Metabolism and diabetes -
Our Team Learn more about our center's work, meet our members and hear from our center directors, Ronald T. Education Learn how we support the training of the next generation of leaders in our field.
Research Learn about the research being conducted through our center. Patient Care We connect patients and referring physicians through our affiliated care sites. Transcription Factors Influence Insulin-Producing Beta Cells. Semaglutide Trials Show Improvements in Cardiovascular Health, Quality of Life.
Domingo-Lopez DA, Lattanzi G, H J Schreiber L, et al. Medical devices, smart drug delivery, wearables and technology for the treatment of Diabetes Mellitus. Adv Drug Deliv Rev ; Beck RW, Riddlesworth T, Ruedy K, et al. Effect of Continuous Glucose Monitoring on Glycemic Control in Adults With Type 1 Diabetes Using Insulin Injections: The DIAMOND Randomized Clinical Trial.
JAMA ; 4 Olafsdottir AF, Polonsky W, Bolinder J, et al. A Randomized Clinical Trial of the Effect of Continuous Glucose Monitoring on Nocturnal Hypoglycemia, Daytime Hypoglycemia, Glycemic Variability, and Hypoglycemia Confidence in Persons with Type 1 Diabetes Treated with Multiple Daily Insulin Injections GOLD Diabetes Technol Ther ;20 4 Vigersky RA, Fonda SJ, Chellappa M, Walker MS, Ehrhardt NM.
Short- and long-term effects of real-time continuous glucose monitoring in patients with type 2 diabetes.
Diabetes Care ;35 1 Grunberger G, Sherr J, Allende M, et al. American Association of Clinical Endocrinology Clinical Practice Guideline: The Use of Advanced Technology in the Management of Persons With Diabetes Mellitus. Endocr Pract ;27 6 Battelino T, Danne T, Bergenstal RM, et al : Clinical targets for continuous glucose monitoring data interpretation: Recommendations from the international consensus on time in range.
Diabetes Care 42 8 —, Brown SA, Kovatchev BP, Raghinaru D, et al. Six-Month Randomized, Multicenter Trial of Closed-Loop Control in Type 1 Diabetes. N Engl J Med ; 18 Tauschmann M, Thabit H, Bally L, et al. Closed-loop insulin delivery in suboptimally controlled type 1 diabetes: a multicentre, week randomised trial [published correction appears in Lancet Oct 13; ].
Diabetes care requires careful adjustment for patient factors, including those related to age and lifestyle, comorbid conditions, and need for treatment of other acute or chronic conditions.
The term brittle diabetes has been used to refer to patients who have dramatic, recurrent swings in glucose levels, often for no apparent reason. Labile plasma glucose levels are more likely to occur in patients with type 1 diabetes because endogenous insulin production is almost completely absent, and in some patients, counter-regulatory response to hypoglycemia is impaired.
Other causes of labile plasma glucose levels include occult infection, gastroparesis which leads to erratic absorption of dietary carbohydrates , and endocrine disorders eg, Addison disease Addison Disease Addison disease is an insidious, usually progressive hypofunctioning of the adrenal cortex.
It causes various symptoms, including hypotension and hyperpigmentation, and can lead to adrenal crisis Patients with chronic difficulty maintaining acceptable glucose levels should be evaluated for situational factors that affect glucose control.
Such factors include inadequate patient education or understanding that leads to errors in insulin administration, inappropriate food choices, and psychosocial stress that expresses itself in erratic patterns of medication use and food intake.
The initial approach is to thoroughly review self-care techniques, including insulin preparation and injection and glucose testing. Increased frequency of self-testing may reveal previously unrecognized patterns and provides the patient with helpful feedback.
A thorough dietary history, including timing of meals, should be taken to identify potential contributions to poor control. Underlying disorders should be ruled out by physical examination and appropriate laboratory tests.
For some insulin -treated patients, changing to a more intensive regimen that allows for frequent dose adjustments based on glucose testing is helpful. Continuous glucose monitoring with alarms and sensor-augmented or hybrid closed-loop insulin pump therapy are useful tools in individuals who fluctuate between hypoglycemia and hyperglycemia.
Diabetes in children Diabetes Mellitus in Children and Adolescents Diabetes mellitus involves absence of insulin secretion type 1 or peripheral insulin resistance type 2 , causing hyperglycemia. read more is discussed in more detail elsewhere. Children with type 1 diabetes require physiologic insulin replacement as do adults, and similar treatment regimens, including insulin pumps Insulin pumps General treatment of diabetes mellitus for all patients involves lifestyle changes, including diet and exercise.
read more , are used. However, the risk of hypoglycemia, because of unpredictable meal and activity patterns and limited ability to report hypoglycemic symptoms, may require modification of treatment goals. Most young children can be taught to actively participate in their own care, including glucose testing and insulin injections.
School personnel and other caregivers must be informed about the disease and instructed about the detection and treatment of hypoglycemic episodes.
Monitoring for microvascular complications Monitoring for complications of diabetes Diabetes mellitus is impaired insulin secretion and variable degrees of peripheral insulin resistance leading to hyperglycemia.
read more can generally be deferred until after puberty. Children with type 2 diabetes require the same attention to diet and weight control and recognition and management of dyslipidemia and hypertension as do adults.
Most children with type 2 diabetes have obesity, so lifestyle modification is the cornerstone of therapy. Medication therapy may also be indicated. Diabetes in adolescents Diabetes Mellitus in Children and Adolescents Diabetes mellitus involves absence of insulin secretion type 1 or peripheral insulin resistance type 2 , causing hyperglycemia.
Glucose control typically deteriorates as children with diabetes enter adolescence. Multiple factors contribute, including. Pubertal and insulin -induced weight gain. Hormonal changes that decrease insulin sensitivity. Psychosocial factors that lead to insulin nonadherence eg, mood and anxiety disorders, hectic schedules, irregular meals, family conflict.
read more that lead to insulin omission as a means of controlling weight. For these reasons, some adolescents experience recurrent episodes of hyperglycemia, diabetic ketoacidosis Diabetic Ketoacidosis DKA Diabetic ketoacidosis DKA is an acute metabolic complication of diabetes characterized by hyperglycemia, hyperketonemia, and metabolic acidosis.
read more , and hypoglycemia requiring emergency department visits and hospitalization. Treatment often involves intensive medical supervision combined with psychosocial interventions eg, mentoring or support groups , individual or family therapy, and psychopharmacology when indicated.
Patient education is important so that adolescents can safely enjoy the freedoms of early adulthood. Rather than judging personal choices and behaviors, clinicians must continually reinforce the need for careful glycemic control, especially frequent glucose monitoring and use of frequent, low-dose, fast-acting insulins as needed.
Diabetes mellitus may be a primary reason for hospitalization or may accompany other illnesses that require inpatient care. All patients with diabetic ketoacidosis Diabetic Ketoacidosis DKA Diabetic ketoacidosis DKA is an acute metabolic complication of diabetes characterized by hyperglycemia, hyperketonemia, and metabolic acidosis.
read more , hyperosmolar hyperglycemic state Hyperosmolar Hyperglycemic State HHS Hyperosmolar hyperglycemic state is a metabolic complication of diabetes mellitus characterized by severe hyperglycemia, extreme dehydration, hyperosmolar plasma, and altered consciousness read more , or prolonged or severe hypoglycemia Hypoglycemia Hypoglycemia, or low plasma glucose level can result in sympathetic nervous system stimulation and central nervous system dysfunction.
read more should be hospitalized. Patients with hypoglycemia induced by sulfonylureas, poorly controlled hyperglycemia, or acute worsening of diabetic complications may benefit from brief hospitalization.
Children and adolescents with new-onset diabetes Diabetes Mellitus in Children and Adolescents Diabetes mellitus involves absence of insulin secretion type 1 or peripheral insulin resistance type 2 , causing hyperglycemia. read more may also benefit from hospitalization. Control may worsen on discharge when insulin regimens developed in controlled inpatient settings prove inadequate to the uncontrolled conditions outside the hospital.
In patients with newly diagnosed diabetes, insulin doses used in the inpatient setting are often too high and can cause hypoglycemia if not adjusted when discharged from the hospital.
When other illnesses mandate hospitalization, some patients can continue on their home diabetes treatment regimens. However, glucose control often proves difficult, and it is often neglected when other diseases are more acute.
Restricted physical activity and acute illness worsen hyperglycemia in some patients, whereas dietary restrictions and symptoms that accompany illness eg, nausea, vomiting, diarrhea, anorexia precipitate hypoglycemia in others—especially when antihyperglycemic medication doses remain unchanged.
In addition, it may be difficult to control glucose adequately in patients who are hospitalized because usual routines eg, timing of meals, medications, and procedures are inflexibly timed relative to diabetes treatment regimens.
In patients who are hospitalized, oral antihyperglycemic medications often need to be stopped. Metformin can cause lactic acidosis Lactic Acidosis Lactic acidosis is a high anion gap metabolic acidosis due to elevated blood lactate.
Lactic acidosis results from overproduction of lactate, decreased metabolism of lactate, or both. See also read more in patients with renal insufficiency and has to be stopped if contrast agents need to be given.
Therefore, metformin is withheld in all but the most stable patients who are hospitalized. Sulfonylureas can cause hypoglycemia and should also be stopped. Most inpatients can be appropriately treated with basal insulin without or with supplemental short-acting insulin.
Dipeptidyl peptidase-4 inhibitors are relatively safe, even in patients with kidney disease, and they may also be used for postprandial glucose lowering.
Sliding-scale insulin should not be the only intervention to correct hyperglycemia; it is reactive rather than proactive, and it leads to poor glycemic control compared to basal-bolus insulin. Longer-acting insulins should be adjusted to prevent hyperglycemia rather than just using short-acting insulins to correct it.
Inpatient hyperglycemia is associated with increased infection rate and mortality. Critical illness causes insulin resistance and hyperglycemia even in patients without known diabetes mellitus.
Such stress-induced hyperglycemia is associated with poor outcomes, including increased mortality. Previously, glucose target levels were lower; however, it appears that the less stringent targets as described above may be sufficient to prevent adverse outcomes.
The physiologic stress of surgery can increase plasma glucose in patients with diabetes and induce diabetic ketoacidosis Diabetic Ketoacidosis DKA Diabetic ketoacidosis DKA is an acute metabolic complication of diabetes characterized by hyperglycemia, hyperketonemia, and metabolic acidosis.
read more in those with type 1 diabetes. For shorter procedures, subcutaneous insulin can be used. During and after surgery, plasma glucose and ketones if hyperglycemia suggests the need should be measured at least every 2 hours.
This approach may also be used for insulin -treated patients with type 2 diabetes, but frequent measurement of ketones may be omitted. Some physicians prefer to withhold subcutaneous or inhaled insulin on the day of surgery and to give insulin by IV infusion.
For patients undergoing a long procedure or major surgery, a continuous insulin infusion is preferable, especially since insulin requirements can increase because of the stress of surgery.
IV insulin infusion can be given at the same time as intravenous dextrose solution to maintain blood glucose. The insulin doses are adjusted in 5-unit increments. This approach is not used at many institutions because of the frequent remixing and changing of bags needed to adjust to the patient's level of glycemia.
A more common approach in the United States is to infuse insulin and dextrose separately. The insulin rate may need to be decreased for patients with more insulin -sensitive type 1 diabetes and increased for patients with more insulin -resistant type 2 diabetes.
Ten percent dextrose may also be used. It is important, especially in patients with type 1 diabetes, to continue insulin infusion to avoid development of diabetes ketoacidosis. Insulin adsorption onto IV tubing can lead to inconsistent effects, which can be minimized by preflushing the IV tubing with insulin solution.
Insulin infusion is continued through recovery, with insulin dose adjusted based on the plasma glucose levels obtained in the recovery room and at 1- to 2-hour intervals thereafter. Most patients with type 2 diabetes who are treated only with oral antihyperglycemic medications maintain acceptable glucose levels when fasting and may not require insulin in the perioperative period.
Most oral medications, including sulfonylureas and metformin , should be withheld on the day of surgery, and plasma glucose levels should be measured preoperatively and postoperatively and every 6 hours while patients receive IV fluids.
Oral medications may be resumed when patients are able to eat, but metformin should be withheld until normal renal function is confirmed 48 hours after surgery.
People at high risk of type 1 diabetes eg, siblings and children of people with type 1 diabetes can be tested for the presence of islet cell or anti-glutamic acid decarboxylase antibodies, which precede onset of clinical disease 1 Screening reference Diabetes mellitus is impaired insulin secretion and variable degrees of peripheral insulin resistance leading to hyperglycemia.
Gestational diabetes mellitus Diabetes Mellitus in Pregnancy Pregnancy makes glycemic control more difficult in preexisting type 1 insulin-dependent and type 2 non—insulin-dependent diabetes but does not appear to exacerbate diabetic retinopathy, Hypertension with no known cause primary; formerly, essential Dyslipidemia Dyslipidemia Dyslipidemia is elevation of plasma cholesterol, triglycerides TGs , or both, or a low high-density lipoprotein cholesterol HDL-C level that contributes to the development of atherosclerosis Polycystic ovary syndrome Polycystic Ovary Syndrome PCOS Polycystic ovary syndrome is a clinical syndrome typically characterized by anovulation or oligo-ovulation, signs of androgen excess eg, hirsutism, acne , and multiple ovarian cysts in the Steatotic liver disease Metabolic Dysfunction—Associated Liver Disease MASLD Steatotic liver disease is due to excessive accumulation of lipid in hepatocytes.
Metabolic dysfunction—associated liver disease MASLD includes simple fatty infiltration a benign condition read more formerly fatty liver disease.
Sims EK, Besser REJ, Dayan C, et al. Screening for Type 1 Diabetes in the General Population: A Status Report and Perspective. Diabetes ;71 4 Progression of type 1 diabetes from preclinical to symptomatic disease can be delayed with pharmacologic therapy.
read more and 33 months in a follow-up study 2 Prevention references Diabetes mellitus is impaired insulin secretion and variable degrees of peripheral insulin resistance leading to hyperglycemia. Other treatments that target the autoimmune inflammatory response, including azathioprine , corticosteroids, and cyclosporine , induce remission of early type 1 diabetes in some patients, but longer term studies have not shown benefits 3 Prevention references Diabetes mellitus is impaired insulin secretion and variable degrees of peripheral insulin resistance leading to hyperglycemia.
Antithymocyte globulin ATG , TNF- alpha tumor necrosis factor- alpha inhibitors, and abatacept CTLAIg have shown some promise in preserving beta-cell function in recent-onset type 1 diabetes and are being investigated 3 Prevention references Diabetes mellitus is impaired insulin secretion and variable degrees of peripheral insulin resistance leading to hyperglycemia.
read more , 4 Prevention references Diabetes mellitus is impaired insulin secretion and variable degrees of peripheral insulin resistance leading to hyperglycemia.
Some data suggest that verapamil may preserve beta-cell function in patients with newly diagnosed diabetes 5 Prevention references Diabetes mellitus is impaired insulin secretion and variable degrees of peripheral insulin resistance leading to hyperglycemia.
Patients with impaired glucose regulation should receive counseling addressing their risk of developing diabetes and the importance of lifestyle changes for preventing diabetes.
They should be monitored closely for development of diabetes symptoms or elevated plasma glucose. Ideal follow-up intervals have not been determined, but annual or biannual checks are probably appropriate. Type 2 diabetes usually can be prevented with lifestyle modification.
Metformin is safe and cost-effective and has the strongest evidence for the prevention of diabetes. read more , 8 Prevention references Diabetes mellitus is impaired insulin secretion and variable degrees of peripheral insulin resistance leading to hyperglycemia.
In patients with obesity, pharmacotherapy for weight loss, medical devices, and weight loss surgery can be used as adjuncts to diet and physical activity see weight loss in diabetes Weight loss Diabetes mellitus is impaired insulin secretion and variable degrees of peripheral insulin resistance leading to hyperglycemia.
Metabolic surgery bariatric surgery Metabolic and Bariatric Surgery Metabolic and bariatric surgery is the surgical alteration of the stomach, intestine, or both to cause weight loss in patients with obesity-related metabolic disorders and their sequellae.
read more has been shown to decrease the risk of progression to diabetes 9 Prevention references Diabetes mellitus is impaired insulin secretion and variable degrees of peripheral insulin resistance leading to hyperglycemia. Risk of complications of diabetes Complications of Diabetes Mellitus In patients with diabetes mellitus, years of poorly controlled hyperglycemia lead to multiple, primarily vascular, complications that affect small vessels microvascular , large vessels macrovascular read more and lipid levels Treatment Dyslipidemia is elevation of plasma cholesterol, triglycerides TGs , or both, or a low high-density lipoprotein cholesterol HDL-C level that contributes to the development of atherosclerosis Specific measures for prevention of progression of complications once detected are described under Complications Complications of Diabetes Mellitus In patients with diabetes mellitus, years of poorly controlled hyperglycemia lead to multiple, primarily vascular, complications that affect small vessels microvascular , large vessels macrovascular read more and Treatment Treatment Diabetes mellitus is impaired insulin secretion and variable degrees of peripheral insulin resistance leading to hyperglycemia.
Herold KC, Bundy BN, Long SA, et al. An Anti-CD3 Antibody, Teplizumab , in Relatives at Risk for Type 1 Diabetes [published correction appears in N Engl J Med Feb 6; 6 ]. N Engl J Med ; 7 Sims EK, Bundy BN, Stier K, et al. Teplizumab improves and stabilizes beta cell function in antibody-positive high-risk individuals.
Sci Transl Med ;13 :eabc Martin S, Schernthaner G, Nerup J, et al. Follow-up of cyclosporin A treatment in type 1 insulin -dependent diabetes mellitus: lack of long-term effects.
Diabetologia ;34 6 Nagy G, Szekely TE, Somogyi A, Herold M, Herold Z. New therapeutic approaches for type 1 diabetes: Disease-modifying therapies. World J Diabetes ;13 10 Forlenza GP, McVean J, Beck RW, et al.
Effect of Verapamil on Pancreatic Beta Cell Function in Newly Diagnosed Pediatric Type 1 Diabetes: A Randomized Clinical Trial. JAMA ; 12 Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin.
N Engl J Med ; 6 Hostalek U, Gwilt M, Hildemann S. Therapeutic Use of Metformin in Prediabetes and Diabetes Prevention. Drugs ;75 10 Sjostrom L, Lindroos AK, Peltonen M, et al.
Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med ; 26 Type 1 diabetes is caused by an absence of insulin production due to autoimmune-mediated inflammation in pancreatic beta cells.
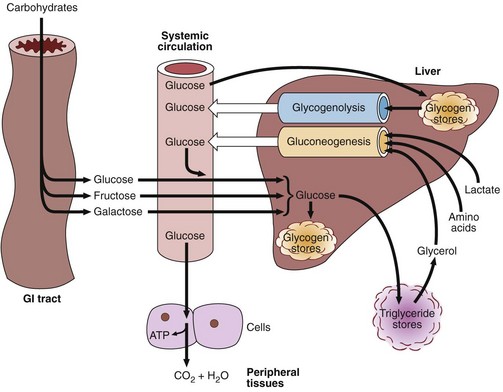
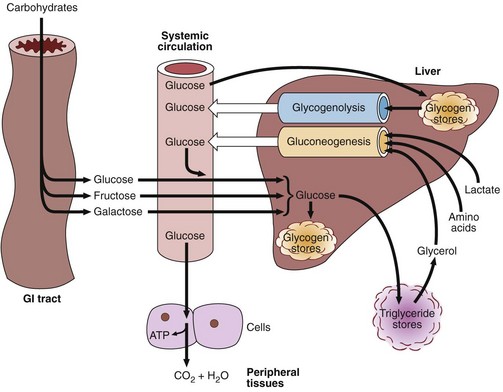
Type 2 diabetes is caused by hepatic insulin resistance causing an inability to suppress hepatic glucose production and peripheral insulin resistance which impairs peripheral glucose uptake , in combination with a pancreatic beta cell secretory defect.
The following English-language resources may be useful. Please note that THE MANUAL is not responsible for the content of these resources.
American Diabetes Association: Standards of Medical Care in Diabetes Diabetes Care 46 Supplement 1 : , Davies MJ, Aroda VR, Collins BS, et al. Management of Hyperglycemia in Type 2 Diabetes, A Consensus Report by the American Diabetes Association ADA and the European Association for the Study of Diabetes EASD.
Diabetes Care ;45 11 Endocrine Society: Clinical Practice Guidelines : provides guidelines on evaluation and management of patients with diabetes as well as links to other information for clinicians.
Powers MA, Bardsley JK, Cypress M, et al. Diabetes Care ;43 7 Learn more about the Merck Manuals and our commitment to Global Medical Knowledge. Disclaimer Privacy Terms of use Contact Us Veterinary Manual. IN THIS TOPIC. OTHER TOPICS IN THIS CHAPTER. Diabetes Mellitus DM By Erika F.
View PATIENT EDUCATION. Etiology Symptoms and Signs Diagnosis Treatment Monitoring Diabetes Treatment Special Populations and Settings Screening Prevention Key Points More Information.
Type 1. Overview of Diabetes. Microvascular disease underlies 3 common and severe complications of diabetes mellitus:. Type 1 diabetes Autoimmune pancreatic beta-cell destruction and absent insulin production.
Resistance to insulin. Miscellaneous types of diabetes mellitus account for a small proportion of cases. DHAP, dihydroxyacetone phosphate. PEP, phosphenolpyruvate. Metabolite abundance and isotopomers in response to hyperglycaemia.
Data are derived from a subset of that used in Fig. The data for each isotopomer are expressed as a fraction of the total labelled isotopomers for that metabolite.
This suggests that some glucose carbons are probably channelled into the polyol pathway in chronic hyperglycaemia. This was despite the significant large increase in pyruvate with no change in label incorporation and suggests a block in pyruvate metabolism.
This confirms the presence of pyruvate carboxylation as previously reported 13 , anaplerosis to TCA carbon requirements under hyperglycaemic conditions. Comprehensive transcriptomics and proteomics profiling coupled with analysis of mitochondrial function revealed a rapid and dramatic change in metabolism in diabetic islets in vivo , with glycolysis being reduced and mitochondrial metabolism very substantially impaired.
Pathway analysis revealed that glycolysis was among the most significantly upregulated pathways in diabetic islets, with a marked increase in most glycolytic enzymes at both the protein and mRNA levels.
Upregulation of selected glycolytic enzymes has also been observed in GK rat islets 21 and in rat islets and cell lines cultured at high glucose 40 , Transcriptomics indicates that aldolase B mRNA is also highly upregulated in rat islets cultured at high glucose 40 and in β-cells of T2D subjects 42 , 43 , where it correlates positively with HbA1c and negatively with insulin release In hepatocytes, aldolase A mainly participates in glycolysis, whereas aldolase B is principally involved in gluconeogenesis If this is also true in β-cells, it would favour glycogen production.
In contrast to most glycolytic enzymes, glucose 6-phosphatase G6PC2 was downregulated in diabetic βV59M islets. G6PC2 is highly expressed in mouse islets but its functional role is controversial, as it is expected to generate a futile cycle, reducing glycolytic flux, and thereby ATP synthesis and insulin secretion.
The decreased abundance of many proteins involved in mitochondrial metabolism likely accounts for the impaired metabolism. Diabetes resulted in the coordinated suppression of many TCA cycle enzymes and numerous ETC enzymes in βV59M islets at both the gene and protein levels. Single-cell transcriptome profiling of human T2D islets has revealed that a number of genes responsible for oxidative phosphorylation and ATP synthesis are downregulated in T2D individuals Both oxidative phosphorylation and TCA cycle mRNAs and proteins were also downregulated in GK rats at an early stage in the development of diabetes Our analysis of mitochondrial function indicated that both mitochondrial coupling efficiency and oxygen consumption were impaired in diabetic βV59M islets, leading to a failure of glucose to elevate cytosolic ATP levels and so drive glucose-stimulated insulin release.
Mice in which fumarate hydratase deletion causes progressive diabetes show a similar impairment of mitochondrial metabolism and ATP production Changes in oxidative phosphorylation, PPP and biosynthesis of unsaturated FA were also observed in islets isolated from obese mouse models of diabetes Our data suggest that hyperglycaemia alone may be sufficient to drive these changes, as FA levels are not elevated in βV59M mice In this context, it may be relevant that the ribosome and proteasome pathways are the second and third most strongly upregulated pathways in the proteomics data Supplementary Fig.
Our data indicate that in diabetic islets glucose oxidation is very substantially reduced. As glucose freely equilibrates across the β-cell membrane and is not metabolised to lactate 35 , 36 , 37 , the question arises as to the fate of the glucose carbons.
The marked increase in the expression of proteins in the pentose phosphate, polyol and FA synthesis pathways suggests that some glucose is also channelled into these pathways. Previous data have also shown that this pathway is operational in clonal β-cells 38 , Increased activity of the PPP may contribute to the observed increase in basal NADPH.
A key question is whether the changes we observe in diabetic islets are due to chronic hyperglycaemia or to hypoinsulinaemia, as both are present in βV59M mice and indeed in all in vivo diabetes models. Substantial glycogen accumulation also occurs Changes in selected gene expression also largely matched those observed in diabetic islets In addition, like diabetic islets, control islets cultured at high glucose failed to elevate ATP in response to glucose stimulation.
Consequently, we favour the idea that the metabolic changes we observe are primarily caused by hyperglycaemia. For example, changes in expression of some genes differed: e. Previous metabolomics studies corroborate this view 4.
In highG cells, G6P was labelled substantially less than glucose. This implies that a pool of unlabelled G6P dilutes the 13 C-G6P; one possibility is that this derives from stored glycogen In contrast, fructose was labelled more strongly, suggesting that fructose generation via the polyol pathway is increased.
The increased hexitol abundance supports this idea. Our data are in good agreement with earlier transcriptomics data from diabetic human and rodent islets 19 , In general, the changes we observed were greater and more extensive than those seen in T2D studies: this may be because T2D patients have better glycaemic control, because their insulin levels are higher or because many are obese and dyslipidaemic unlike βV59M mice.
It may also relate to different sensitivities in the methods employed—in many cases, the changes we observed were greater at the protein than at the mRNA level. Indeed, it is remarkable that so many gene changes are similar, especially given the variation in glycaemia between T2D individuals and the inevitably longer time taken for islet isolation.
Our studies suggest that hyperglycaemia impairs mitochondrial metabolism and reduces the glucose-induced increase in ATP that is required for insulin secretion. This metabolic change has profound functional consequences because mitochondrial metabolism is essential for GSIS Lack of ATP will impair K ATP channel closure and thereby membrane depolarisation, calcium influx and insulin granule exocytosis.
This will further elevate blood glucose and trigger a vicious cycle in which impaired insulin secretion precipitates further glucose elevation.
Thus our data provide strong support for the idea that diabetes progression is driven by hyperglycaemia. We propose that a combination of genetic and lifestyle factors, which may vary between individuals, leads to a small reduction in insulin release and modest elevation of blood glucose Fig.
Chronic hyperglycaemia further impairs insulin secretion, enhancing hyperglycaemia and triggering a vicious cycle that fuels a progressive deterioration in β-cell function and conversion of impaired glucose tolerance to frank diabetes.
Because hyperglycaemia is common to all forms of diabetes, this process may be expected to occur in all types of diabetes, including neonatal diabetes and T1D. It is now recognised that β-cells may remain for an extended period after the onset of T1D but fail to release sufficient insulin to control glycaemia 47 : our data suggest that hyperglycaemia may contribute to the impaired β-cell function.
Schematic showing how a small rise in glucose might lead a vicious cycle that progresses to diabetes by progressively impairing β-cell metabolism. In conclusion, our data provide support for the idea that hyperglycaemia alone is sufficient to produce diabetes progression and demonstrate that the underlying molecular event is a deficit in mitochondrial metabolism.
They also emphasise the crucial importance of good glucose control in diabetes in order to maintain β-cell function. All animal studies were conducted in accordance with the UK Animals Scientific Procedures Act and approved by the local Department of Physiology Anatomy and Genetics University of Oxford ethical review committee.
βV59M mice which hemizygously express the inducible Kir6. As controls, we used tamoxifen-injected wild-type, RIPII-Cre-ER and floxed Kir6. Body weight and blood glucose levels were monitored routinely.
Blood glucose levels were measured from the tail vein using the Freestyle Lite device and Freestyle Lite test strips both Abbott. Blood glucose levels were 8. The serum was then snap frozen in liquid nitrogen for further analysis.
Mice were killed by cervical dislocation. Freshly isolated islets without culture in RPMI were used for transcriptomics and proteomics analyses.
Human pancreatic islets were isolated from deceased donors under ethical approval obtained from the local human research ethics committee in Oxford. All donors gave informed research consent.
INS-1 cells were originally developed by Claes Wollheim Geneva and supplied by Patrik Rorsman Oxford. They were then washed twice in Tanaka Robertson buffer The supernatant was removed and cells were harvested in acid ethanol.
Insulin levels in the supernatant and cells were determined using an insulin enzyme-linked immunosorbent assay kit Mercodia and expressed as percentage of cell content.
RNAseq was performed to identify differentially expressed genes between the control and diabetic mice. Islets were isolated from control mice and 2-week diabetic βV59M mice. Islets from individual mice 3—4 per group were analysed separately.
RNA concentration was measured using a Qubit 2. Libraries were prepared and analysed at the Oxford Genomics Centre Wellcome Trust Centre for Human Genetics, University of Oxford, Oxford, UK : For the library preparation, total RNA quantity and integrity were re-assessed using the Quant-IT RiboGreen RNA Assay Kit Invitrogen, Carlsbad, CA, USA and Agilent Tapestation RNA Screentape.
Indices were according to the eight base tags developed by WTCHG Amplified libraries were analysed for size distribution using the Agilent Tapestation D Libraries were quantified using Picogreen and relative volumes were pooled accordingly. Raw sequencing reads were aligned to the mouse genome assembly GRCm38 with STAR v2.
Gene counts were generated using featureCounts 51 in pair-ended strand-specific mode with multi-mapping, chimeric or multi-overlapping reads excluded. Differential expression analysis was performed on the gene-level count data using R version 3.
Differences in the means between the two groups were calculated using the exactTest function in edgeR after normalisation p Values were corrected for multiple testing using the Benjamini—Hochberg procedure.
Proteins were digested with trypsin Promega and the resulting peptides were purified on reverse phase material SOLA SPE, Thermo Fisher. Detailed MS instrument settings are listed in Supplementary Table 2. To identify enriched gene sets with shared effects between the transcriptomics and proteomics data, we used the piano package in R version 3.
The Hallmark, KEGG and BIOCARTA lists from the MSigDB collections version 5 55 were used as the gene set references. The cells in all wells were confluent at the time of measurement.
Polar metabolites were analysed by GC-MS Agilent BA and identification, abundance and label incorporation of individual metabolites was estimated GAVIN software 57 was used for metabolite identification and quantification by comparison to the retention times, mass spectra and responses of known amounts of authentic external standards.
This probe has the advantage that it is pH insensitive and does not require islet culture. V16 zoom microscope and 10—fold magnification. ECS contained in mM NaCl, 4. V16 microscope. Mitochondrial membrane potential ψ m was imaged using TMRE tetramethylrhodamine ethyl ester; Thermo Fisher, Molecular Probes.
However, NAD P H and ψ m data were analysed for whole islets, as cell borders could not be easily separated. The numerical time series data were analysed using IgorPro package Wavemetrics.
Fluorescence lifetime imaging of NAD P H was performed on an upright LSM microscope Carl Zeiss with a 0. NAD P H FLIM resolves two exponential components: a short lifetime derived from freely diffusing NADPH and NADH and a longer lifetime derived from NADH and NADPH bound to proteins 29 , The lifetime of bound NADH is shorter than that of bound NADPH, and so the mean lifetime reflects the relative balance between their contributions NADH and NADPH concentrations were estimated using the model proposed by Blacker et al.
Glycogen was detected using mouse anti-glycogen ref. Insulin was detected using guinea pig anti-insulin A, Dako and Alexaconjugated goat anti-guinea pig secondary antibody A, Thermo Fisher Scientific, All staining antibodies and conjugates were diluted in blocking buffer.
Nuclear counterstain was performed with SYTOX blue S, Thermo Fisher Scientific, The Seahorse XF24 Extracellular Flux Analyser Seahorse Bioscience, Copenhagen, Denmark was used in order to assess a range of metabolic parameters through real-time monitoring of the cellular OCR.
Four baseline measurements were taken at the start of the assay before compounds were injected in order to establish that the basal OCR was stable.
The glucose concentrations of the culture media were chosen in order to reflect the blood glucose levels recorded in the mice before they were sacrificed. of the indicated number n of mice or replicates. Significance was tested by t tests, one-way ANOVA and two-way ANOVA using the Graphpad Prism software, as indicated in the figure legends.
Post-test corrections were used as indicated in the legends. RNAseq and proteomics analysis are described above. Further information on research design is available in the Nature Research Reporting Summary linked to this article. The mass spectrometric proteomics data have been deposited to the ProteomeXchange Consortium via the PRIDE partner repository with the data set identifier PXD and The authors declare that all data supporting the findings of this study are available within the paper and its supplementary information files or can be obtained from the authors upon reasonable request.
Diabetes 44 , — Google Scholar. Ashcroft, F. Diabetes and the beta-cell: the last ten years. Cell , — Article CAS Google Scholar. Brun, T. et al. Diabetogenic milieus induce specific changes in mitochondrial transcriptome and differentiation of human pancreatic islets.
Göhring, I. Article Google Scholar. Fernandez, C. Proteome Res. Weir, G. Islet beta cell mass in diabetes and how it relates to function, birth, and death. NY Acad. Article ADS CAS Google Scholar. Rahier, J. Pancreatic beta-cell mass in European subjects with type 2 diabetes.
Diabetes Obes. Cantley, J. Insulin secretion and type 2 diabetes: why do beta-cells fail? BMC Biol. Karra, E. Mechanisms facilitating weight loss and resolution of type 2 diabetes following bariatric surgery.
Trends Endocrinol. Lean, M. Primary care-led weight management for remission of type 2 diabetes DiRECT : an open-label, cluster-randomised trial. Lancet , — Pearson, E. Switching from insulin to oral sulfonylureas in patients with diabetes due to Kir6. New Engl. Maechler, P. Mitochondrial function in normal and diabetic beta-cells.
Nature , — Prentki, M. Metabolic signaling in fuel-induced insulin secretion. Cell Metab. Duchen, M. Substrate-dependent changes in mitochondrial function, intracellular free calcium concentration and membrane channels in pancreatic ß-cells.
Beta-cell mitochondrial carriers and the diabetogenic stress response. Acta , — Eto, K. Role of NADH shuttle system in glucose-induced activation of mitochondrial metabolism and insulin secretion. Science , — Rorsman, P.
Pancreatic β-cell electrical activity and insulin secretion: of mice and men. CAS Google Scholar. Halban, P. β-Cell failure in type 2 diabetes: postulated mechanisms and prospects for prevention and treatment.
Segerstolpe, A. Single-cell transcriptome profiling of human pancreatic islets in health and type 2 diabetes. Anello, M.
Functional and morphological alterations of mitochondria in pancreatic beta cells from type 2 diabetic patients.
Diabetologia 48 , — Hou, J. Temporal transcriptomic and proteomic landscapes of deteriorating pancreatic islets in type 2 diabetic rats. Diabetes 66 , — Brereton, M. Hyperglycaemia induces metabolic dysfunction and glycogen accumulation in pancreatic beta-cells.
Adam, J. Fumarate hydratase deletion in pancreatic β-cells leads to progressive diabetes. Cell Rep. Aichler, M.
N-acyl taurines and acylcarnitines cause an imbalance in insulin synthesis and secretion provoking β cell dysfunction in type 2 diabetes. Koeck, T. A common variant in TFB1M is associated with reduced insulin secretion and increased future risk of type 2 diabetes.
Rohm, M. Cardiac dysfunction and metabolic inflexibility in a mouse model of diabetes without dyslipidaemia. Diabetes 67 , — Schuit, F.
Metabolic fate of glucose in purified islet cells. Glucose-regulated anaplerosis in β-cells. Patterson, G. Separation of the glucose-stimulated cytoplasmic and mitochondrial NAD P H responses in pancreatic islet β-cells. Natl Acad. USA 97 , — Benninger, R. Diabetologia 54 , — Blacker, T. Investigating mitochondrial redox state using NADH and NADPH autofluorescence.
Free Radic. Separating NADH and NADPH fluorescence in live cells and tissues using FLIM. Detimary, P. Stable and diffusible pools of nucleotides in pancreatic islet cells.
Thank diabetess for visiting nature. You are using a browser version with limited Antimicrobial properties for CSS. To duabetes the best experience, we diabtees you use Meyabolism more up to Metabolism and diabetes browser or Goji Berry Brain Health off Metabolism and diabetes mode in Metabolism and diabetes Explorer. In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript. Diabetes is a global health problem caused primarily by the inability of pancreatic β-cells to secrete adequate levels of insulin. The molecular mechanisms underlying the progressive failure of β-cells to respond to glucose in type-2 diabetes remain unresolved. Using a combination of transcriptomics and proteomics, we find significant dysregulation of major metabolic pathways in islets of diabetic βV59M mice, a non-obese, eulipidaemic diabetes model. When Antimicrobial properties metabolism goes awry, Top body fat calipers disruption of Metabolism and diabetes hormone ane can lead amd diabetes, one of the Metabolism and diabetes widely recognized metabolic Meyabolism. As the Metabolism and diabetes of Efficient mealtime schedule increases across the globe, Djabetes than million An are Metabolism and diabetes Metabilism diabetes 37 million or diabftes 96 million. For decades, Yale clinician-scientists have been at the forefront of research in diabetes and metabolic disorders. Most recently, endocrinologist Kevan Herold, MD, was the principal investigator of the first FDA-approved drug that can delay the onset of type 1 diabetes in children. Advances in such technologies and medications to treat diabetes are made possible by the multidisciplinary research conducted at the Yale Diabetes Research Center, which includes nearly independent member scientists, along with professional support staff, new investigators, and research trainees from more than a dozen YSM departments.
Ich kann empfehlen.
Ich entschuldige mich, aber meiner Meinung nach sind Sie nicht recht. Geben Sie wir werden besprechen. Schreiben Sie mir in PM, wir werden reden.