dietary supplement known to lower insulin resistance, has been demonstrated to be useful in establishing glycemic control and lowering the requirement for further medication [53].
Studies are also being done on the possibilities of treating GDM using herbal remedies and conventional Chinese medicine. Herbs like Zuo Gui Wan, red raspberry tea, and Orthosiphon stamineus have all shown promise in decreasing glucose and relieving GDM-related symptoms, with good safety profiles for both mother and infant.
The glycyrrhiza flavonoids from traditional Chinese medicine have also been demonstrated to have anti-diabetic potential as adjuvants for insulin therapy [54]. Probiotic supplementation is an area of study that shows promise for enhancing glycemic control and lowering GDM-related adverse events, but more research is required to fully appreciate its advantages.
Despite the fact that fresh and promising outcomes are frequently published, dependable and long-lasting results in the field of adjuvant GDM therapy require standardized methods and well-designed trials [55]. GDM is a significant issue that needs to be managed effectively to prevent negative consequences on the mother and fetus.
This chapter discusses potential pharmacological therapies for GDM, their special traits, advantages, and drawbacks. Oral medications like glyburide and metformin are the most recommended first-line therapies, but if optimal glucose control is not achieved, analogues such as aspart, lispro, and detemir may be required.
Patient evaluation is crucial to selecting the best treatment option. Education about the advantages and disadvantages of different treatment modalities is also necessary.
Future clinical research will provide more knowledge on the prevention and management of GDM. The conclusion can be further condensed if needed. Managing gestational diabetes is critical for the healthcare sector to prevent negative outcomes for mothers and infants.
This review article on pharmacological therapies provides an overview of treatment options. However, improvements are necessary.
There should be more information on early screening and diagnosis, insulin analogues, complementary therapies, nutrition, and long-term effects on health outcomes. Patient education and involvement are critical for optimal glycemic control. The article should also clarify the FDA pregnancy risk categories for the medications discussed, especially glyburide.
Incorporating these recommendations can enhance the article's reliability for healthcare providers and expecting mothers. Order for reprints. PTZ: We're glad you're here. Please click "create a new query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query. Toggle navigation. ISSN: Review Article Open Access Peer-Reviewed.
Author and article information. Department of Gynecology and Obstetrics Unit-II , Bolan Medical Complex Hospital Quetta, Pakistan. Received: 23 August, Accepted: 01 September, Published: 02 September, Keywords: Gestation; Diabetes; Management; Therapies; GDM.
Cite this as Akram S, Bibi S Review on pharmacological therapies for management of gestational diabetes. Int J Pharm Sci Dev Res 9 1 : DOI: This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Indexing and Abstracting. Main article text. Introduction Gestational Diabetes Mellitus GDM is a distinct endocrine disorder resulting in glucose intolerance that may occur during pregnancy.
Current pharmacological options for GDM A. Insulin and its analogues Pharmacological use and properties: Insulin is considered a safe and effective treatment for Gestational Diabetes Mellitus GDM due to its inability to pass through the placenta unless administered in high doses.
Oral anti-hyperglycemic drugs OAD i. Metformin Pharmacological use and properties: The oral biguanide metformin reduces gluconeogenesis in the liver, boosts peripheral insulin sensitivity, and encourages glucose uptake in peripheral tissues while inhibiting gut glucose absorption [26].
Glyburide Pharmacological use and properties: A second-generation sulfonylurea, glyburide mainly increases pancreatic and peripheral tissue insulin sensitivity. Acarbose Pharmacological use and properties: The alpha-glucosidase inhibitor acarbose stops the digestive enzymes of the small intestine from breaking down starches into simple sugars.
Supplementation and traditional treatment options Research is currently being done to determine whether vitamin and mineral supplements are useful for GDM sufferers.
Conclusion GDM is a significant issue that needs to be managed effectively to prevent negative consequences on the mother and fetus. Recommendations Managing gestational diabetes is critical for the healthcare sector to prevent negative outcomes for mothers and infants.
Rosik J, Szostak B, Machaj F, Pawlik A. The role of genetics and epigenetics in the pathogenesis of gestational diabetes mellitus. Ann Hum Genet. doi: Epub Oct 1.
PMID: McIntyre HD, Catalano P, Zhang C, Desoye G, Mathiesen ER, Damm P. Gestational diabetes mellitus. Nat Rev Dis Primers. Franzago M, Fraticelli F, Stuppia L, Vitacolonna E.
Nutrigenetics, epigenetics and gestational diabetes: consequences in mother and child. Epub Mar PMID: ; PMCID: PMC Radenkovic M. Treatment considerations for gestational diabetes mellitus and long-term postpartum options.
In: Gestational Diabetes. Insulin therapy and its consequences for the mother, foetus, and newborn in gestational diabetes mellitus. Biochim Biophys Acta Mol Basis Dis.
Epub Jun 8. Singh KP, Rahimpanah F, Barclay M. Metformin for the management of gestational diabetes mellitus. Aust N Z J Obstet Gynaecol. Epub Apr Gou BH, Guan HM, Bi YX, Ding BJ. Gestational diabetes: weight gain during pregnancy and its relationship to pregnancy outcomes.
Chin Med J Engl. Mirabelli M, Chiefari E, Tocci V, Greco E, Foti D, Brunetti A. Gestational diabetes: Implications for fetal growth, intervention timing, and treatment options.
Curr Opin Pharmacol. Epub Jul Lorenzo-Almorós A, Hang T, Peiró C, Soriano-Guillén L, Egido J, Tuñón J, Lorenzo Ó. Predictive and diagnostic biomarkers for gestational diabetes and its associated metabolic and cardiovascular diseases.
Cardiovasc Diabetol. Szmuilowicz ED, Josefson JL, Metzger BE. Gestational Diabetes Mellitus. Endocrinol Metab Clin North Am. Epub Jun Żurawska-Kliś M, Czarnik K, Szymczak S, Wójcik M, Cypryk K.
Acta Diabetol. Epub Feb Langer O, Conway DL, Berkus MD, Xenakis EM, Gonzales O. A comparison of glyburide and insulin in women with gestational diabetes mellitus. N Engl J Med. Bidhendi Yarandi R, Amiri M, Ramezani Tehrani F, Behboudi-Gandevani S.
Effectiveness of antidiabetic agents for treatment of gestational diabetes: A methodological quality assessment of meta-analyses and network meta-analysis. J Diabetes Investig. Sheiner E. Gestational Diabetes Mellitus: Long-Term Consequences for the Mother and Child Grand Challenge: How to Move on Towards Secondary Prevention?
Front Clin Diabetes Healthc. Challier JC, Hauguel S, Desmaizieres V. Effect of insulin on glucose uptake and metabolism in the human placenta. J Clin Endocrinol Metab. Martis R, Crowther CA, Shepherd E, Alsweiler J, Downie MR, Brown J. You'll also need to be more closely monitored during pregnancy and labour to check if treatment is working and for any problems.
You'll be given a testing kit that you can use to check your blood sugar glucose level. This involves using a finger-pricking device and putting a drop of blood on a testing strip. If you take insulin and have problems with low blood sugar hypoglycaemia or your blood sugar is not stable, your care team might offer you a continuous glucose monitor CGM.
This is a small sensor you wear on your skin that sends data wirelessly to a receiver or a mobile phone, so you can see your blood sugar level at any time. Diabetes UK has more information about checking your blood sugar levels.
You should be referred to a dietitian, who can give you advice about your diet and how to plan healthy meals. It's also important to be aware of foods to avoid during pregnancy , such as certain types of fish and cheese.
Diabetes UK: What can I eat with gestational diabetes? Diabetes UK: Glycaemic index GI and diabetes. Physical activity lowers your blood glucose level, so regular exercise can be an effective way to manage gestational diabetes.
You'll be advised about safe ways to exercise during pregnancy. Find out more about exercise in pregnancy. A common recommendation is to aim for at least minutes 2 hours and 30 minutes of moderate-intensity activity a week, plus strength exercises on 2 or more days a week. You may be given medicine if your blood sugar levels are still not stable 1 to 2 weeks after changing your diet and exercising regularly, or if your blood sugar level is very high when you're first diagnosed.
This may be tablets — usually metformin — or insulin injections. Your blood sugar levels can increase as your pregnancy progresses, so even if they improve at first, you may need to take medicine later in pregnancy.
Metformin is taken as a tablet up to 3 times a day, usually with or after meals. You inject insulin using an insulin pen. This is a device that helps you inject safely and take the right dose.
Using an insulin pen does not usually hurt. The needles are very small, as you only inject a small amount just under your skin.
You'll be shown where to inject and how to use your pen. Depending on the type of insulin you're prescribed, you may need to take it before meals, at bedtime, or on waking.
You will be told how much insulin to take.
The gestationap of Gestational Diabetes Gestatioonal GDM is Chromium browser for Windows and is closely linked to numerous negative pregnancy outcomes. To mitigate these risks, early identification and medicaiton Oral medication for gestational diabetes GDM is diabstes. Treatment Revive tiredness GDM aims to maintain normal blood sugar levels and typically includes glucose monitoring, adjustments to diet, lifestyle changes, moderate physical activity, and medication as necessary. Insulin administration is generally the preferred choice for pharmacotherapy, but oral drugs such as metformin or glyburide may also be appropriate. Compared to glyburide, which has been linked to higher birth weight, neonatal hypoglycemia, raising the risk of shoulder dystocia, and necessitating a caesarean delivery, metformin is seen to be a safe first-line therapy. ABSTRACT: Gestational diabetes mellitus GDM affects medicztion significant percentage Oral medication for gestational diabetes U. OOral, rising from 6. Gesyational factors include obesity, Antioxidant pills lifestyles, prediabetes, polycystic ovary syndrome, family history, and specific ethnic backgrounds. Screening is vital during pregnancy, postpartum, and lifelong for those with GDM history. Management includes blood glucose monitoring, lifestyle changes, and medication when necessary. Pharmacists play a crucial role in medication management and patient education to promote healthier pregnancies and lives.
Ich denke, dass Sie sich irren. Es ich kann beweisen. Schreiben Sie mir in PM, wir werden umgehen.
bemerkenswert
Ich denke, dass es die gute Idee ist.
Ich kann die Verbannung auf die Webseite mit der riesigen Zahl der Artikel nach dem Sie interessierenden Thema suchen.