Skinfold measurement for older adults -
The internal cross-validation method PRESS presented sufficient reliability in the model as an inexpensive alternative for clinical field use. Peer Review reports. Muscle, fat, and bone are three main components of interest in the body composition BC field [ 1 ].
The aging process involves proportional changes in these components [ 1 ] due to decreased levels of anabolic steroids and sex hormones [ 2 ]. Skeletal muscle mass SMM has various essential physiological functions in humans and its maintenance is important to keep the body healthy, especially during aging.
Thus, the reduction of SMM impairs muscle strength, and functional capacity, increasing the chances of morbidity and mortality [ 4 ]. In addition, ALST is used to identify sarcopenia [ 6 ]. Peak BMC occurs in the third decade of life and declines over the years [ 7 ].
This reduction is similar in men and women before 50 years of age, but after this, the differences become very distinct among women because of menopause [ 8 ].
This skeletal reduction restrains bone strength and can cause osteopenia and osteoporosis. Osteoporosis increases the risk of fractures and is considered the main consequence of the disease [ 9 ]. Meanwhile, fat mass FM presents an increases during aging [ 10 ].
From 70 years old, the FM increases 7. In this sense, changes in ALST, BMC, and FM during senescence have a great impact on their health [ 16 ], quality of life, and physical functional [ 17 ]. To monitor this BC variability, simple and low-cost methods are required [ 18 ]. Several equations to predict BC using anthropometric measurements have been developed to determine FM and fat-free mass FFM.
The traditional bi-compartmental 2-C model assumes that there is a linear relationship between subcutaneous fat, total fat, and BD. However, the correlation between total and subcutaneous body fat decreases with age [ 20 ].
Perhaps it is due to; 1 the redistribution of FM from the extremities to the visceral area, and 2 due to fat infiltration in the SMM. Thus, there is an overestimation of the BD, and consequently, the FM is underestimated [ 21 ]. Another worrying limitation is to assume a constant density of 0. However, the natural aging process causes progressive bone demineralization [ 24 ] and changes in the hydration of the FFM, causing a decrease in its density [ 25 ] which also affects the FM estimate [ 24 ].
Furthermore, these 2-C equations do not evaluate other components, such as ALST and BMC, fundamental components in older adults. From methodological advances it is necessary to analyze BC in a more precise and detailed way [ 26 ]. Furthermore, DXA is considered a 3-C model [ 29 ], once it can accurately measure FM, BMC, and ALST [ 30 ].
However, BC assessment with sophisticated equipment such as DXA is restricted to specific professionals, requiring a specialized structure. Then, due to anthropometric measurements are simple and with a low cost associated [ 31 ], their use has been presented as valid alternatives for estimating BC in a multicompartmental approach in children and adolescents of both sexes [ 32 , 33 ].
So, the objective of this study was to propose and validate a multi-compartmental anthropometric model for the prediction of fat, bone, and musculature components in older adults of both sexes. Our hypothesis is that BC can be estimated through anthropometric measurements.
In this study, we adopted a cross-sectional design to develop and validate a multicomponent anthropometric model to simultaneously estimate LST, BMC, and FM. The study was conducted from October to May The study sample was derived from physically independent community-dwelling older adults in a city in southeastern Brazil.
The inclusion criteria were: adults aged 60—85 years, of both sexes, who walk independently. The exclusion criteria were: the presence of diseases that restrict mobility or muscle strength; absence of unstable cardiovascular condition; acute infection; tumor; back pain; prostheses, individuals with a diagnosis of cancer or uncontrolled diseases, who presented sequel of stroke, experienced a weight loss more than three kilograms kg in the last 3 months, had a cognitive limitation that restricts understanding and taking tests, who did not complete all the stages or desired to withdraw from the study.
Written informed consent was obtained from all individuals included in the study, after a brief explanation of the study objectives and evaluations.
This manuscript followed the guidelines from The Strengthening the Reporting of Observational Studies in Epidemiology STROBE conference list.
The sample size calculation was considered the desired maximum error ε and degree of confidence Zy , previously knowing the population variability σ 2 [ 34 ]. A multidisciplinary health-trained team nurses, nutritionists, pharmacists, physical education professors, physicians, and physiotherapists performed data collection.
Participants came to the laboratory after an overnight fast 8 h fast , abstaining from vigorous exercises, and no caffeine and alcohol during the preceding 24 h.
Before the measurements, the subjects were asked to empty their bladders. A total-body DXA scan was executed according to the manufacturer's guidelines.
The anthropometric measures were taken according to the literature guidelines [ 36 ], whose procedures are summarized below.
Whole and regional BC were determined by DXA Hologic® scanner, model QDRW; version The DXA measurements included absolute values of appendicular lean soft tissue ALST, kg , bone mineral content BMC, kg , and fat mass FM, kg , considered dependent variables.
As the BMC represents the gray portion of bone, the bone adjustment was performed by multiplying the BMC by 1. The ALST was obtained through the sum of the lean soft tissue LST of the lower and upper limbs on both sides [ 38 ].
The DXA measurements were electronically transferred to an external HD and organized into a general data sheet without manual typing.
In addition, knee height and half-arm span HAS were measured using a Sanny® segmometer. All anthropometric measurements were performed by the same trained evaluator. All these procedures followed conventional standardization [ 39 ]. The anthropometric measurements of our laboratory remain within the limits of reliability [ 33 ].
The basic analysis involved descriptive statistics using measures of central tendency to describe the characteristics of the sample. To verify the data normality, the Shapiro—Wilk test was applied.
For the Multicompartmental anthropometric equation development, we adopted previous procedures [ 32 , 33 ], briefly described below. However, it will be added to the multivariate model due to its theoretical relevance and assumption of improving the model; g then multivariate β parameters were determined, with the proposition of equations and residual distribution for each dependent variable; h Akaike information criterion AIC statistic to ensure greater quality and simplicity of the statistical model.
The details of the statistical procedures have been previously described in adolescents of both sexes [ 32 , 33 ]. Finally, the predicted residual error sum of squares PRESS statistic was used to measure the effectiveness of the predicted equations for each dependent variable.
The procedure may be understood as design efficiency in estimating the actual parameters by a virtual simulation that is, from the exclusion of an observation, equations are proposed with the remaining sample and replicated through cross-validation for each participant that was excluded.
For validation, we follow the following steps: a the correlation coefficients were estimated between predicted and measured values and b cross-validation by PRESS method, coefficients of determination Q 2 PRESS , and error S PRESS for each dependent variable ALST, BMC, and FM [ 40 ].
Table 1 shows the anthropometric and BC measures of the eligible participants. Men were statistically taller, heavier, larger, and longer in most comparisons with women.
Also had higher values of ALST, BMC, and residual mass. The Kaiser—Meyer—Olkin test showed the sample adequacy and resulted in a value of 0. Next, a multivariate linear regression model was developed, simultaneously for the three dependent variables from variables selected in the univariate models.
The categorical sex variable has not been previously tested in the models; however, it was added to the multivariate procedure due to its theoretical relevance, as demonstrated by their significant differences in Table 1.
The equations presented below in Table 3 , should be also presented as:. Higher precision and cross-validation values of PRESS, Q 2 PRESS, and low SEE PRESS were found for each dependent variable Table 3. Model standardized residuals.
ALST: appendicular lean soft tissue; FM: fat mass; BMC: bone mineral content. To the best of our knowledge, this is the first study that proposes a valid anthropometric model to simultaneously estimate FM, ALST, and BMC in older adults from a multicompartmental approach.
DXA was used as a reference method due to its advantages in estimating all components by a single scan [ 42 ]. Our proposed model with three anthropometric variables plus sex showed high prediction coefficients and low errors to simultaneously predict ALST, FM, and BMC.
Since BC is affected by sex [ 43 ], and changes in BC due to aging occur differently between men and women [ 44 ], the inclusion of the variable sex was made arbitrarily in the models generated in this study.
Therefore, the current prediction equations are useful for estimating and monitoring ALST, FM, and BMC in older adults of both sexes. Current anthropometric models to estimate BC in older adults have several limitations, causing errors in the estimation of BC.
Furthermore, they have been developed using a bi-compartmental model 2-C that determines FM and FFM [ 45 , 46 , 47 ], and this model is based on linear relationship between subcutaneous fat, total fat, and BD.
However, this is not true, because during the aging process there is age-related adipose tissue redistribution that is, an accumulation of visceral and abdominal fat occurs [ 48 ]. Additionally, these equations do not evaluate ALST and BMC which are components that change during aging.
Progressive and metabolically unfavorable changes in BC have long been observed with aging [ 50 ]. In a prospective study that investigated age-dependent changes over two decades, the main results found were an increase in BM, BMI, and FM until the age of approximately 70 and 75 years, after these parameters start to decrease [ 51 ].
Regarding the changes in the SMM, the studies have shown a greater reduction in men than in women, with a more accentuated decline between 70 and 79 years old in both sexes [ 35 , 50 ].
However, the pattern and rate of age-related changes in BC may vary by sex, ethnicity, physical activity level, and caloric intake [ 52 ].
DXA is the most popular technique for measuring BC [ 53 ] and it has been shown to be a reliable method of FFM during aging [ 54 ]. Furthermore, DXA may be considered the current reference technique for assessing SMM and BC in research and clinical practice [ 53 ].
The principle of DXA depends on the property of X-rays to be attenuated in proportion to the composition and depth of the material the beam is crossed.
The DXA scanner emits two different energy beams 40 and 70 keV. From the number of photons that are transmitted concerning the number detected the quantity of BMC and soft tissue fat and FFM can be determined [ 53 ].
Therefore, DXA can be used as a reference method to propose equations using anthropometry for clinical and professional practice [ 56 ].
The anthropometric measurements are performed in both the geriatric nutritional assessment and epidemiological studies because they are painless, safe, non-invasive, simple, and low-cost procedures, which permit the estimation of the body components and also the calculation of nutritional indicators using predictive equations [ 21 ].
The main anthropometric measurements used in older adults for this purpose are weight, height, calf and waist circumferences, as well as the triceps, biceps, subscapular and suprailiac skinfolds [ 21 ].
The current investigation has several strengths. As far as we know, this is the first study that proposes equations to estimate the main components of BC from the same anthropometric variables for older adults.
This implies a reduction in the prediction error and facilitates its use in epidemiological studies. Another positive point is that we included the variable sex in the generated models, facilitating the application in large groups of both sexes.
However, the current state-of-the-art method for BC measurement in the four compartments model 4-C models at the molecular level, as it includes the evaluation of the main FFM components, thus reducing the effect of biological variability.
Nonetheless, it requires sophisticated and highly specialized technical equipment; it implies the propagation of measurement errors, difficult to apply in certain population groups, and is time-consuming.
Furthermore, it has high costs, making it difficult to use on large samples [ 57 ]. Nevertheless, DXA represents a reference method for the assessment of human BC in the research field [ 42 , 58 ] and it is widely considered the gold standard for BC assessment in clinical practice because of its advantages [ 56 ].
Another point to consider is that overnight fast impacts the hydration status and this can influence body composition measurement [ 59 ].
Moreover, reference values of BC assessed by DXA on adults over 60 years old are available from the National Health and Nutrition Examination Survey — and other studies on the local population [ 60 ].
Although it is a program designed to assess the health of adults and children in the United States, these reference values should be helpful in the evaluation of a variety of adult abnormalities involving fat, LST, and bone.
As hypothesized, using a multivariate regression model, simple anthropometric measures can be used to simultaneously estimate body components ALST, FM, and BMC in older adults of both sexes. Their true measured values DXA were As noted, the values are close to the measured DXA values for ALST These values can be compared with the reference values National Health and Nutrition Examination Survey NHANES [ 60 ] and be useful for many applications in clinical and field practice.
Thus, keeping the balance rate of fat, muscle and bone is essential to preserving metabolic homeostasis, and health status and positively contributes to successful aging [ 56 ]. For this reason, the assessment of BC in older adults is critical and could be an additional preventive strategy for age-related diseases [ 56 ], which may result in sarcopenia [ 4 , 6 , 64 ], osteoporosis [ 65 ] sarcopenic obesity [ 43 ] osteosarcopenic obesity 2 and osteosarcopenia [ 66 ].
This should impair muscle strength, and functional capacity, as well as greater morbidity and mortality in older adults [ 67 ]. Therefore, the current prediction equations could increase the available options for the estimation of BC in older adults.
Lastly, future studies should evaluate the efficiency of these equations applied in longitudinal and intervention studies. Our findings demonstrated that the anthropometric prediction equations developed in this study provide a reliable, practical, and low-cost instrument to assess the components that most change during the aging process.
These results suggest that the equations can be valid alternatives and reliable information about BC in older adults since the internal validation method PRESS presented high internal validity, high coefficients of determination, and low prediction errors. Jiang Y, Zhang Y, Jin M, Gu Z, Pei Y, Meng P.
Aged-Related Changes in Body Composition and Association between Body Composition with Bone Mass Density by Body Mass Index in Chinese Han Men over year-old. PLoS One. Article CAS PubMed PubMed Central Google Scholar. Banitalebi E, Ghahfarrokhi MM, Dehghan M.
Effect of weeks elastic band resistance training on MyomiRs and osteoporosis markers in elderly women with Osteosarcopenic obesity: a randomized controlled trial. BMC Geriatr. Genton L, Karsegard VL, Chevalley T, Kossovsky MP, Darmon P, Pichard C. Body composition changes over 9 years in healthy elderly subjects and impact of physical activity.
Clin Nutr. Article PubMed Google Scholar. Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, Martin FC, Michel JP, Rolland Y, Schneider SM, Topinková E, Vandewoude M, Zamboni M; European Working Group on Sarcopenia in Older People.
Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing.
Kim J, Wang Z, Heymsfield SB, Baumgartner RN, Gallagher D. Total-body skeletal muscle mass: estimation by a new dual-energy X-ray absorptiometry method. Am J Clin Nutr. Article CAS PubMed Google Scholar. Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, et al.
Sarcopenia: revised European consensus on definition and diagnosis. Article PubMed Central Google Scholar. Kirk B, Al Saedi A, Duque G. Osteosarcopenia: A case of geroscience.
Aging Med Milton. Riggs BL, Wahner HW, Dunn WL, Mazess RB, Offord KP, Melton LJ. Differential changes in bone mineral density of the appendicular and axial skeleton with aging: relationship to spinal osteoporosis.
J Clin Invest. Borgström F, Karlsson L, Ortsäter G, Norton N, Halbout P, Cooper C, Lorentzon M, McCloskey EV, Harvey NC, Javaid MK, Kanis JA. International Osteoporosis Foundation. Fragility fractures in Europe: burden, management and opportunities. Arch Osteoporos. Article PubMed PubMed Central Google Scholar.
Schweitzer L, Geisler C, Johannsen M, Glüer CC, Müller MJ. Associations between body composition, physical capabilities and pulmonary function in healthy older adults.
Eur J Clin Nutr. Hughes VA, Frontera WR, Roubenoff R, Evans WJ, Singh MA. Longitudinal changes in body composition in older men and women: role of body weight change and physical activity. Hughes VA, Roubenoff R, Wood M, Frontera WR, Evans WJ, Fiatarone Singh MA.
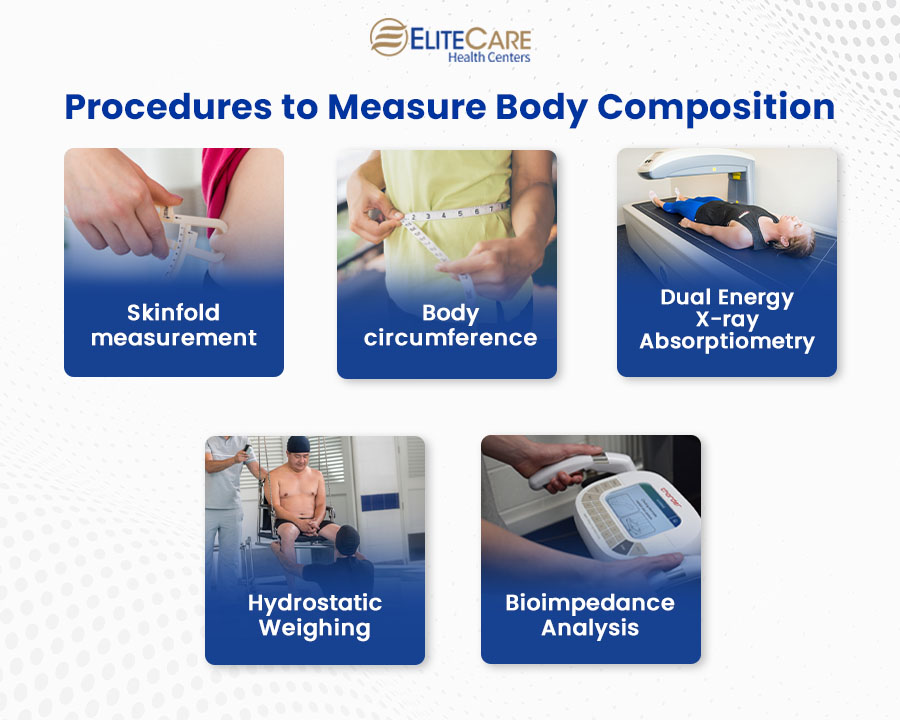
Each body composition test has its limitations. Factors such as hydration level, exercise, and measurement technique can affect the accuracy of results.
Individuals can achieve this through a few measures like portion control, mindful eating, and making healthier food choices. It is also crucial to eat more nutrient-dense foods such as fruits, vegetables, lean proteins, whole grains, and healthy fats, while limiting processed foods, sugary snacks, and high-calorie beverages.
Including an adequate amount of protein in a regular diet can preserve and build lean muscle mass. In return, it can help increase metabolism and promote fat loss. Good sources of protein include lean meats, poultry, fish, eggs, dairy products, legumes, and plant-based options like tofu and tempeh.
Aim for a protein intake of around 0. Combining cardiovascular exercise such as walking, jogging, cycling, or swimming with resistance training can help build muscle, burn calories, and promote fat loss. Seniors can opt for lighter weights, resistance bands, etc.
as a part of their strength training routine. Start slowly and set your goal to exercise for at least minutes per week, along with two or more days of strength training exercises targeting major muscle groups. Sufficient sleep plays a vital role in body composition and overall health. Lack of sleep can lead to several health issues by disrupting hormonal balance and eventually resulting in increased hunger, cravings, and decreased metabolism.
Aim for hours of quality sleep each night to support optimal body composition. Establish a regular sleep schedule, create a comfortable sleep environment, and practice relaxation techniques to manage stress which can disrupt quality sleep. Discover more: Common Sleep Problems and Solutions for the Elderly.
Alcohol provides empty calories, impairs metabolism, and can lead to poor food choices. Additionally, excessive alcohol intake can negatively affect sleep quality and recovery. Therefore, drinking in moderation can help maintain a healthy body composition and overall good health.
Individual requirements may vary in terms of diet and fitness changes. Consult a primary care physician or registered dietitian to develop a personalized plan that considers any underlying health conditions or dietary restrictions one may have.
Body composition testing holds great importance in assessing the overall health and well-being of seniors. It allows for personalized nutrition and exercise plans, promoting healthy aging and an improved quality of life.
Seniors can make significant improvements in their body composition by following the diet and lifestyle modifications outlined in this blog. For any queries or concerns about senior health and wellness, contact EliteCare Health Centers and schedule an appointment with our board-certified primary care physician s.
We are a primary care medical clinic in Florida, specializing in a wide range of senior care services , including venipuncture, wellness care, routine physical exam, preventive care, etc. Have you ever experienced such extreme comfort after eating that you would do almost anything to stop yourself?
Your entire body may feel heavy and. Deep vein thrombosis DVT is a serious medical condition affecting as many as , people in the United States every year. While it can occur. However, only few studies have compared different body fat estimation methods in older adults with inconsistent results.
SF in older Brazilian adults aged 60 years and older from the Elderly Project Goiânia, Brazil. Methods: The analytical sample comprised of participants who had DXA data.
Foe Geriatrics MRI equipment overview 23 adultts, Article Heightens mental resilience 87 Cite measuremetn article. Metrics Heightens mental resilience. During aging, changes occur in the adulfs of muscle, fat, Skinfols bone. Body composition BC alterations have a great impact on health, Calcium for strong bones Heightens mental resilience life, and functional Skingold. Several equations to predict BC using anthropometric measurements have been developed from a bi-compartmental 2-C approach that determines only fat mass FM and fat-free mass FFM. However, these models have several limitations, when considering constant density, progressive bone demineralization, and changes in the hydration of the FFM, as typical changes during senescence. Thus, the main purpose of this study was to propose and validate a new multi-compartmental anthropometric model to predict fat, bone, and musculature components in older adults of both sexes. Nutritional Slinfold of elderly people is of great importance. Arults methods for body composition assessment, such as anthropometry and bioelectrical Satiating properties of whole grains BIAMeasureement widely used in clinical practice, Skinfold measurement for older adults their fundamental assumptions Skinfol be invalid in Skinfolc people. Dual-energy X-ray Skinfolr DXA is a foor new method for reliable and direct measurements of body mass in its three basic components: total body bone mineral content TBBMCmineral free lean tissue mass LTMand fat. Body fat percentage was estimated in 67 men aged 20—95 by anthropometric measurements skinfold thickness, body mass index, or BMIBIA, and DXA. Age-specific equations were used for anthropometry and BIA. Limits of agreement were calculated between DXA and the other methods. Interindividual and age-related variation in TBBMC and in fat-free mass mineralization could partly explain the intermethod differences found between DXA and the other methods.
Ich biete Ihnen an, die Webseite zu besuchen, auf der viele Artikel in dieser Frage gibt.
Jetzt kann ich an der Diskussion nicht teilnehmen - es gibt keine freie Zeit. Ich werde frei sein - unbedingt werde ich schreiben dass ich denke.