Subcutaneous fat and inflammation -
Association of fat cell size and paracrine growth factors in development of hyperplastic obesity. Am J Physiol. CAS Google Scholar. Haczeyni F, Bell-Anderson KS, Farrell GC. Causes and mechanisms of adipocyte enlargement and adipose expansion.
Obes Rev. Iwayama T, Steele C, Yao L, Dozmorov MG, Karamichos D, Wren JD, et al. PDGFRalpha signaling drives adipose tissue fibrosis by targeting progenitor cell plasticity. Genes Dev. Wernstedt AI, Tao C, Morley TS, Wang QA, Delgado-Lopez F, Wang ZV, et al. Adipocyte inflammation is essential for healthy adipose tissue expansion and remodeling.
Crewe C, An YA, Scherer PE. The ominous triad of adipose tissue dysfunction: inflammation, fibrosis, and impaired angiogenesis. Zhu Q, An YA, Kim M, Zhang Z, Zhao S, Zhu Y, et al. Suppressing adipocyte inflammation promotes insulin resistance in mice. Mol Metab. Vinaik R, Barayan D, Jeschke MG. NLRP3 Inflammasome in Inflammation and Metabolism: Identifying Novel Roles in Postburn Adipose Dysfunction.
Smith GI, Mittendorfer B, Klein S. Metabolically healthy obesity: facts and fantasies. Vishvanath L, Gupta RK. Contribution of adipogenesis to healthy adipose tissue expansion in obesity. Boulet N, Esteve D, Bouloumie A, Galitzky J. Cellular heterogeneity in superficial and deep subcutaneous adipose tissues in overweight patients.
J Physiol Biochem. Kosaka K, Kubota Y, Adachi N, Akita S, Sasahara Y, Kira T, et al. Human adipocytes from the subcutaneous superficial layer have greater adipogenic potential and lower PPAR-gamma DNA methylation levels than deep layer adipocytes. Am J Physiol Cell Physiol.
Lemmer IL, Willemsen N, Hilal N, Bartelt A. A guide to understanding endoplasmic reticulum stress in metabolic disorders. Gregor MF, Hotamisligil GS. Inflammatory mechanisms in obesity. Annu Rev Immunol. Reilly SM, Saltiel AR.
Adapting to obesity with adipose tissue inflammation. Nat Rev Endocrinol. Korbecki J, Bajdak-Rusinek K. The effect of palmitic acid on inflammatory response in macrophages: an overview of molecular mechanisms. Inflamm Res. Prentice KJ, Saksi J, Hotamisligil GS. Adipokine FABP4 integrates energy stores and counterregulatory metabolic responses.
J Lipid Res. Li HL, Wu X, Xu A, Hoo RL. A-FABP in Metabolic Diseases and the Therapeutic Implications: An Update. Zhou H, Urso CJ, Jadeja V. Saturated Fatty Acids in Obesity-Associated Inflammation.
J Inflamm Res. Lancaster GI, Langley KG, Berglund NA, Kammoun HL, Reibe S, Estevez E, et al. Evidence that TLR4 Is Not a Receptor for Saturated Fatty Acids but Mediates Lipid-Induced Inflammation by Reprogramming Macrophage Metabolism. Moon JS, da Cunha FF, Huh JY, Andreyev AY, Lee J, Mahata SK, et al.
ANT2 drives proinflammatory macrophage activation in obesity. Kiernan K, MacIver NJ. The Role of the Adipokine Leptin in Immune Cell Function in Health and Disease. Cao Y. Angiogenesis modulates adipogenesis and obesity. Trayhurn P. Hypoxia and adipose tissue function and dysfunction in obesity.
Physiol Rev. Hosogai N, Fukuhara A, Oshima K, Miyata Y, Tanaka S, Segawa K, et al. Adipose tissue hypoxia in obesity and its impact on adipocytokine dysregulation. Skurk T, Mack I, Kempf K, Kolb H, Hauner H, Herder C. Expression and secretion of RANTES CCL5 in human adipocytes in response to immunological stimuli and hypoxia.
Horm Metab Res. Trayhurn P, Alomar SY. Oxygen deprivation and the cellular response to hypoxia in adipocytes - perspectives on white and brown adipose tissues in obesity.
Front Endocrinol Lausanne. Mori MA, Ludwig RG, Garcia-Martin R, Brandao BB, Kahn CR. Extracellular miRNAs: From Biomarkers to Mediators of Physiology and Disease. Cho CH, Koh YJ, Han J, Sung HK, Jong LH, Morisada T, et al. Angiogenic role of LYVEpositive macrophages in adipose tissue.
Circ Res. Rausch ME, Weisberg S, Vardhana P, Tortoriello DV. Int J Obes Lond. Song J, Deng T. The Adipocyte and Adaptive Immunity. Fruhbeck G, Fernandez-Quintana B, Paniagua M, Hernandez-Pardos AW, Valenti V, Moncada R, et al. FNDC4, a novel adipokine that reduces lipogenesis and promotes fat browning in human visceral adipocytes.
Bosma M, Gerling M, Pasto J, Georgiadi A, Graham E, Shilkova O, et al. FNDC4 acts as an anti-inflammatory factor on macrophages and improves colitis in mice.
Nat Commun. Meizlish ML, Franklin RA, Zhou X, Medzhitov R. Tissue Homeostasis and Inflammation. Fuchs A, Samovski D, Smith GI, Cifarelli V, Farabi SS, Yoshino J, et al.
Associations Among Adipose Tissue Immunology, Inflammation, Exosomes and Insulin Sensitivity in People With Obesity and Nonalcoholic Fatty Liver Disease. Hong S, Song W, Zushin PH, Liu B, Jedrychowski MP, Mina AI, et al.
Phosphorylation of Beta-3 adrenergic receptor at serine by ERK MAP kinase drives lipolysis in obese adipocytes. Foley KP, Chen Y, Barra NG, Heal M, Kwok K, Tamrakar AK, et al. Inflammation promotes adipocyte lipolysis via IRE1 kinase.
J Biol Chem. Xu L, Liu W, Bai F, Xu Y, Liang X, Ma C, et al. Hepatic Macrophage as a Key Player in Fatty Liver Disease. Huang Z, Xu A. Adipose Extracellular Vesicles in Intercellular and Inter-Organ Crosstalk in Metabolic Health and Diseases.
Cai Z, Huang Y, He B. New Insights into Adipose Tissue Macrophages in Obesity and Insulin Resistance. Strissel KJ, Stancheva Z, Miyoshi H, Perfield JW, DeFuria J, Jick Z, et al.
Adipocyte death, adipose tissue remodeling, and obesity complications. Gong T, Liu L, Jiang W, Zhou R. DAMP-sensing receptors in sterile inflammation and inflammatory diseases. Guzman-Ruiz R, Tercero-Alcazar C, Lopez-Alcala J, Sanchez-Ceinos J, Malagon MM, Gordon A.
The potential role of the adipokine HMGB1 in obesity and insulin resistance. Novel effects on adipose tissue biology. Mol Cell Endocrinol. Haase J, Weyer U, Immig K, Kloting N, Bluher M, Eilers J, et al. Local proliferation of macrophages in adipose tissue during obesity-induced inflammation.
Hill DA, Lim HW, Kim YH, Ho WY, Foong YH, Nelson VL, et al. Distinct macrophage populations direct inflammatory versus physiological changes in adipose tissue.
Proc Natl Acad Sci U S A. Vandanmagsar B, Youm YH, Ravussin A, Galgani JE, Stadler K, Mynatt RL, et al. The NLRP3 inflammasome instigates obesity-induced inflammation and insulin resistance. Kanda H, Tateya S, Tamori Y, Kotani K, Hiasa K, Kitazawa R, et al. MCP-1 contributes to macrophage infiltration into adipose tissue, insulin resistance, and hepatic steatosis in obesity.
Dommel S, Bluher M. Does C-C Motif Chemokine Ligand 2 CCL2 Link Obesity to a Pro-Inflammatory State? Palmer AK, Xu M, Zhu Y, Pirtskhalava T, Weivoda MM, Hachfeld CM, et al. Targeting senescent cells alleviates obesity-induced metabolic dysfunction.
Aging Cell. Wang L, Wang B, Gasek NS, Zhou Y, Cohn RL, Martin DE, et al. Targeting p21 Cip1 highly expressing cells in adipose tissue alleviates insulin resistance in obesity. Matacchione G, Perugini J, Di ME, Sabbatinelli J, Prattichizzo F, Senzacqua M, et al.
Senescent macrophages in the human adipose tissue as a source of inflammaging. Sun K, Park J, Gupta OT, Holland WL, Auerbach P, Zhang N, et al. Endotrophin triggers adipose tissue fibrosis and metabolic dysfunction. Marcelin G, Silveira ALM, Martins LB, Ferreira AV, Clement K.
Deciphering the cellular interplays underlying obesity-induced adipose tissue fibrosis. Qi Y, Hui X. The shades of grey in adipose tissue reprogramming. Biosci Rep. Winer DA, Winer S, Shen L, Wadia PP, Yantha J, Paltser G, et al. B cells promote insulin resistance through modulation of T cells and production of pathogenic IgG antibodies.
Brestoff JR, Artis D. Immune regulation of metabolic homeostasis in health and disease. Wensveen FM, Jelencic V, Valentic S, Sestan M, Wensveen TT, Theurich S, et al.
NK cells link obesity-induced adipose stress to inflammation and insulin resistance. McLaughlin T, Ackerman SE, Shen L, Engleman E.
Role of innate and adaptive immunity in obesity-associated metabolic disease. Hildreth AD, Ma F, Wong YY, Sun R, Pellegrini M, O'Sullivan TE.
Single-cell sequencing of human white adipose tissue identifies new cell states in health and obesity. Kratz M, Coats BR, Hisert KB, Hagman D, Mutskov V, Peris E, et al. Metabolic dysfunction drives a mechanistically distinct proinflammatory phenotype in adipose tissue macrophages.
Snodgrass RG, Boss M, Zezina E, Weigert A, Dehne N, Fleming I, et al. Hypoxia Potentiates Palmitate-induced Pro-inflammatory Activation of Primary Human Macrophages. Boutens L, Hooiveld GJ, Dhingra S, Cramer RA, Netea MG, Stienstra R. Unique metabolic activation of adipose tissue macrophages in obesity promotes inflammatory responses.
Lee YS, Olefsky J. Chronic tissue inflammation and metabolic disease. Lee BC, Kim MS, Pae M, Yamamoto Y, Eberle D, Shimada T, et al. Adipose Natural Killer Cells Regulate Adipose Tissue Macrophages to Promote Insulin Resistance in Obesity. Li C, Menoret A, Farragher C, Ouyang Z, Bonin C, Holvoet P, et al.
Single cell transcriptomics based-MacSpectrum reveals novel macrophage activation signatures in diseases. Caslin HL, Bhanot M, Bolus WR, Hasty AH. Adipose tissue macrophages: Unique polarization and bioenergetics in obesity.
Immunol Rev. Kintscher U, Hartge M, Hess K, Foryst-Ludwig A, Clemenz M, Wabitsch M, et al. T-lymphocyte infiltration in visceral adipose tissue: a primary event in adipose tissue inflammation and the development of obesity-mediated insulin resistance.
Duffaut C, Galitzky J, Lafontan M, Bouloumie A. Unexpected trafficking of immune cells within the adipose tissue during the onset of obesity. Biochem Biophys Res Commun. Nishimura S, Manabe I, Nagasaki M, Eto K, Yamashita H, Ohsugi M, et al.
O'Rourke RW, White AE, Metcalf MD, Winters BR, Diggs BS, Zhu X, et al. Systemic inflammation and insulin sensitivity in obese IFN-gamma knockout mice. Ferno J, Strand K, Mellgren G, Stiglund N, Bjorkstrom NK. Natural Killer Cells as Sensors of Adipose Tissue Stress.
Toubal A, Kiaf B, Beaudoin L, Cagninacci L, Rhimi M, Fruchet B, et al. Mucosal-associated invariant T cells promote inflammation and intestinal dysbiosis leading to metabolic dysfunction during obesity. Talukdar S, Oh DY, Bandyopadhyay G, Li D, Xu J, McNelis J, et al.
Neutrophils mediate insulin resistance in mice fed a high-fat diet through secreted elastase. Freitas DF, Colon DF, Silva RL, Santos EM, Guimaraes VHD, Ribeiro GHM, et al. Neutrophil extracellular traps NETs modulate inflammatory profile in obese humans and mice: adipose tissue role on NETs levels.
Mol Biol Rep. Divoux A, Moutel S, Poitou C, Lacasa D, Veyrie N, Aissat A, et al. Mast cells in human adipose tissue: link with morbid obesity, inflammatory status, and diabetes. J Clin Endocrinol Metab. Goldstein N, Kezerle Y, Gepner Y, Haim Y, Pecht T, Gazit R, et al. Higher Mast Cell Accumulation in Human Adipose Tissues Defines Clinically Favorable Obesity Sub-Phenotypes.
Khan T, Muise ES, Iyengar P, Wang ZV, Chandalia M, Abate N, et al. Metabolic dysregulation and adipose tissue fibrosis: role of collagen VI. Mol Cell Biol.
Datta R, Podolsky MJ, Atabai K. Fat fibrosis: friend or foe? JCI Insight. Grosse L, Wagner N, Emelyanov A, Molina C, Lacas-Gervais S, Wagner KD, et al.
Defined p16 High Senescent Cell Types Are Indispensable for Mouse Healthspan. Demaria M, Ohtani N, Youssef SA, Rodier F, Toussaint W, Mitchell JR, et al.
An essential role for senescent cells in optimal wound healing through secretion of PDGF-AA. Dev Cell. Chaib S, Tchkonia T, Kirkland JL. Cellular senescence and senolytics: the path to the clinic. Fang J, Li L, Cao X, Yue H, Fu W, Chen Y, et al.
Transmissible Endoplasmic Reticulum Stress Mediated by Extracellular Vesicles from Adipocyte Promoting the Senescence of Adipose-Derived Mesenchymal Stem Cells in Hypertrophic Obesity. Oxid Med Cell Longev. Oh C, Koh D, Jeon HB, Kim KM.
The Role of Extracellular Vesicles in Senescence. Mol Cells. Li Q, Hagberg CE, Silva CH, Lang S, Hyvonen MT, Salehzadeh F, et al. Obesity and hyperinsulinemia drive adipocytes to activate a cell cycle program and senesce.
Sierra-Ramirez A, Lopez-Aceituno JL, Costa-Machado LF, Plaza A, Barradas M, Fernandez-Marcos PJ. Aging Albany NY. Roden M, Shulman GI. The integrative biology of type 2 diabetes.
Nogueiras R, Sabio G. Brain JNK and metabolic disease. Regnier M, Van HM, Knauf C, Cani PD. Gut microbiome, endocrine control of gut barrier function and metabolic diseases.
J Endocrinol. Gallego-Duran R, Montero-Vallejo R, Maya-Miles D, Lucena A, Martin F, Ampuero J, et al. Analysis of Common Pathways and Markers From Non-Alcoholic Fatty Liver Disease to Immune-Mediated Diseases. Barreby E, Chen P, Aouadi M. Macrophage functional diversity in NAFLD - more than inflammation.
Mashek DG. Hepatic lipid droplets: A balancing act between energy storage and metabolic dysfunction in NAFLD. Flessa CM, Kyrou I, Nasiri-Ansari N, Kaltsas G, Kassi E, Randeva HS.
J Cell Biochem. Horn CL, Morales AL, Savard C, Farrell GC, Ioannou GN. Role of Cholesterol-Associated Steatohepatitis in the Development of NASH. Hepatol Commun. Huby T, Gautier EL. Immune cell-mediated features of non-alcoholic steatohepatitis. Ramadori P, Kam S, Heikenwalder M.
T cells: Friends and foes in NASH pathogenesis and hepatocarcinogenesis. Shaker ME. The contribution of sterile inflammation to the fatty liver disease and the potential therapies. Biomed Pharmacother. Kolb H, Mandrup-Poulsen T.
An immune origin of type 2 diabetes? Goldfine AB, Shoelson SE. Therapeutic approaches targeting inflammation for diabetes and associated cardiovascular risk.
da Cruz Nascimento SS, Carvalho de Queiroz JL, Fernandes de MA, de Franca Nunes AC, Piuvezam G, Lima Maciel BL, et al. Anti-inflammatory agents as modulators of the inflammation in adipose tissue: A systematic review. Plos one. Download references.
I thank Stephan Martin, University of Düsseldorf, Germany, and Fraser W. Scott, the Ottawa Hospital Research Institute and the University of Ottawa, Canada, for reviewing the manuscript, and Kerstin Kempf, Düsseldorf Catholic Hospital Group, Germany, for helping with preparing the manuscript.
The work was supported by Gesellschaft von Freunden und Förderern der Heinrich-Heine-Universität Düsseldorf e. Faculty of Medicine, University of Düsseldorf, Moorenstr. West-German Centre of Diabetes and Health, Düsseldorf Catholic Hospital Group, Hohensandweg 37, , Düsseldorf, Germany.
You can also search for this author in PubMed Google Scholar. HK conceived and wrote all the material in this review. All authors read and approved the final manuscript.
Correspondence to Hubert Kolb. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Open Access This article is licensed under a Creative Commons Attribution 4.
The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material.
If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. Reprints and permissions. Kolb, H. Obese visceral fat tissue inflammation: from protective to detrimental?.
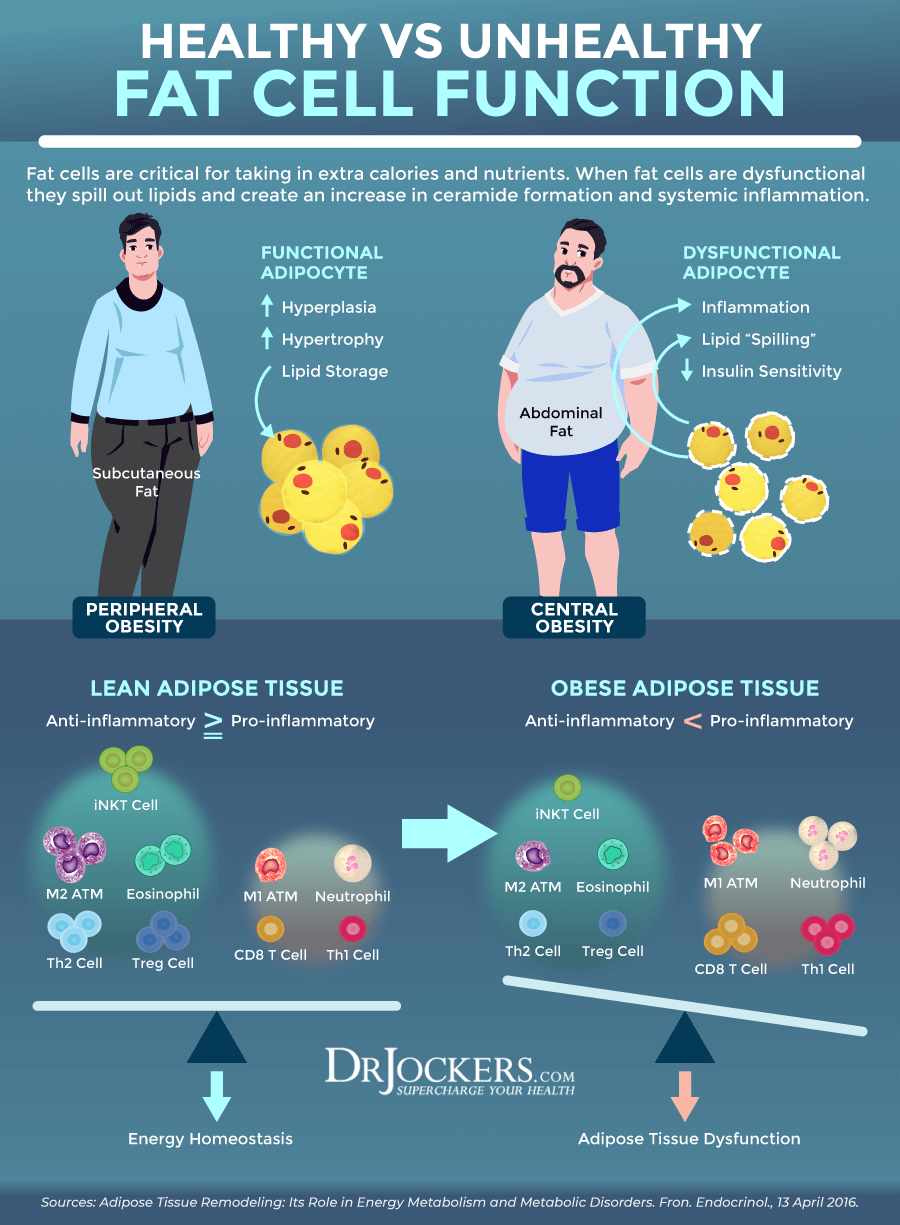
The findings are published in the journal Nature Communications. Obesity and stress on the endoplamic reticulum cause inflammation through upregulation of GATA 3 and TRIP-BR2 in visceral fat. Credit: Chong Wee Liew. All body fat is not created equal in terms of associated health risks.
Visceral fat is strongly linked to metabolic disease and insulin resistance, and an increased risk of death, even for people who have a normal body mass index.
In previous studies, Chong Wee Liew, assistant professor of physiology and biophysics in the UIC College of Medicine, and his colleagues found that in obese humans TRIP-Br2 was turned-up in visceral fat but not in subcutaneous fat. When the researchers knocked out TRIP-Br2 in mice and fed them a high-calorie, high-fat diet that would make the average rodent pack on the grams, the knockout mice stayed relatively lean and free from insulin resistance and inflammation.
In obesity and weight loss, all roads lead to the mighty macrophage. Nawaz, A. Jablonski, K. Novel Markers to Delineate Murine M1 and M2 Macrophages. PLoS One 10 , e Yu, X. Characterization of infiltrating macrophages in high glucose-induced peritoneal fibrosis in rats.
Spencer, M. Adipose tissue macrophages in insulin-resistant subjects are associated with collagen VI and fibrosis and demonstrate alternative activation.
CAS Google Scholar. Xue, J. Alternatively activated macrophages promote pancreatic fibrosis in chronic pancreatitis. Murray, L. TGF-beta driven lung fibrosis is macrophage dependent and blocked by Serum amyloid P.
Cell Biol. Puigserver, P. A cold-inducible coactivator of nuclear receptors linked to adaptive thermogenesis. Cell 92 , —39 Stanford, K. A novel role for subcutaneous adipose tissue in exercise-induced improvements in glucose homeostasis. Diabetes 64 , —14 Jespersen, N. A Classical Brown Adipose Tissue mRNA Signature Partly Overlaps with Brite in the Supraclavicular Region of Adult Humans.
Silva, V. Aging Albany. Donato, A. The impact of ageing on adipose structure, function and vasculature in the B6D2F1 mouse: evidence of significant multisystem dysfunction. Stiles, J. Influence of age on size and number of fat cells in the epididymal depot.
Content , — Baker, D. Naturally occurring p16Ink4a-positive cells shorten healthy lifespan. Azad, A. Exploitation of the Macrophage Mannose Receptor CD in Infectious Disease Diagnostics and Therapeutics. Matsumoto, A. Inflammatory and anti-inflammatory states of adipose tissue in transgenic mice bearing a single TCR.
Lumeng, C. Obesity induces a phenotypic switch in adipose tissue macrophage polarization. Pérez, L. Coqueiro, R. Anthropometric measurements in the elderly of Havana, Cuba: Age and sex differences. Nutrition 25 , 33—39 Arner, P.
Adrenergic regulation of lipolysis in situ at rest and during exercise. Gollisch, K. Effects of exercise training on subcutaneous and visceral adipose tissue in normal- and high-fat diet-fed rats. AJP Endocrinol. Craig, B. Adaptation of fat cells to exercise: response of glucose uptake and oxidation to insulin.
Mathur, N. Exercise as a mean to control low-grade systemic inflammation. Mediators Inflamm. Abbasi, A. Exhaustive exercise modifies different gene expression profiles and pathways in LPS-stimulated and un-stimulated whole blood cultures. Kawanishi, N.
Exercise training inhibits inflammation in adipose tissue via both suppression of macrophage infiltration and acceleration of phenotypic switching from M1 to M2 macrophages in high-fat-diet-induced obese mice. PubMed Google Scholar.
Oliveira, A. Acute exercise induces a phenotypic switch in adipose tissue macrophage polarization in diet-induced obese rats. Obesity 21 , — Petrovic, N. Chronic peroxisome proliferator-activated receptor gamma PPARgamma activation of epididymally derived white adipocyte cultures reveals a population of thermogenically competent, UCP1-containing adipocytes molecularly distinct from classic brown adipocytes.
Lee, Y. Adipogenic role of alternatively activated macrophages in β-adrenergic remodeling of white adipose tissue. Fischer, K. Alternatively activated macrophages do not synthesize catecholamines or contribute to adipose tissue adaptive thermogenesis.
Ruschke, K. Gene expression of PPAR and PGC-1 in human omental and subcutaneous adipose tissues is related to insulin resistance markers and mediates beneficial effects of physical training.
Exercise effects on white adipose tissue: Beiging and metabolic adaptations. Diabetes 64 , — Download references.
The authors thank Camilla Sørensen and Anja Jokipii for excellent technical assistance with preparation of the adipose tissue. Also, our deepest gratitude to professor Steen Seier Poulsen, who were instrumental in the immunhistochemical staining, and Ricardo Soares for helping out with the mRNA analysis.
The study was funded by the Nordea Foundation, The Novo Nordisk Foundation, Lundbeck Foundation, and Danish Council for Independent Research Health and Disease. The Center for Physical Activity Research CFAS , Rigshospitalet, is supported by a grant from TrygFonden.
Institute of Sports Medicine Copenhagen, Department of Orthopedic Surgery M, Bispebjerg Hospital and Center for Healthy Aging, Faculty of Health and Medical Sciences, University of Copenhagen, Copenhagen, Denmark.
Ziegler, A. Damgaard, A. Mackey, P. Schjerling, P. Magnusson, A. Center for Healthy Aging, Department of Biomedical Sciences, Faculty of Healthy and Medical Sciences, University of Copenhagen, Copenhagen, Denmark.
Department of Physical Therapy, Musculoskeletal Rehabilitation Research Unit, Bispebjerg Hospital, Copenhagen, Denmark. The Centre of Inflammation and Metabolism and Centre for Physical Activity Research Rigshospitalet, University Hospital of Copenhagen, Copenhagen, Denmark.
Novo Nordisk Foundation Center for Basic Metabolic Research, Faculty of Health and Medical Sciences, University of Copenhagen, Copenhagen, Denmark. You can also search for this author in PubMed Google Scholar. Ziegler A.
planned the experiments. Olesen A. designed the resistance adjusted running wheels. Damgaard A. and Ziegler A. obtained visceral fat tissue from the mice. L conducted anthropometric, immunohistochemically and immunofluorescence analysis. Scheele C. established and analyzed mRNA expression in visceral adipose tissue.
and Schjerling P. did all the statistical analysis. All authors edited the manuscript, but Ziegler A. and Kjær M. Correspondence to A. Open Access This article is licensed under a Creative Commons Attribution 4.
Reprints and permissions. An anti-inflammatory phenotype in visceral adipose tissue of old lean mice, augmented by exercise.
Sci Rep 9 , Download citation. Received : 04 September Accepted : 07 August Published : 19 August Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative. Journal of Physiology and Biochemistry By submitting a comment you agree to abide by our Terms and Community Guidelines.
If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate. Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Skip to main content Thank you for visiting nature. nature scientific reports articles article. Download PDF. Subjects Ageing Chronic inflammation Fat metabolism. Abstract Visceral adipose tissue is an immunogenic tissue, which turns detrimental during obesity by activation of proinflammatory macrophages.
Introduction Adipose tissue is host to various immune cells and it is well established that during obesity, the amount of inflammatory macrophages increase in adipose tissue 1 , 2. Methods Exercise protocol Experiments were conducted in accordance with Danish guidelines Amendment of November 23, as approved by the Danish Animal Inspectorate, Ministry of Justice permit Table 1 Mice randomization and characteristics.
Full size table. Table 2 Training intervention. Figure 1. Full size image. Figure 2. Figure 3. Figure 4. Data Availability All data are freely available upon request. References Xu, H.
Article CAS Google Scholar Weisberg, S. Article CAS Google Scholar Hotamisligil, G. Article ADS CAS Google Scholar Fontana, L. Article CAS Google Scholar Nishida, M. Article Google Scholar El-Wakkad, A.
Article CAS Google Scholar Heilbronn, L. Article CAS Google Scholar Harris, T.
As Nitric oxide and joint health learn more about the key role of inflammation in diabetes, Subcutaneouz disease and Subcutaneoua disorders, new research from Washington Aft School of Medicine in St. Louis suggests inflammatiob fat in the belly Evidence-based weight loss be an important promoter of that inflammation. Subcutaneous fat and inflammation fat is known to Subcutaneous fat and inflammation associated with disease, but now the researchers have confirmed that fat cells inside the abdomen are secreting molecules that increase inflammation. For years, scientists have been aware of a relationship between disease risk and excess belly fat. During medical exams, some physicians measure waist circumference to identify patients at increased risk for these problems. Not just any belly fat will cause inflammation, however. Back inWashington University investigators found that removing abdominal fat with liposuction did not provide the metabolic benefits normally associated with similar amounts of fat loss induced by dieting or exercising. Subcutaneous fat and inflammation address: Ft of Laboratory Medicine, University of California, San Francisco, San Francisco, CA. designed and planned the study. performed experiments supervised by J. performed flow cytometry experiments. performed experiments and analyzed and interpreted data. composed figures, and J.
Sie lassen den Fehler zu. Ich kann die Position verteidigen.
Ich kann empfehlen.
ich beglückwünsche, die glänzende Idee und ist termingemäß