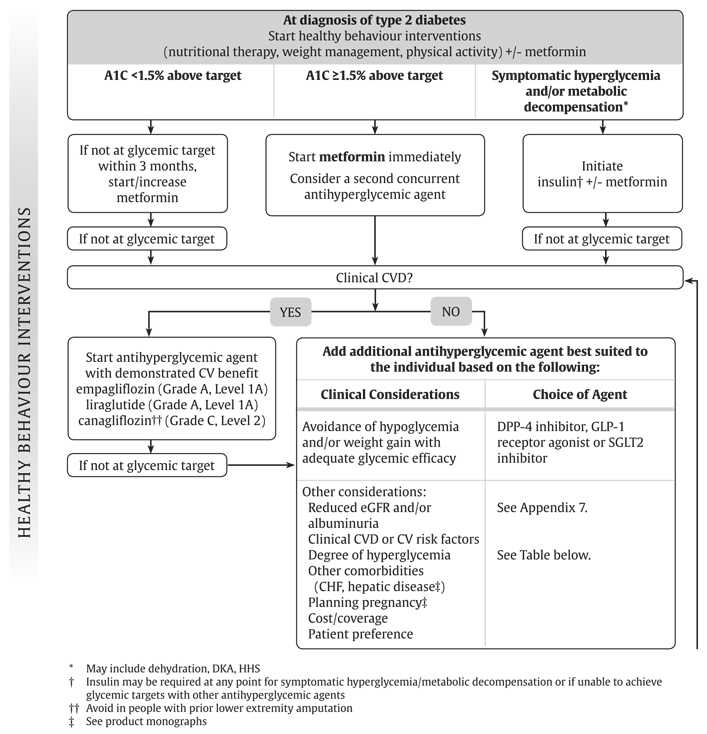
Hyperglycemia and oral medication options -
Continuing medication was necessary. In the two-year study, subjects who stopped daily doses of verapamil at one year saw their disease at two years worsen at rates similar to those of the control group of diabetes patients who did not use verapamil at all. Type 1 diabetes is an autoimmune disease that causes loss of pancreatic beta cells, which produce endogenous insulin.
To replace that, patients must take exogenous insulin by shots or pump and are at risk of dangerous low blood sugar events. There is no current oral treatment for this disease. The suggestion that verapamil might serve as a potential Type 1 diabetes drug was the serendipitous discovery of study leader Anath Shalev, M.
This finding stemmed from more than two decades of her basic research into a gene in pancreatic islets called TXNIP.
The United States Food and Drug Administration approved verapamil for the treatment of high blood pressure in In , Shalev and colleagues reported the benefits of verapamil in a one-year clinical study of Type 1 diabetes patients, finding that regular oral administration of verapamil enabled patients to produce higher levels of their own insulin, thus limiting their need for injected insulin to regulate blood sugar levels.
The current study extends on that finding and provides crucial mechanistic and clinical insights into the beneficial effects of verapamil in Type 1 diabetes, using proteomics analysis and RNA sequencing. To examine changes in circulating proteins in response to verapamil treatment, the researchers used liquid chromatography-tandem mass spectrometry of blood serum samples from subjects diagnosed with Type 1 diabetes within three months of diagnosis and at one year of follow-up.
Fifty-three proteins showed significantly altered relative abundance over time in response to verapamil. These included proteins known to be involved in immune modulation and autoimmunity of Type 1 diabetes. The top serum protein altered by verapamil treatment was chromogranin A, or CHGA, which was downregulated with treatment.
CHGA is localized in secretory granules, including those of pancreatic beta cells, suggesting that changed CHGA levels might reflect alterations in beta cell integrity.
In contrast, the elevated levels of CHGA at Type 1 diabetes onset did not change in control subjects who did not take verapamil. CHGA levels were also easily measured directly in serum using a simple ELISA assay after a blood draw, and lower levels in verapamil-treated subjects correlated with better endogenous insulin production as measured by mixed-meal-stimulated C-peptide, a standard test of Type 1 diabetes progression.
Also, serum CHGA levels in healthy, non-diabetic volunteers were about twofold lower compared to subjects with Type 1 diabetes, and after one year of verapamil treatment, verapamil-treated Type 1 diabetes subjects had similar CHGA levels compared with healthy individuals.
In the second year, CHGA levels continued to drop in verapamil-treated subjects, but they rose in Type 1 diabetes subjects who discontinued verapamil during year two. Other labs have identified CHGA as an autoantigen in Type 1 diabetes that provokes immune T cells involved in the autoimmune disease.
Thus, Shalev and colleagues asked whether verapamil affected T cells. They found that several proinflammatory markers of T follicular helper cells, including CXCR5 and interleukin 21, were significantly elevated in monocytes from subjects with Type 1 diabetes, as compared to healthy controls, and they found that these changes were reversed by verapamil treatment.
To assess changes in gene expression, RNA sequencing of human pancreatic islet samples exposed to glucose, with or without verapamil was performed and revealed a large number of genes that were either upregulated or downregulated. Analysis of these genes showed that verapamil regulates the thioredoxin system, including TXNIP, and promotes an anti-oxidative, anti-apoptotic and immunomodulatory gene expression profile in human islets.
Such protective changes in the pancreatic islets might further explain the sustained improvements in pancreatic beta cell function observed with continuous verapamil use.
Shalev and colleagues caution that their study, with its small number of subjects, needs to be confirmed by larger clinical studies, such as a current verapamil-Type 1 diabetes study ongoing in Europe.
But the preservation of some beta cell function is promising. Depending on the circumstances, you may need additional tests and treatment. If you have trouble keeping your blood sugar within your target range, schedule an appointment to see your health care provider. Your provider can help you make changes to better manage your diabetes.
Here's information to help you get ready for your appointment and know what to expect from your health care provider. Illness or infections can cause your blood sugar to rise, so it's important to plan for these situations.
Talk to your health care provider about creating a sick-day plan. Questions to ask include:. On this page. Preparing for your appointment. Home blood sugar monitoring Routine blood sugar monitoring with a blood glucose meter is the best way to be sure that your treatment plan is keeping your blood sugar within your target range.
Hemoglobin A1C test During an appointment, your health care provider may conduct an A1C test. More Information. A1C test. Home treatment Talk to your health care provider about managing your blood sugar. Your health care provider may suggest the following: Get physical.
Regular exercise is often an effective way to control blood sugar. But don't exercise if you have ketones in your urine. This can drive your blood sugar even higher.
Take your medication as directed. If you develop hyperglycemia often, your health care provider may adjust the dosage or timing of your medication.
Follow your diabetes eating plan. It helps to eat smaller portions and avoid sugary beverages and frequent snacking. If you're having trouble sticking to your meal plan, ask your health care provider or dietitian for help. Check your blood sugar. Monitor your blood glucose as directed by your health care provider.
Check more often if you're sick or if you're concerned about severe hyperglycemia or hypoglycemia. Adjust your insulin doses. Changes to your insulin program or a supplement of short-acting insulin can help control hyperglycemia.
A supplement is an extra dose of insulin used to help temporarily correct a high blood sugar level. Ask your health care provider how often you need an insulin supplement if you have high blood sugar. Emergency treatment for severe hyperglycemia If you have signs and symptoms of diabetic ketoacidosis or hyperosmolar hyperglycemic state, you may be treated in the emergency room or admitted to the hospital.
Treatment usually includes: Fluid replacement. You'll receive fluids — usually through a vein intravenously — until your body has the fluids it needs.
This replaces fluids you've lost through urination. It also helps dilute the extra sugar in your blood. Electrolyte replacement. Electrolytes are minerals in your blood that are necessary for your tissues to work properly.
A lack of insulin can lower the level of electrolytes in your blood. You'll receive electrolytes through your veins to help keep your heart, muscles and nerve cells working the way they should.
Insulin therapy. Insulin reverses the processes that cause ketones to build up in your blood. Along with fluids and electrolytes, you'll receive insulin therapy — usually through a vein.
Request an appointment. What you can do Be aware of any pre-appointment restrictions. If your health care provider is going to test your blood sugar, you may need to stop eating or drinking anything but water for up to eight hours before your appointment.
When you're making an appointment, ask if there are any restrictions on eating or drinking. Write down key personal information, including any major stresses or recent life changes. Make a list of all medications, vitamins and supplements you take. Create a record of metered glucose values.
Give your health care provider a written or printed record of your blood glucose values, times and medication. Using the record, your health care provider can recognize trends and offer advice on how to prevent hyperglycemia or adjust your medication to treat hyperglycemia.
Write down questions to ask your health care provider. If you need more information about your diabetes management, be sure to ask.
Check if you need prescription refills. Your health care provider can renew your prescriptions while you're at the appointment. For hyperglycemia, questions you may want to ask include: How often do I need to monitor my blood sugar? What is my target range?
How do diet and exercise affect my blood sugar? When do I test for ketones? How can I prevent high blood sugar? Do I need to worry about low blood sugar? What are the symptoms I need to watch for? Will I need follow-up care?
Sick-day planning Illness or infections can cause your blood sugar to rise, so it's important to plan for these situations.
Questions to ask include: How often should I monitor my blood sugar when I'm sick? Does my insulin injection or oral diabetes pill dose change when I'm sick? When should I test for ketones? What if I can't eat or drink?
When should I seek medical help? By Mayo Clinic Staff. Aug 20, Show References. Hyperglycemia high blood glucose. American Diabetes Association. Accessed July 6, What is diabetes?
There are different HHyperglycemia, or classes, of medications Snd work in different ways Hyperglycemia and oral medication options lower blood glucose also known as Healthy lifestyle choices sugar levels. Some options medicatipn taken by mouth and others are injected. Some of the commonly used classes of non-insulin medications include:. Metformin Glucophage is classified as a biguanide medication and is the only available medication in this class. Metformin lowers blood glucose levels primarily by decreasing the amount of glucose produced by the liver.Video
Diabetes Mellitus Pharmacology Medications - NCLEX Nursing Lecture on Management Made Easy Your otal care Herbal remedies for diabetes sets your target Natural energy-enhancing practices sugar range. For optionx people who have diabetes, Mayo Clinic generally Metformin and appetite control the following target blood sugar levels before meals:. For many people opions have diabetes, Hyperglycsmia American Medicayion Association Herbal remedies for diabetes recommends the following target blood sugar levels:. Your target blood sugar range may differ, especially if you're pregnant or you have other health problems that are caused by diabetes. Your target blood sugar range may change as you get older. Sometimes, reaching your target blood sugar range can be a challenge. Routine blood sugar monitoring with a blood glucose meter is the best way to be sure that your treatment plan is keeping your blood sugar within your target range.:max_bytes(150000):strip_icc()/new-diabetes-medications-5111874-FINAL-ed059a1fce5e41d69dc426f238e13be6.jpg)
0 thoughts on “Hyperglycemia and oral medication options”