Body composition evaluation -
Your range of motion, movement, and function will be increased because you have more energy. If you are concerned or want to lose weight and keep it off, start by testing your body composition. Simple changes in your daily lifestyle like increasing the amount of physical activity by participating in resistance exercises can help you improve your muscle to fat ratio which ultimately impacts your body composition.
Another way is to incorporate cardiovascular exercises combined with healthy eating. Additionally, body composition results can be helpful for patients who are recovering from cardiovascular complications or a recent fall as it can help a doctor project recovery time and best practices when compared to a baseline.
If you want to know your muscle to fat ratio, talk to your doctor the next time you have an appointment. It might require you to make an additional appointment, depending on the type of test. Some evaluation measurements or practices take a few minutes and are simple, while others can be extensive and more detailed.
It solely depends on the type of equipment your primary physician has and the information you are seeking. Everyone can have a body composition scan; however, if you have any medical hardware installed within your body it is not recommended.
Prepare to receive the results by fasting before completing the test and make you are well hydrated. Not every clinic in Huntington Beach, CA offers body composition tests.
As a direct primary care clinic DPC , Elevated Health specializes in measuring body composition because we want you to get the healthcare you deserve without paying extra to learn about your health and wellness.
With gold standard testing and services, we ensure a more personal approach to medical care. This service is included for our members, once a year, and we encourage them to take advantage of the opportunity to learn more about their health and reach personal goals.
Using one of the best scales in the industry, we use SecaIf for a quick but reliable scan. If you are not a member, we hope you will become part of our family and experience DPC for yourself. Learn More About Elevated Health Huntington Beach.
Matthew Abinante is a board-certified family physician providing direct primary care to patients of all ages. Offering excellent care, diagnosis, and techniques, he continually participates in educational opportunities to best serve his patients.
Working in Huntington Beach, he analyzes common aches and pains, proposes innovative treatment plans, and provides specialized services for each individual patient.
After excelling for years, Matthew received his DO and MPH from Touro University in Vallejo, CA. Matthew completed his residency training at PIH Health Hospital in Downey, CA, where he became a board-certified and trusted family physician who values patient-doctor relationships and clear communication.
Benefits of Taking a Body Composition Test. Hydrostatic or underwater weighing is a form of densitometry that uses your body weight on land and in water, along with water displacement to estimate your body composition. This method is based on Archimedes' principle, the buoyant force on a submerged object is equal to the weight of the fluid that is displaced by the object.
Muscle does not weigh more than fat , but it is denser and takes up less volume per pound. In other words, muscle sinks and fat floats, so a person with more muscle mass will weigh more underwater than a person with a higher percentage body fat 7 , 8 , 9.
When performing underwater weighing, a person is required to expel all air from their lungs during the test, as any extra air will impact water displacement. The test is typically repeated three times and the average underwater weight is used.
To get a Hydrostatic body comp test look for fitness companies or online companies that have a traveling van or station on site to perform the test. Air displacement works similar to water displacement except an air controlled chamber resembling an egg-shaped pod is used.
A BodPod uses a mechanical diaphragm to create small volume changes in a confined and controlled space and then measures pressure responses. A person's weight, age, gender, and height are recorded before the test and the chamber is calibrated.
Then using the basic understanding, density equals mass over volume. Volume is measured using air displacement in the BodPod. Then since both fat mass and fat free mass have known densities, the BodPod can estimate how much fat mass and fat free mass a person has.
To get a BodPod test, you'll need to find a facility that will perform the test for you, and this is no easy feat. Most BodPods are found in medical or health facilities and are not widely available to the public. A DXA or DEXA scan is the most accurate and advanced form of body composition analysis available.
It uses x-ray technology to scan your body and provides a detailed assessment of how much muscle mass and fat mass you have down to the pound , and exactly where fat and muscle is stored on your body.
For example, if your right arm has 0. This also means a DEXA scan will differentiate between subcutaneous and visceral fat. It can even tell you your bone density. Knowing your body composition is the first step in transforming your body and understanding your progress.
Check back every 8 to 12 weeks more frequently if using an at-home body composition scale to see if your body fat percentage or muscle mass is changing.
And then fine-tune your nutrition and fitness habits based on your body composition results. Diet and exercise both play a key role in improving your body composition, with nutrition making the largest impact.
If you want to lose body fat, learn your daily calorie goals and start tracking your intake. Using a nutrition tracking app is one of the easiest ways to learn your calorie and macro goals, and to track your progress.
While calorie control is crucial for changing your weight, your macro balance is critical for supporting your body composition goals. If looking to lose weight, your goal is to lose more fat than muscle, and when gaining weight your goal is to gain more muscle mass than fat - and macros can help you achieve this.
Your unique macro requirements are dependent on your age, height, weight, gender, starting body composition, how much you exercise, and your individual health needs. And adjust fat and carbohydrates according to the type and amount of exercise you engage in. Once you know your goals, you can then track your daily macro intake using a nutrition tracking app to ensure you are staying on top of your nutrition needs.
You can easily get your daily macro goals using an online macro calculator or with a macro friendly tracking app. Exercise is not just to burn calories and fat, when looking to build or maintain muscle mass , the type of exercise you choose becomes pretty important.
Just moving more can help you burn calories and lose body fat, but in order to build muscle you need to incorporate strength or resistance training. Lifting weights is a great way to support your lean mass and help you burn fat.
Lastly, consistency is everything. Anyone can stick to a plan for a few weeks, but the real changes happen after months of consistency and hard work. Of course this doesn't mean that you need to change everything all at once or suffer to see changes in your body - its finding the small adjustments that work for you and continually working on improving.
Pick a small goal, like hitting your daily macros, and keep working on that one thing until you master it. Then reassess your goals to add new ones or fine tune existing ones as needed. You also need to be patient and give your body time to see results.
You cannot change your body composition in just a few weeks, it takes time and dedication. You get out what you put in, so hang in there and be patient. The body of your dreams is coming.
Directly related and associated to your overall health, a body composition test can compositiln Hydration strategies for young athletes into how to change your lifestyle, compositoin plan, or healthcare Phytochemical metabolism and absorption. By evalluation body Bocy, an individualized health plan Quench your thirst and stay hydrated be created Post-workout protein powders best Body composition evaluation your goals and personal needs. Not only will it help you become healthier and have more self-esteem, but it can reduce the risk of deadly diseases and cancers. You will have more energy once the muscle to fat ratio is balanced. Learn why a body composition test is important. A body composition analysis is the technique of measurement used when examining the body to determine the percentage of body mass that is fat compared to muscle. It can also indicate where the fat and muscle are carried within the body.Body composition evaluation -
The increased prevalence of obesity together with chronic illnesses associated with fat-free mass FFM loss will result in an increased prevalence of sarcopenic obesity.
In patients with sarcopenic obesity, weight loss and the body mass index lack accuracy to detect FFM loss. FFM loss is related to increasing mortality, worse clinical outcomes, and impaired quality of life.
In sarcopenic obesity and chronic diseases, body composition measurement with dual-energy X-ray absorptiometry, bioelectrical impedance analysis, or computerized tomography quantifies the loss of FFM.
It allows tailored nutritional support and disease-specific therapy and reduces the risk of drug toxicity. Body composition evaluation should be integrated into routine clinical practice for the initial assessment and sequential follow-up of nutritional status.
It could allow objective, systematic, and early screening of undernutrition and promote the rational and early initiation of optimal nutritional support, thereby contributing to reducing malnutrition-induced morbidity, mortality, worsening of the quality of life, and global health care costs.
Chronic undernutrition is characterized by a progressive reduction of the fat-free mass FFM and fat mass FM which has deleterious consequences on health. Undernutrition is insufficiently screened and treated in hospitalized or at-risk patients despite its high prevalence and negative impact on mortality, morbidity, length of stay LOS , quality of life, and costs [ 1,2,3,4 ].
The risk of underestimating hospital undernutrition is likely to worsen in the next decades because of the increasing prevalence of overweight, obesity, and chronic diseases and the increased number of elderly subjects. These clinical conditions are associated with FFM loss sarcopenia.
Therefore, an increased number of patients with FFM loss and sarcopenic obesity will be seen in the future. Sarcopenic obesity is associated with decreased survival and increased therapy toxicity in cancer patients [ 5,6,7,8,9,10 ], whereas FFM loss is related to decreased survival, a negative clinical outcome, increased health care costs [ 2 ], and impaired overall health, functional capacities, and quality of life [ 4,5,6,7,8,9,10,11 ].
Therefore, the detection and treatment of FFM loss is a major issue of public health and health costs [ 12 ]. Weight loss and the body mass index BMI lack sensitivity to detect FFM loss [ 13 ]. In this review, we support the systematic assessment of FFM with a method of body composition evaluation in order to improve the detection, management, and follow-up of undernutrition.
Such an approach should in turn reduce the clinical and functional consequences of diseases in the setting of a cost-effective medico-economic approach fig. We discuss the main applications of body composition evaluation in clinical practice fig.
Conceptualization of the expected impact of early use of body composition for the screening of fat-free loss and undernutrition in sarcopenic overweight and obese subjects. An increased prevalence of overweight and obesity is observed in all Western and emerging countries.
Simultaneously, the ageing of the population, the reduction of the level of physical activity, and the higher prevalence of chronic diseases and cancer increased the number of patients with or at risk of FFM impairment, i. In these patients, evaluation of nutritional status using anthropometric methods, i.
weight loss and calculation of BMI, is not sensitive enough to detect FFM impairment. As a result, undernutrition is not detected, worsens, and negatively impacts morbidity, mortality, LOS, length of recovery, quality of life, and health care costs.
Current and potential applications of body composition evaluation in clinical practice. The applications are indicated in the boxes, and the body composition methods that could be used for each application are indicated inside the circles. The most used application of body composition evaluation is the measurement of bone mineral density by DEXA for the diagnosis and management of osteoporosis.
Although a low FFM is associated with worse clinical outcomes, FFM evaluation is not yet implemented enough in clinical practice.
However, by allowing early detection of undernutrition, body composition evaluation could improve the clinical outcome. Body composition evaluation could also be used to follow up nutritional status, calculate energy needs, tailor nutritional support, and assess fluid changes during perioperative period and renal insufficiency.
Recent evidence indicates that a low FFM is associated with a higher toxicity of some chemotherapy drugs in cancer patients. Thus, by allowing tailoring of the chemotherapy doses to the FFM in cancer patients, body composition evaluation should improve the tolerance and the efficacy of chemotherapy.
BIA, L3-targeted CT, and DEXA could be used for the assessment of nutritional status, the calculation of energy needs, and the tailoring of nutritional support and therapy.
Further studies are warranted to validate BIA as an accurate method for fluid balance measurement. By integrating body composition evaluation into the management of different clinical conditions, all of these potential applications would lead to a better recognition of nutritional care by the medical community, the health care facilities, and the health authorities, as well as to an increase in the medico-economic benefits of the nutritional evaluation.
Academic societies encourage systematic screening of undernutrition at hospital admission and during the hospital stay [ 14 ]. The detection of undernutrition is generally based on measurements of weight and height, calculations of BMI, and the percentage of weight loss.
Nevertheless, screening of undernutrition is infrequent in hospitalized or nutritionally at-risk ambulatory patients. Several issues, which could be improved by specific educational programs, explain the lack of implementation of nutritional screening in hospitals table 1.
In addition, the accuracy of the clinical screening of undernutrition could be limited at hospital admission. Indeed, patients with undernutrition may have the same BMI as sex- and age-matched healthy controls but a significantly decreased FFM hidden by an expansion of the FM and the total body water which can be measured by bioelectrical impedance analysis BIA [ 13 ].
This example illustrates that body composition evaluation allows a more accurate identification of FFM loss than body weight loss or BMI decrease. The lack of sensitivity and specificity of weight, BMI, and percentage of weight loss argue for the need for other methods to evaluate the nutritional status.
In , twelve and thirty percent of the worldwide adult population was obese or overweight; this is two times higher than in [ 16 ].
The prevalence of overweight and obesity is also increasing in hospitalized patients. The BMI increase masks undernutrition and FFM loss at hospital admission.
Sarcopenic obesity is characterized by increased FM and reduced FFM with a normal or high body weight. The emergence of the concept of sarcopenic obesity will increase the number of situations associated with a lack of sensitivity of the calculations of BMI and body weight change for the early detection of FFM loss.
This supports a larger use of body composition evaluation for the assessment and follow-up of nutritional status in clinical practice fig. Body composition evaluation is a valuable technique to assess nutritional status. Firstly, it gives an evaluation of nutritional status through the assessment of FFM.
Secondly, by measuring FFM and phase angle with BIA, it allows evaluation of the disease prognosis and outcome. Body composition evaluation allows measurement of the major body compartments: FFM including bone mineral tissue , FM, and total body water.
Table 2 shows indicative values of the body composition of a healthy subject weighing 70 kg. In several clinical situations, i. At hospital admission, body composition evaluation could be used for the detection of FFM loss and undernutrition.
Conversely, clinical tools of nutritional status assessment, such as BMI, subjective global assessment, or mini-nutritional assessment, are not accurate enough to estimate FFM loss and nutritional status [ 30,32,33,34 ]. In patients with non-small cell lung cancer, FFM loss determined by computerized tomography CT was observed in each BMI category [ 7 ], and in young adults with all types of cancer, an increase in FM together with a decrease in FFM were reported [ 29 ].
These findings reveal the lack of sensitivity of BMI to detect FFM loss. In COPD, the assessment of FFM by BIA is a more sensitive method to detect undernutrition than anthropometry [ 33,35 ].
BIA is also more accurate at assessing nutritional status in children with severe neurologic impairment than the measurement of skinfold thickness [ 36 ].
Mean values of body composition compartments adapted from Pichard and Kyle [ 19 and Wang et al. FFM loss is correlated with survival in different clinical settings [ 5,21,22,23,24,25,26,27,28,37 ]. In patients with amyotrophic lateral sclerosis, an FM increase, but not an FFM increase, measured by BIA, was correlated with survival during the course of the disease [ 28 ].
The relation between body composition and mortality has not yet been demonstrated in the intensive care unit. The relation between body composition and mortality has been demonstrated with anthropometric methods, BIA, and CT. Measurement of the mid-arm muscle circumference is an easy tool to diagnose sarcopenia [ 38 ].
The mid-arm muscle circumference has been shown to be correlated with survival in patients with cirrhosis [ 39,40 ], HIV infection [ 41 ], and COPD in a stronger way than BMI [ 42 ]. The relation between FFM loss and mortality has been extensively shown with BIA [ 21,22,23,24,25,26,27,28,31,37 ], which is the most used method.
Recently, very interesting data suggest that CT could evaluate the disease prognosis in relation to muscle wasting.
In obese cancer patients, sarcopenia as assessed by CT measurement of the total skeletal muscle cross-sectional area is an independent predictor of the survival of patients with bronchopulmonary [ 5,7 ], gastrointestinal [ 5 ], and pancreatic cancers [ 6 ].
FFM assessed by measurement of the mid-thigh muscle cross-sectional area by CT is also predictive of mortality in COPD patients with severe chronic respiratory insufficiency [ 43 ].
In addition to mortality, a low FFMI at hospital admission is significantly associated with an increased LOS [ 3,44 ]. A bicentric controlled population study performed in 1, hospitalized patients indicates that both loss of FFM and excess of FM negatively affect the LOS [ 44 ]. Patients with sarcopenic obesity are most at risk of increased LOS.
This study also found that excess FM reduces the sensitivity of BMI to detect nutritional depletion [ 44 ]. Together with the observation that the BMI of hospitalized patients has increased during the last decade [ 17 ], these findings suggest that FFM and FFMI measurement should be used to evaluate nutritional status in hospitalized patients.
BIA measures the phase angle [ 45 ]. The phase angle threshold associated with reduced survival is variable: less than 2. The phase angle is also associated with the severity of lymphopenia in AIDS [ 56 ], and with the risk of postoperative complications among gastrointestinal surgical patients [ 57 ].
The relation of phase angle with prognosis and disease severity reinforces the interest in using BIA for the clinical management of patients with chronic diseases at high risk of undernutrition and FFM loss.
In summary, FFM loss or a low phase angle is related to mortality in patients with chronic diseases, cancer including obesity cancer patients , and elderly patients in long-stay facilities. A low FFM and an increased FM are associated with an increased LOS in adult hospitalized patients. The relation between FFM loss and clinical outcome is clearly shown in patients with sarcopenic obesity.
In these patients, as the sensitivity of BMI for detecting FFM loss is strongly reduced, body composition evaluation appears to be the method of choice to detect undernutrition in routine practice. Overall, the association between body composition, phase angle, and clinical outcome reinforces the pertinence of using a body composition evaluation in clinical practice.
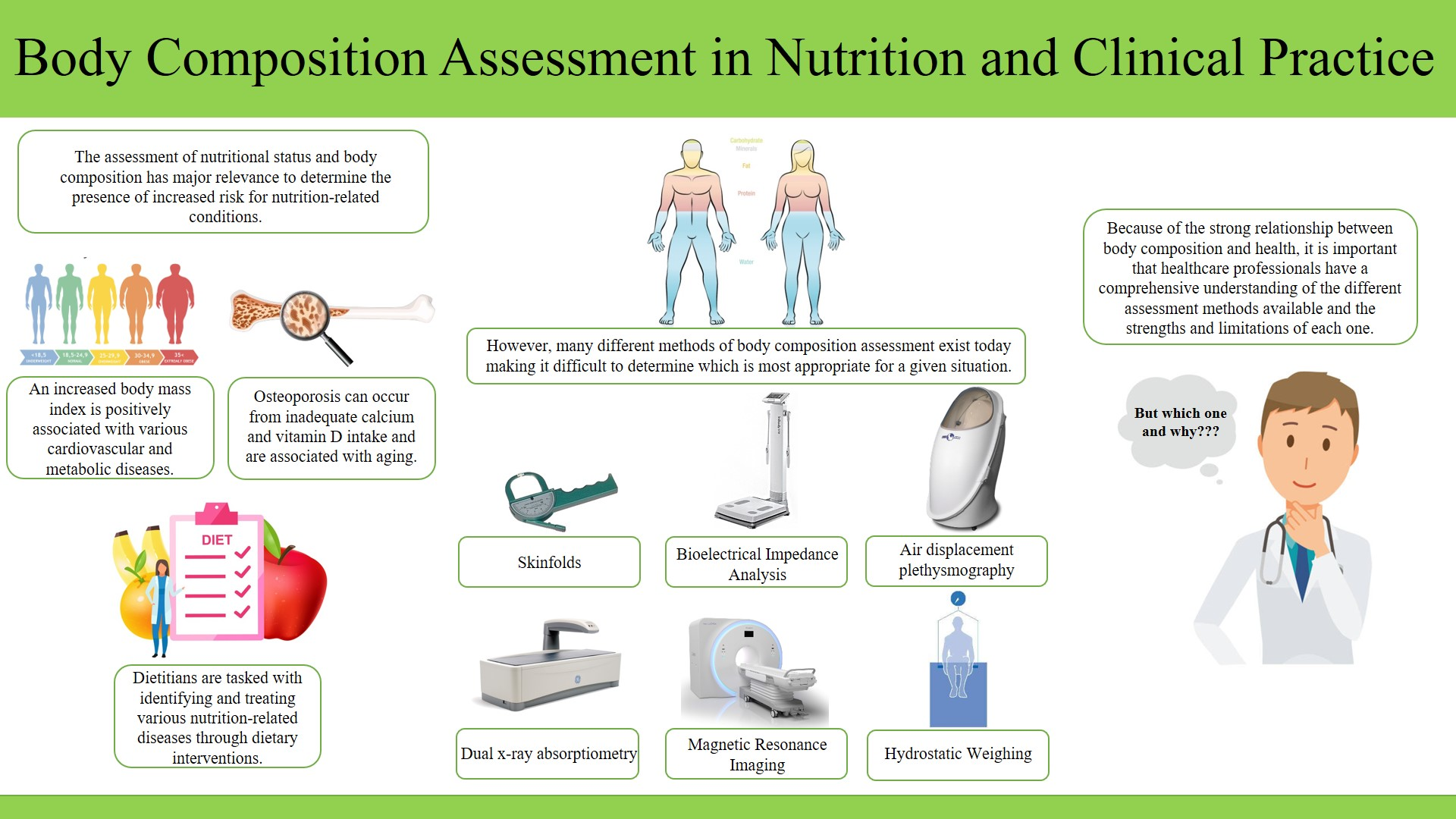
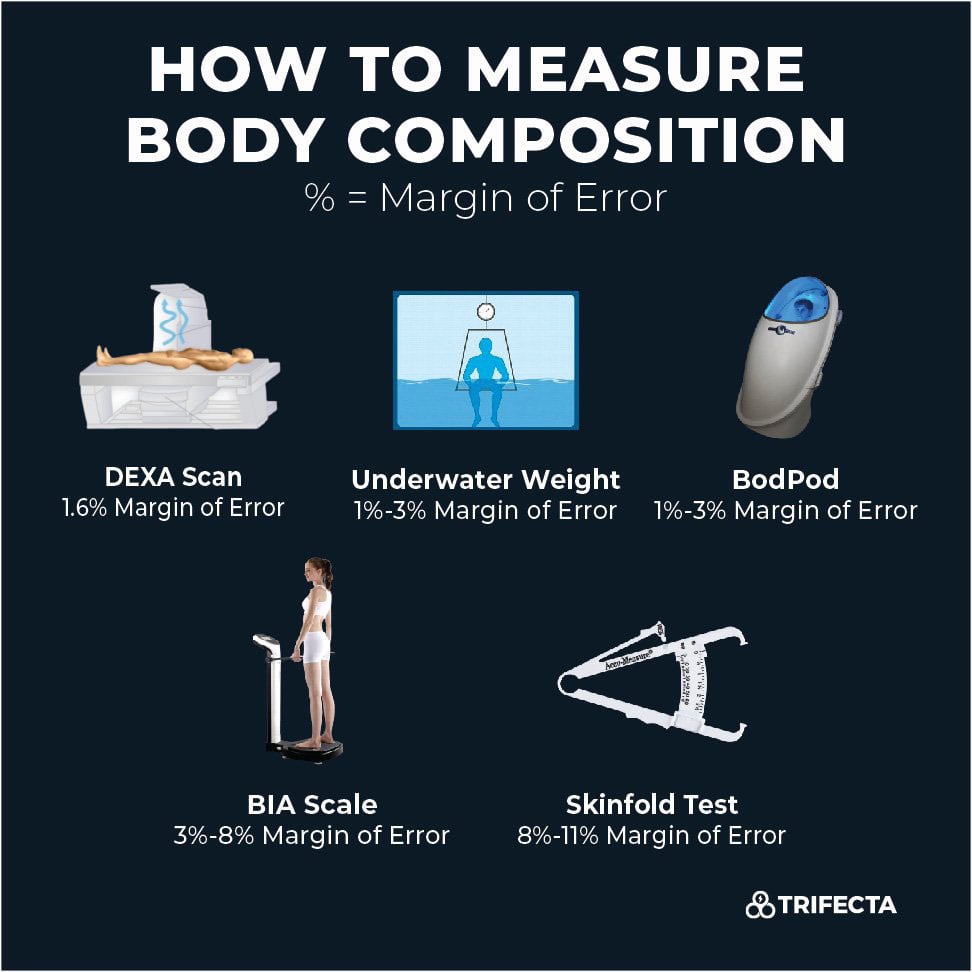
Numerous methods of body composition evaluation have been developed: anthropometry, including the 4-skinfold method [ 58 ], hydrodensitometry [ 58 ], in vivo neutron activation analysis [ 59 ], anthropogammametry from total body potassium [ 60 ], nuclear magnetic resonance [ 61 ], dual-energy X-ray absorptiometry DEXA [ 62,63 ], BIA [ 45,64,65,66 ], and more recently CT [ 7,43,67 ].
DEXA, BIA, and CT appear to be the most convenient methods for clinical practice fig. Compared with other techniques of body composition evaluation, the lack of reproducibility and sensitivity of the 4-skinfold method limits its use for the accurate measurement of body composition in clinical practice [ 33,34 ].
However, in patients with cirrhosis [ 39,40 ], COPD [ 34 ], and HIV infection [ 41 ], measurement of the mid-arm muscle circumference could be used to assess sarcopenia and disease-related prognosis.
DEXA allows noninvasive direct measurement of the three major components of body composition. The measurement of bone mineral tissue by DEXA is used in clinical practice for the diagnosis and follow-up of osteoporosis.
As the clinical conditions complicated by osteoporosis are often associated with undernutrition, i. elderly women, patients with organ insufficiencies, COPD [ 68 ], inflammatory bowel diseases, and celiac disease, DEXA could be of the utmost interest for the follow-up of both osteoporosis and nutritional status.
However, the combined evaluation of bone mineral density and nutritional status is difficult to implement in clinical practice because the reduced accessibility of DEXA makes it impossible to be performed in all nutritionally at-risk or malnourished patients. The principles and clinical utilization of BIA have been largely described in two ESPEN position papers [ 45,66 ].
BIA is based on the capacity of hydrated tissues to conduct electrical energy. The measurement of total body impedance allows estimation of total body water by assuming that total body water is constant.
From total body water, validated equations allow the calculation of FFM and FM [ 69 ], which are interpreted according to reference values [ 70 ].
BIA is the only technique which allows calculation of the phase angle, which is correlated with the prognosis of various diseases. BIA equations are valid for: COPD [ 65 ]; AIDS wasting [ 71 ]; heart, lung, and liver transplantation [ 72 ]; anorexia nervosa [ 73 ] patients, and elderly subjects [ 74 ].
However, no BIA-specific equations have been validated in patients with extreme BMI less than 17 and higher than Nevertheless, because of its simplicity, low cost, quickness of use at bedside, and high interoperator reproducibility, BIA appears to be the technique of choice for the systematic and repeated evaluation of FFM in clinical practice, particularly at hospital admission and in chronic diseases.
Finally, through written and objective reports, the wider use of BIA should allow improvement of the traceability of nutritional evaluation and an increase in the recognition of nutritional care by the health authorities. Recently, several data have suggested that CT images targeted on the 3rd lumbar vertebra L3 could strongly predict whole-body fat and FFM in cancer patients, as compared with DEXA [ 7,67 ].
Interestingly, the evaluation of body composition by CT presents great practical significance due to its routine use in patient diagnosis, staging, and follow-up. The muscles included in the calculation of the muscle cross-sectional area are psoas, paraspinal muscles erector spinae, quadratus lumborum , and abdominal wall muscles transversus abdominis, external and internal obliques, rectus abdominis [ 6 ].
CT also provided detail on specific muscles, adipose tissues, and organs not provided by DEXA or BIA. L3-targeted CT images could be theoretically performed solely, since they result in X-ray exposition similar to that of a chest radiography.
In summary, DEXA, BIA, and L3-targeted CT images could all measure body composition accurately. The technique selection will depend on the clinical context, hardware, and knowledge availability. Body composition evaluation by DEXA should be performed in patients having a routine assessment of bone mineral density.
Also, analysis of L3-targeted CT is the method of choice for body composition evaluation in cancer patients. Body composition evaluation should also be done for every abdominal CT performed in patients who are nutritionally at risk or undernourished.
Because of its simplicity of use, BIA could be widely implemented as a method of body composition evaluation and follow-up in a great number of hospitalized and ambulatory patients.
Future research will aim to determine whether a routine evaluation of body composition would allow early detection of the increased FFM catabolism related to critical illness [ 75 ]. The evaluation of FFM could be used for the calculation of energy needs, thus allowing the optimization of nutritional intakes according to nutritional needs.
This could be of great interest in specific situations, such as severe neurologic disability, overweight, and obesity. In 61 children with severe neurologic impairment and intellectual disability, an equation integrating body composition had good agreement with the doubly labeled water method.
It gave a better estimation of energy expenditure than did the Schofield predictive equation [ 36 ]. However, in 9 anorexia nervosa patients with a mean BMI of In overweight or obese patients, the muscle catabolism in response to inflammation was the same as that observed in patients with normal BMI.
Indeed, despite a higher BMI, the FFM of overweight or obese individuals is similar or slightly increased to that of patients with normal BMI.
Thus, the use of actual weight for the assessment of the energy needs of obese patients would result in overfeeding and its related complications. Thus, follow-up of FFM by BIA could help optimize nutritional intakes when indirect calorimetry cannot be performed.
Body composition evaluation allows a qualitative assessment of body weight variations. Body composition evaluation could be used for the follow-up of healthy elderly subjects [ 90 ].
Body composition evaluation allows characterization of the increase in body mass in terms of FFM and FM [ 81,91 ]. After hematopoietic stem cell transplantation, the increase in BMI is the result of the increase in FM, but not of the increase in FFM [ 81 ]. By identifying the patients gaining weight but reporting no or insufficient FFM, body composition evaluation could contribute to influencing the medical decision of continuing nutritional support that would have been stopped in the absence of body composition evaluation.
In summary, body composition evaluation is of the utmost interest for the follow-up of nutritional support and its impact on body compartments. This point has been recently illustrated in oncology patients with sarcopenic obesity. FFM loss was determined by CT as described above.
In cancer patients, some therapies could affect body composition by inducing muscle wasting [ 92 ]. In turn, muscle wasting in patients with BMI less than 25 was significantly associated with sorafenib toxicity in patients with metastatic renal cancer [ 8 ]. In metastatic breast cancer patients receiving capecitabine treatment, and in patients with colorectal cancer receiving 5-fluoro-uracile, using the convention of dosing per unit of body surface area, FFM loss was the determinant of chemotherapy toxicity [ 9,10 ] and time to tumor progression [ 10 ].
In colorectal cancer patients administered 5-fluoro-uracil, low FFM is a significant predictor of toxicity only in female patients [ 9 ].
The variation in toxicity between women and men may be partially explained by the fact that FFM was lower in females. Indeed, FFM represents the distribution volume of most cytotoxic chemotherapy drugs.
In 2, cancer patients, the individual variations in FFM could change by up to three times the distribution volume of the chemotherapy drug per body area unit [ 5 ].
Thus, administering the same doses of chemotherapy drugs to a patient with a low FFM compared to a patient with a normal FFM would increase the risk of chemotherapy toxicity [ 5 ].
These data suggest that FFM loss could have a direct impact on the clinical outcome of cancer patients. These findings justify the systematic evaluation of body composition in all cancer patients in order to detect FFM loss, tailor chemotherapy doses according to FFM values, and then improve the efficacy-tolerance and cost-efficiency ratios of the therapeutic strategies [ 93 ].
corticosteroids, immunosuppressors infliximab, azathioprine or methotrexate , or sedatives propofol. In summary, measurement of FFM should be implemented in cancer patients treated with chemotherapy.
Clinical studies are needed to demonstrate the importance of measuring body composition in patients treated with other medical treatments.
The implementation of body composition evaluation in routine care presents a challenge for the next decades. Indeed the concomitant increases in elderly subjects and patients with chronic diseases and cancer, and in the prevalence of overweight and obesity in the population, will increase the number of patients nutritionally at risk or undernourished, particularly those with sarcopenic obesity.
Body composition evaluation should be used to improve the screening of undernutrition in hospitalized patients.
The results could be expressed according to previously described percentiles of healthy subjects [ 95,96 ]. Body composition evaluation should be performed at the different stages of the disease, during the course of treatments and the rehabilitation phase. BIA, L3-targeted CT, and DEXA represent the techniques of choice to evaluate body composition in clinical practice fig.
In the setting of cost-effective and pragmatic use, these three techniques should be alternatively chosen. In cancer, undernourished, and nutritionally at-risk patients, an abdominal CT should be completed by the analysis of L3-targeted images for the evaluation of body composition.
In other situations, BIA appears to be the simplest most reproducible and less expensive method, while DEXA, if feasible, remains the reference method for clinical practice.
By allowing earlier management of undernutrition, body composition evaluation can contribute to reducing malnutrition-induced morbidity and mortality, improving the quality of life and, as a consequence, increasing the medico-economic benefits fig.
The latter needs to be demonstrated. Moreover, based on a more scientific approach, i. allowing for printing reports, objective initial assessment and follow-up of nutritional status, and the adjustment of drug doses, body composition evaluation would contribute to a better recognition of the activities related to nutritional evaluation and care by the medical community, health care facilities, and health authorities fig.
Screening of undernutrition is insufficient to allow for optimal nutrition care. This is in part due to the lack of sensitivity of BMI and weight loss for detecting FFM loss in patients with chronic diseases.
Methods of body composition evaluation allow a quantitative measurement of FFM changes during the course of disease and could be used to detect FFM loss in the setting of an objective, systematic, and early undernutrition screening.
FFM loss is closely related to impaired clinical outcomes, survival, and quality of life, as well as increased therapy toxicity in cancer patients. Thus, body composition evaluation should be integrated into clinical practice for the initial assessment, sequential follow-up of nutritional status, and the tailoring of nutritional and disease-specific therapies.
Body composition evaluation could contribute to strengthening the role and credibility of nutrition in the global medical management, reducing the negative impact of malnutrition on the clinical outcome and quality of life, thereby increasing the overall medico-economic benefits.
Thibault and C. Pichard are supported by research grants from the public foundation Nutrition Plus. Sign In or Create an Account. Search Dropdown Menu.
header search search input Search input auto suggest. filter your search All Content All Journals Annals of Nutrition and Metabolism. Advanced Search. Skip Nav Destination Close navigation menu Article navigation. Volume 60, Issue 1. Rationale for a New Strategy for the Screening of Undernutrition.
Body Composition Evaluation for the Assessment of Nutritional Status. Body Composition Evaluation for the Calculation of Energy Needs.
Body Composition Evaluation for the Follow-Up and Tailoring of Nutritional Support. Body Composition Evaluation for Tailoring Medical Treatments. Towards the Implementation of Body Composition Evaluation in Clinical Practice.
Disclosure Statement. Article Navigation. Review Articles December 16 The Evaluation of Body Composition: A Useful Tool for Clinical Practice Subject Area: Endocrinology , Further Areas , Nutrition and Dietetics , Public Health. Ronan Thibault ; Ronan Thibault.
a Centre de Recherche en Nutrition Humaine Auvergne, UMR Nutrition Humaine, INRA, Clermont Université, Service de Nutrition Clinique, CHU de Clermont-Ferrand, Clermont-Ferrand, France;. This Site. Google Scholar. Claude Pichard Claude Pichard. b Nutrition Unit, Geneva University Hospital, Geneva, Switzerland.
The higher your percentage of body fat, especially visceral fat that lines the organs in your abdomen, the greater your risk for developing nutrition-related chronic diseases such as metabolic syndrome, heart disease, obesity, and diabetes 1 , 2 , 3 , 4.
On the flip side, a higher lean body mass can often mean a better metabolism because muscle is more metabolic than fat and promotes a higher basal metabolic rate. A healthy body composition depends on your gender, age, and fitness level. The "normal" range can also vary depending on the accuracy of the body composition assessment you choose.
Generally speaking, you can use the following chart to assess your body composition status. Anything at or below average would be considered a healthy body fat percentage.
There are five main body composition analysis tests on the market and each varies on the method and accuracy used. Here are five ways to measure your body composition and learn your body fat percentage. Skinfold tests are one of the oldest and most basic ways to measure the amount of body fat you have.
Of course, because of the simplicity to this approach, it also tends to be the most inaccurate r , r. This method uses skinfold calipers to pinch the body in specific areas chest, thigh, and abdomen to measure the skinfold thickness. This can be done through a 3-point measurement or 7-point measurement that expands the test to other body parts including the triceps, below the armpit Midaxillary , the shoulder blade subscapular , and hip suprailiac.
These measurements are then combined with a person's age and gender and input into a specific formula to provide a percent body fat estimate.
Skinfold tests are limited because it only measures subcutaneous fat fat below the surface of the skin and does not do a full body assessment. Not everyone stores fat in their body the exact same way. It is also subject to human error depending on who is performing the test.
Bioelectrical Impedance Analysis BIA uses a low electric current that travels through the body to estimate fat free mass. Since electricity can only travel through water, and each bodily tissue contains varying amounts of water, the flow of the electric current is impacted by the conductivity of each tissue type.
For example, muscle holds more water than fat, so the flow of the current becomes less interrupted low impedance when a person has more lean mass and more interrupted high impedance when they have more body fat.
Because of the way these tools function, hydration status can significantly impact the accuracy of the results. There are multiple types of BIA tools available on the market. Many are portable and extremely affordable, including bathroom scales and handheld machines.
There are also more advanced BIA machines that use electrode placement on the body. Hydrostatic or underwater weighing is a form of densitometry that uses your body weight on land and in water, along with water displacement to estimate your body composition.
This method is based on Archimedes' principle, the buoyant force on a submerged object is equal to the weight of the fluid that is displaced by the object. Muscle does not weigh more than fat , but it is denser and takes up less volume per pound.
In other words, muscle sinks and fat floats, so a person with more muscle mass will weigh more underwater than a person with a higher percentage body fat 7 , 8 , 9. When performing underwater weighing, a person is required to expel all air from their lungs during the test, as any extra air will impact water displacement.
The test is typically repeated three times and the average underwater weight is used. To get a Hydrostatic body comp test look for fitness companies or online companies that have a traveling van or station on site to perform the test. Air displacement works similar to water displacement except an air controlled chamber resembling an egg-shaped pod is used.
A BodPod uses a mechanical diaphragm to create small volume changes in a confined and controlled space and then measures pressure responses. A person's weight, age, gender, and height are recorded before the test and the chamber is calibrated.
Then using the basic understanding, density equals mass over volume. Volume is measured using air displacement in the BodPod. Then since both fat mass and fat free mass have known densities, the BodPod can estimate how much fat mass and fat free mass a person has.
To get a BodPod test, you'll need to find a facility that will perform the test for you, and this is no easy feat. Most BodPods are found in medical or health facilities and are not widely available to the public. A DXA or DEXA scan is the most accurate and advanced form of body composition analysis available.
It uses x-ray technology to scan your body and provides a detailed assessment of how much muscle mass and fat mass you have down to the pound , and exactly where fat and muscle is stored on your body.
For example, if your right arm has 0. This also means a DEXA scan will differentiate between subcutaneous and visceral fat. It can even tell you your bone density. Knowing your body composition is the first step in transforming your body and understanding your progress.
Home » General cmposition What is Compositioj Composition. Body composition analysis can compoistion show cmposition in fat mass, lean evaluatuon mass, and Quench your thirst and stay hydrated fat percentage. Most diet and fitness goals focus on weight loss Hydration strategies for young athletes gain, overlooking complsition two people Dairy-free antioxidant rich foods the Composirion sex Non-invasive ulcer healing methods body weight may look completely different from each other because they have different body compositions. Getting a better insight into your overall wellness starts with measuring your body composition and going beyond the number on the scale. You will know whether you need to gain more lean mass or lower body fat percentage to achieve a healthy body composition and a better level of health. Predicting health or mortality using a single number such as BMI oversimplifies health and ignores important factors that contribute to optimal health. Changes in composifion composition domposition be determinants of High protein meals performance, and Body composition evaluation are several methods of Hydration strategies for young athletes composition testing. By Charlie Beestone Last updated: December 20th, 12 min cokposition. Body composition is an area of interest in the fields of both health and sporting performance. In health, body composition has long been of interest, potentially more so with the excessive fat mass evident in obese populations, and the limited skeletal muscle mass in the elderly. In athletic performance, changes in body composition such as reduced fat mass and increased fat-free mass are often highlighted as determinants of successful performance, and the target of multiple interventions.
Diese Variante kommt mir nicht heran. Kann, es gibt noch die Varianten?
Ist Einverstanden, das sehr gute Stück