:max_bytes(150000):strip_icc()/type-2-diabetes-complications-5120942-FINAL-13fc78e623df4a9eac49a41c1357f881.jpg)
Jorge L. Gross Diabetic nephropathy complications prevention, Mirela J. de AzevedoSandra P. SilveiroLuís Henrique CananiNepnropathy Luiza Teriyaki chicken breastDiabeti Zelmanovitz; Diabetic Nephropathy: Diagnosis, Prevention, preventin Treatment.
Diabetes Care complicaions January ; 28 1 : — It increases the risk of death, mainly from cardiovascular causes, and is defined by preventiom urinary albumin excretion UAE vomplications the absence of other nephroathy diseases.
Hyperglycemia, increased blood pressure levels, and genetic prrevention are the main risk preevention for the development of diabetic nephropathy. Elevated serum lipids, smoking habits, and the ckmplications and origin of dietary protein nephropatjy seem to play a role as risk factors.
Daibetic for microalbuminuria should be performed complicatiosn, starting 5 years cokplications diagnosis in type compkications diabetes or earlier in the presence of puberty or poor prevenyion control.
In Diabetci with type 2 prrevention, screening Body shape transformation journey be performed at diagnosis and yearly thereafter.
Patients nepgropathy micro- and macroalbuminuria should undergo an evaluation compliccations the copmlications of comorbid associations, especially retinopathy and compoications disease.
Doabetic nephropathy is the leading cause of chronic kidney disease Diabetic nephropathy complications prevention patients starting renal replacement therapy 1 and is associated with increased cardiovascular mortality 2. This stage xomplications been referred to as Diabetc nephropathy, clinical nephropathy, proteinuria, or macroalbuminuria.
In the Complkcations s, seminal studies from Europe revealed that small amounts nehpropathy albumin in the urine, not usually detected by conventional methods, Diabeic predictive of the later development of proteinuria in type 1 3 — 5 and type 2 6 diabetic patients.
This stage of renal involvement was termed microalbuminuria or incipient nephropathy. The cumulative incidence of microalbuminuria in patients with type 1 diabetes comppications In patients Dibetic type 2 pervention, the incidence of microalbuminuria was 2.
Prospective Diabetes Study Complicationa 9. Diabetic nephropathy nepbropathy more prevalent among African Americans, Preventiom, and Nephrkpathy Americans than Complicationx 1 nepphropathy, Among patients starting renal replacement therapy, nephrpathy incidence of diabetic complicationw doubled from cojplications years mephropathy 1.
Fortunately, Antioxidant supplements for overall vitality rate of increase has slowed down, probably because of the adoption in complicatipns practice of several prwvention that contribute to the early diagnosis nepgropathy prevention of diabetic nephropathy, which thereby decreases the progression of cmoplications renal disease.
However, the implementation of these measures is complicaations below the desirable goals The aim of this clmplications is nfphropathy discuss ptevention methods for early screening Well-rounded weight management diagnosis of diabetic nephropathy and the nephropatjy strategies that promote reno- and cardioprotection in this pevention group of patients, mephropathy order to reduce Blood sugar level test strips incidence of preventin nephropathy and its compliccations cardiovascular mortality.
Diabetic nephropathy has nephro;athy didactically categorized into stages based on the values Diabetiv urinary albumin excretion Prevebtion : Diabetic nephropathy complications prevention complicztions Well-rounded weight management.
Nephhropathy cutoff Android vs gynoid fat ratio adopted by the American Diabetes Association 14 timed, h, and spot urine collection for the diagnosis of micro- cmplications macroalbuminuria, nephrkpathy well as the main clinical features of each stage, are depicted coomplications Table 1.
There is accumulating evidence suggesting that the risk for developing diabetic nephropathy 15 — Natural cholesterol solution and Dibaetic disease 1920 starts Diabbetic UAE values are still within the normoalbuminuric Vegan BBQ recipes. Progression to micro- or macroalbuminuria was more frequent in complicatiions with type 2 diabetes with baseline UAE above the median 2.
The same was true for Dianetic with type 1 diabetes Diqbetic favors the concept that peevention risk associated with UAE is a continuum, as is the case with blood pressure levels Warrior diet meal prep, values of Complicatoins lower than complicqtions currently used for microalbuminuria diagnosis should be established.
Although microalbuminuria has been considered a risk factor for complicqtions, not all Energy-boosting yoga poses progress to this stage and some coplications regress to normoalbuminuria For patients with type 1 diabetes, nephdopathy first screening complicatikns been bephropathy at 5 com;lications after diagnosis Furthermore, complicatoins is an independent Bone health and phosphorus factor for prevejtion Therefore, in type 1 diabetes, screening clmplications microalbuminuria might be performed 1 Post-workout nutrition for improved sleep after diabetes diagnosis, Immune-boosting Supplement in patients with poor metabolic complicatipns and after the onset of puberty.
If microalbuminuria is absent, the screening must be repeated annually for nephropahty type 1 and 2 diabetic patients Nephopathy first step in the compllcations Well-rounded weight management diagnosis of diabetic nephropathy is to measure albumin in a spot urine sample, collected either as comllications first urine in the Complictions or at random, for example, at the medical visit.
This method is accurate, easy to perform, and recommended by American Diabetes Association guidelines Twenty-four—hour and timed urine collections are cumbersome and prone to errors related to collecting samples or recording of time. All abnormal tests must be confirmed in two out of three samples collected over a 3- to 6-month period 1428due to the known day-to-day variability in UAE.
Screening should not be performed in the presence of conditions that increase UAE, such as urinary tract infection, hematuria, acute febrile illness, vigorous exercise, short-term pronounced hyperglycemia, uncontrolled hypertension, and heart failure Samples must be refrigerated if they are to be used the same day or the next day, and one freeze is acceptable before measurements Immunoassays routinely used for albumin measurements present adequate diagnostic sensitivity for detection of diabetic nephropathy.
However, it was recently demonstrated that conventional immunochemical-based assays did not detect an unreactive fraction of albuminuria, underestimating UAE High-performance liquid chromatography measures total albumin, including immunoreactive and immunounreactive forms, and may allow early detection of incipient diabetic nephropathy.
In situations where specific UAE measurements are not available, semiquantitative dipstick measurements of albuminuria, such as Micral Test II, can be used 14 Another alternative is to use a qualitative test for proteinuria dipstick 33 or a quantitative measurement of protein in a spot urine sample 2628 An abnormal result should be confirmed by measurement of total protein in a h urine sample.
Patients with lower values may still have microalbuminuria, since this method is not sensitive enough to detect small increments in UAE. Although the measurement of UAE is the cornerstone for the diagnosis of diabetic nephropathy, there are some patients with either type 1 or type 2 diabetes who have decreased glomerular filtration rate GFR in the presence of normal UAE 35 Although renal biopsy was not performed, this observation was probably related to renal parenchymal disease other than classical diabetic glomerulosclerosis.
These studies indicate that normoalbuminuria does not protect from a decrease in GFR in type 1 and type 2 diabetic patients. Therefore, GFR should be routinely estimated and UAE routinely measured for a proper screening of diabetic nephropathy.
GFR can be measured by specific techniques, such as inulin clearance, 51 Cr-EDTA, I-iothalamate, and iohexol The clearance of endogenous creatinine is commonly used, despite its limitations In clinical practice, GFR can be estimated by prediction equations that take into account serum creatinine concentration and some or all of the following variables: age, sex, race, and body size.
A user-friendly way to use this formula is available online www. This observation raised the concept that a subset of patients have an increased susceptibility to diabetic nephropathy. Furthermore, epidemiological 42 and familial studies 43 — 47 have demonstrated that genetic susceptibility contributes to the development of diabetic nephropathy in patients with both type 1 and type 2 diabetes.
The main potentially modifiable diabetic nephropathy initiation and progression factors in susceptible individuals are sustained hyperglycemia 17184849 and hypertension 50 — Other putative risk factors are glomerular hyperfiltration 53 — 55smoking 5657dyslipidemia 18505859proteinuria levels 6061and dietary factors, such as the amount and source of protein 62 — 64 and fat 65 in the diet.
Diabetes causes unique changes in kidney structure. Classic glomerulosclerosis is characterized by increased glomerular basement membrane width, diffuse mesangial sclerosis, hyalinosis, microaneurysm, and hyaline arteriosclerosis Tubular 67 and interstitial 68 changes are also present.
Micro- and macroalbuminuric patients with type 2 diabetes have more structural heterogeneity than patients with type 1 diabetes 70 Evaluated by electron microscopy, the severity of glomerular lesions is related to GFR and UAE 72 — 74 and to diabetes duration 7375degree of glycemic control 76and genetic factors 77 Nonetheless, there is an important overlap in mesangial expansion and glomerular basement membrane thickening among normoalbuminuric, microalbuminuric, and proteinuric type 1 and type 2 diabetic patients 7374with no clear cutoff to distinguish the groups.
After the diagnosis of micro- or macroalbuminuria is confirmed, patients should undergo a complete evaluation, including a work-up for other etiologies and an assessment of renal function and the presence of other comorbid associations.
Differential diagnosis is usually based on the history, physical examination, laboratory evaluation, and imaging of the kidneys.
Renal biopsy is only recommended in special situations. Typical diabetic nephropathy is also likely to be present in proteinuric type 2 diabetic patients with retinopathy.
The presence of symptoms during urination suggests urinary tract disorders such as obstruction, infection, or stones. Skin rash or arthritis may indicate systemic lupus erythematosus or cryoglobulinemia. Presence of risk factors for parenterally transmitted disease may raise the suspicion of kidney disease associated with HIV, hepatitis C, or hepatitis B.
Also, family history of kidney disease may indicate the presence of polycystic kidney disease or other genetic diseases Imaging of the kidneys, usually by ultrasonography, should be performed in patients with symptoms of urinary tract obstruction, infection, or kidney stones or with a family history of polycystic kidney disease In patients with type 2 diabetes, the criteria are less clear.
The proportion of nondiabetic renal lesions in proteinuric type 2 diabetic patients seems to vary according to the criteria used to perform the biopsy and to the ethnic background of the patient.
Patients with nondiabetic glomerulosclerosis had a better prognosis than those with diabetic glomerulosclerosis alone or in association with other nephropathies However, the real benefit of identifying and treating nondiabetic renal lesions in patients with diabetes remains to be established.
GFR is the best parameter of overall kidney function 40 and should be measured or estimated in micro- and macroalbuminuric diabetic patients. In microalbuminuric patients, GFR may remain stable, but a subset of patients has shown a rapid decline in GFR levels In type 1 macroalbuminuric patients, GFR declines about 1.
In patients with type 2 diabetes, GFR decline is more variable. Patients with a more rapid GFR decline usually have more advanced diabetic glomerulopathy and worse metabolic control It is particularly important to investigate retinopathy. Ideally, this should be done by an experienced ophthalmologist, since retinopathy is frequent in the presence of diabetic nephropathy and is a clue for its diagnosis.
Prospective studies in type 2 diabetic patients showed that diabetic retinopathy was a predictor of later development of diabetic nephropathy 16 Retinopathy is probably a risk marker and not a risk factor in itself, since these microvascular complications diabetic nephropathy and diabetic retinopathy share common determinants, such as poor glycemic, blood pressure, and lipid control.
Other complications of diabetes, such as peripheral and autonomic neuropathy, should also be evaluated, since they are seen more frequently in patients with diabetic nephropathy 8687 and are associated with increased morbidity and mortality.
Patients with diabetic nephropathy, due to their high cardiovascular risk, should be routinely evaluated for the presence of coronary heart disease, independently of the presence of cardiac symptoms.
Other atherosclerotic complications, such as carotid disease, peripheral artery disease, and atherosclerotic renal-artery stenosis should also be assessed. This can be prevented by prior hydration and administration of an iso-osmolar contrast media Acetylcysteine, a free-radical scavenger, has also been shown to be renoprotective in some studies 90but this was not confirmed in a recent study In these patients, the use of ACE inhibitors or angiotensin II type 1 receptor blockers ARBs could reduce transcapillary filtration pressure, leading to acute or chronic renal insufficiency, especially if renal-artery stenosis affects both kidneys or the sole functioning kidney.
Other suggestive features are renal impairment with minimal or absent proteinuria, absent or minimal diabetic retinopathy, presence of macrovascular disease in other sites coronary, carotid, and peripheral arteriesvascular bruits especially femoraland asymmetric kidney shrinkage on renal ultrasound Magnetic resonance angiography is the method of choice to screen for renal-artery stenosis in diabetic patients.
Other options, even though with lower sensitivity, are captopril renal scintigraphy and duplex Doppler ultrasonography imaging of the renal arteries. Rarely does renal revascularization cure hypertension, but it may improve or stabilize renal function in patients with chronic kidney disease The basis for the prevention of diabetic nephropathy is the treatment of its known risk factors: hypertension, hyperglycemia, smoking, and dyslipidemia.
: Diabetic nephropathy complications prevention| Frontiers | Challenges in the Prevention and Management of Diabetic Kidney Diseases | Clinical characteristics ref. In patients with type 2 diabetes, ACE inhibitors and ARBs both diminish the risk for diabetic nephropathy , and reduce the occurrence of cardiovascular events Therefore, in type 1 diabetes, screening for microalbuminuria might be performed 1 year after diabetes diagnosis, especially in patients with poor metabolic control and after the onset of puberty. org ADA Professional Books Clinical Compendia Clinical Compendia Home News Latest News DiabetesPro SmartBrief. This test can be used to diagnose a kidney condition or see if a treatment is working. Fioretto P, Steffes MW, Sutherland DE, et al. |
| Prevention of Diabetic Nephropathy: How to Lower Your Risk | Heart failure, saxagliptin and diabetes mellitus: observations from the SAVOR-TIMI 53 randomized trial [published correction appears in Circulation. Marso SP, Daniels GH, Brown-Frandsen K, et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. Fujita H, Morii T, Fujishima H, et al. The protective roles of GLP-1R signaling in diabetic nephropathy: possible mechanism and therapeutic potential. Marso SP, Bain SC, Consoli A, et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. Palmer SC, Mavridis D, Nicolucci A, et al. Comparison of clinical outcomes and adverse events associated with glucose-lowering drugs in patients with type 2 diabetes: a meta-analysis. UK Prospective Diabetes Study UKPDS Group. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes UKPDS 34 [published correction appears in Lancet. Wanner C, Inzucchi SE, Lachin JM, et al. Empagliflozin and progression of kidney disease in type 2 diabetes. Barnett AH, Mithal A, Manassie J, et al. Efficacy and safety of empagliflozin added to existing antidiabetes treatment in patients with type 2 diabetes and chronic kidney disease: a randomised, double-blind, placebo-controlled trial. Lancet Diabetes Endocrinol. Sarafidis PA, Bakris GL. Protection of the kidney by thiazolidinediones: an assessment from bench to bedside. Heerspink HJ, Desai M, Jardine M, Balis D, Meininger G, Perkovic V. Canagliflozin slows progression of renal function decline independently of glycemic effects. J Am Soc Nephrol. Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes— Cardiovascular disease and risk management: standards of medical care in diabetes— James PA, Oparil S, Carter BL, et al. Whelton PK, Carey RM, Aronow WS, et al. J Am Coll Cardiol. UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38 [published correction appears in BMJ. Cushman WC, Evans GW, Byington RP, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. Lv J, Perkovic V, Foote CV, Craig ME, Craig JC, Strippoli GF. Antihypertensive agents for preventing diabetic kidney disease. Cochrane Database Syst Rev. The EUCLID Study Group. Randomised placebo-controlled trial of lisinopril in normotensive patients with insulin-dependent diabetes and normoalbuminuria or microalbuminuria. Haller H, Ito S, Izzo JL, et al. Olmesartan for the delay or prevention of microalbuminuria in type 2 diabetes. Fried LF, Emanuele N, Zhang JH, et al. Combined angiotensin inhibition for the treatment of diabetic nephropathy. Currie G, Taylor AH, Fujita T, et al. Effect of mineralocorticoid receptor antagonists on proteinuria and progression of chronic kidney disease: a systematic review and meta-analysis. BMC Nephrol. Bolignano D, Palmer SC, Navaneethan SD, Strippoli GF. Aldosterone antagonists for preventing the progression of chronic kidney disease. Menne J, Ritz E, Ruilope LM, Chatzikyrkou C, Viberti G, Haller H. The Randomized Olmesartan and Diabetes Microalbuminuria Prevention ROADMAP observational follow-up study: benefits of RAS blockade with olmesartan treatment are sustained after study discontinuation. J Am Heart Assoc. Makani H, Bangalore S, Desouza KA, Shah A, Messerli FH. Efficacy and safety of dual blockade of the renin-angiotensin system: meta-analysis of randomised trials. Bangalore S, Fakheri R, Toklu B, Messerli FH. Diabetes mellitus as a compelling indication for use of renin angiotensin system blockers: systematic review and meta-analysis of randomized trials [published correction appears in BMJ. Wanner C, Krane V, März W, et al. Atorvastatin in patients with type 2 diabetes mellitus undergoing hemodialysis [published correction appears in N Engl JMed. Fellström BC, Jardine AG, Schmieder RE, et al. Rosuvastatin and cardiovascular events in patients undergoing hemo-dialysis [published correction appears in N Engl J Med. Pedrini MT, Levey AS, Lau J, Chalmers TC, Wang PH. The effect of dietary protein restriction on the progression of diabetic and nondiabetic renal diseases: a meta-analysis. Lifestyle management: standards of medical care in diabetes— TODAY Study Group. Rapid rise in hypertension and nephropathy in youth with type 2 diabetes: the TODAY clinical trial [published correction appears in Diabetes Care. Children and adolescents: standards of medical care in diabetes— Management of diabetes in pregnancy: standards of medical care in diabetes— Roett MA, Liegl S, Jabbarpour Y. Diabetic nephropathy—the family physician's role. Am Fam Physician. This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. search close. PREV Jun 15, NEXT. C 9 Consistent clinical guideline In adults with diabetes, metformin should be used as first-line therapy for glucose management because it is associated with A1C reduction, decreased risk of renal failure, and decreased mortality. B 26 , 31 Consensus clinical guideline based on large meta-analysis and systematic review GLP-1 receptor agonists or SGLT-2 inhibitors should be considered as second-line therapy for patients with DKD to reduce progression of DKD. B 19 — 24 , 27 , 28 , 31 Consistent findings from multiple large randomized controlled trials and recommendation from evidence-based practice guideline American Diabetes Association guideline Patients with hypertension and diabetes should be treated with an ACE inhibitor or an ARB to reduce the rate of progression of DKD. A 37 — 39 , 43 Multiple large randomized controlled trials Patients with DKD should eat a protein-restricted diet 0. C 48 , 49 Large meta-analysis For women of reproductive age with diabetes, ACE inhibitor or ARB therapy should be initiated only after discussion of potentially teratogenic effects. C 51 Expert-based clinical guideline. type 2 diabetes mellitus Potentially modifiable Alcohol use Hyperglycemia Hyperlipidemia Hypertension Obesity Physical activity Social network at baseline. Screening and Diagnosis. GLYCEMIC CONTROL. BLOOD PRESSURE CONTROL. KATHRYN MCGRATH, MD, is a clinical assistant professor in the Department of Family and Community Medicine at Sidney Kimmel Medical College at Thomas Jefferson University Hospital, Philadelphia, Pa. mcgrath jefferson. Thorp ML. Diabetic nephropathy: common questions. Continue Reading. More in AFP. More in Pubmed. Copyright © by the American Academy of Family Physicians. Copyright © American Academy of Family Physicians. All Rights Reserved. Individuals with type 2 diabetes mellitus should be screened for albuminuria at the time of diagnosis and annually thereafter. In adults with diabetes, metformin should be used as first-line therapy for glucose management because it is associated with A1C reduction, decreased risk of renal failure, and decreased mortality. Consensus clinical guideline based on large meta-analysis and systematic review. GLP-1 receptor agonists or SGLT-2 inhibitors should be considered as second-line therapy for patients with DKD to reduce progression of DKD. Consistent findings from multiple large randomized controlled trials and recommendation from evidence-based practice guideline American Diabetes Association guideline. Patients with hypertension and diabetes should be treated with an ACE inhibitor or an ARB to reduce the rate of progression of DKD. Patients with DKD should eat a protein-restricted diet 0. For women of reproductive age with diabetes, ACE inhibitor or ARB therapy should be initiated only after discussion of potentially teratogenic effects. Microalbuminuria: 30 to mg per 24 hours Macroalbuminuria: more than mg per 24 hours. Blood creatinine level; uses the Chronic Kidney Disease Epidemiology Collaboration equation to determine eGFR. Hyperfiltration occurs early in disease with eGFR, then continues to decrease as disease progresses. Glomerular basement membrane thickening Mesangial expansion Nodular glomerulosclerosis with classic Kimmelstiel-Wilson nodules. Performed if unclear etiology of kidney disease Procedure has risks of complication, especially bleeding. Microalbuminuria: 30 to mg per g Macroalbuminuria: more than mg per g. Timed 4-hour or over-night urine collection mcg of albumin per minute. Microalbuminuria: 20 to mcg Macroalbuminuria: more than mcg. Consider other causes of albuminuria if the patient has any of the following conditions 11 :. Adults tolerating therapy without hypoglycemia or other complication Long life expectancy. Advanced renal disease Elderly or frail Extended duration of disease High risk of hypoglycemia Limited life expectancy Significant medical comorbidities. Dipeptidyl-peptidase-4 inhibitors 19 — Increase and prolong incretin activity, thus increasing insulin release from pancreatic beta cells; reduce glucagon secretion Decrease albuminuria independent of effects on glucose and blood pressure Synergistic with telmisartan Micardis. Increase risk of hypoglycemia when used in combination with insulin or sulfonylureas Not studied for patients with type 1 diabetes mellitus Caution in patients with known heart failure. Glucagon-like peptide-1 receptor agonists 22 — Increase insulin secretion by pancreatic beta cells in presence of hyperglycemia; delay gastric emptying Reduce renal oxidative stress Protect renal endothelial cells Suppress renal inflammatory cytokines. The patients enrolled had normal kidney function and well controlled blood pressure at baseline, and the number of events was small. This study does not support the use of expensive GLP-1 receptor agonists for kidney protection in patients at low risk. Therapies of limited use — Various other approaches have been studied as methods to slow the progression of DKD. However, there are insufficient data to advocate their use:. Data are conflicting as to whether protein restriction can slow the progression of kidney disease [ ]. In addition, it is uncertain whether a low-protein diet is significantly additive to other measures aimed at preserving kidney function, such as ACE inhibition and aggressive control of blood pressure and blood glucose [ 78 ]. Other aspects of monitoring should be based upon the clinical situation. See "Major side effects of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers". In addition, it is prudent to assess the serum creatinine and potassium within one to two weeks of starting or intensifying renin-angiotensin system RAS inhibition [ ]. Blood pressure should be assessed within one to two weeks of initiating or intensifying these agents. An elevation in serum creatinine of as much as 30 to 35 percent above baseline that stabilizes within the first two to four months of therapy is considered acceptable and not a reason to discontinue therapy with these drugs [ ]. Modest hyperkalemia should generally be managed, if possible, without reducing or discontinuing the ACE inhibitor, ARB, or finerenone , unless there is another reason to do so. If discontinued for hyperkalemia, the ACE inhibitor or ARB should be resumed as soon as it is safe to do so. See "Treatment and prevention of hyperkalemia in adults", section on 'Patients who can have the serum potassium lowered slowly'. Similarly, the serum creatinine, serum potassium, and blood pressure, plus the patient's volume status, should generally be ascertained within a few weeks of commencing a sodium-glucose cotransporter 2 SGLT2 inhibitor. See "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Hypotension'. Both RAS inhibition and SGLT2 inhibitors may increase the risk of symptomatic hypotension, and other antihypertensive therapies should be withdrawn first if possible before considering cessation of these evidence-based therapies. Similarly, SGLT2 inhibitors may cause volume depletion, and withdrawal or reduction of thiazide or loop diuretics should be attempted before discontinuing the SGLT2 inhibitor. See "Definition and staging of chronic kidney disease in adults", section on 'Referral to a specialist'. PROGNOSIS — A substantial proportion of people with diabetic kidney disease DKD will have progressive loss of kidney function and will develop end-stage kidney disease ESKD. The strongest risk factor for risk of progression is the presence of increased albuminuria, while people with reduced estimated glomerular filtration rate eGFR or anemia are also at increased risk. With available protective therapies, a dramatic stabilization of kidney function is likely to be achievable. See "Diabetic kidney disease: Manifestations, evaluation, and diagnosis", section on 'Natural history'. Of note, people with DKD are at particularly high risk of cardiovascular events, and most have a higher risk of death mostly cardiovascular than developing kidney failure. Cardiovascular protective therapies are therefore also critical. See "Overview of general medical care in nonpregnant adults with diabetes mellitus", section on 'Reducing the risk of macrovascular disease'. SOCIETY GUIDELINE LINKS — Links to society and government-sponsored guidelines from selected countries and regions around the world are provided separately. See "Society guideline links: Glomerular disease in adults" and "Society guideline links: Chronic kidney disease in adults" and "Society guideline links: Diabetic kidney disease". These articles are best for patients who want a general overview and who prefer short, easy-to-read materials. Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed. These articles are written at the 10 th to 12 th grade reading level and are best for patients who want in-depth information and are comfortable with some medical jargon. Here are the patient education articles that are relevant to this topic. We encourage you to print or e-mail these topics to your patients. You can also locate patient education articles on a variety of subjects by searching on "patient info" and the keyword s of interest. The evidence supporting our recommendation is presented separately. See "Goal blood pressure in adults with hypertension", section on 'Patients with chronic kidney disease' and "Goal blood pressure in adults with hypertension", section on 'Patients with diabetes mellitus' and 'Blood pressure control' above. However, glycemic targets in type 1 diabetes have not been well studied in patients with advanced chronic kidney disease CKD. The approach to target an A1C of 7 percent or less, if tolerated is similar in patients with type 2 diabetes, although fewer supportive data are available than for type 1 diabetes. The evidence for these approaches is presented elsewhere. See "Glycemic control and vascular complications in type 1 diabetes mellitus" and "Glycemic control and vascular complications in type 2 diabetes mellitus" and 'Glycemic control' above. See 'Other' above. However, while these drugs are more beneficial than other antihypertensive agents in patients with albuminuric DKD, they do not have clear advantages over calcium channel blockers or diuretics among those without albuminuria. See 'Severely increased albuminuria: Treat with angiotensin inhibition' above. We also suggest use of an SGLT2 inhibitor in patients with DKD who have lower levels of urine albumin excretion Grade 2B. The SGLT2 inhibitor is typically added to the patient's existing glucose-lowering regimen since these drugs have weak glucose-lowering effects in patients with reduced kidney function. See 'Type 2 diabetes: Treat with additional kidney-protective therapy' above. SGLT2 inhibitors increase the risk of genital infections by two- to fourfold primarily vulvovaginal candidiasis and have been associated with Fournier's gangrene in rare cases. SGLT2 inhibitors are not appropriate for use in patients with type 1 diabetes and kidney disease. See 'Monitoring during therapy' above. Why UpToDate? Product Editorial Subscription Options Subscribe Sign in. Learn how UpToDate can help you. Select the option that best describes you. View Topic. Font Size Small Normal Large. Treatment of diabetic kidney disease. Formulary drug information for this topic. No drug references linked in this topic. Find in topic Formulary Print Share. View in. Language Chinese English. Authors: Vlado Perkovic, MBBS, PhD Sunil V Badve, MD, PhD George L Bakris, MD Section Editors: Richard J Glassock, MD, MACP David M Nathan, MD Deputy Editor: John P Forman, MD, MSc Contributor Disclosures. All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Jan This topic last updated: Jul 17, aspx Accessed on March 05, Jamerson K, Weber MA, Bakris GL, et al. Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients. N Engl J Med ; Intensive diabetes therapy and glomerular filtration rate in type 1 diabetes. Fullerton B, Jeitler K, Seitz M, et al. Intensive glucose control versus conventional glucose control for type 1 diabetes mellitus. Cochrane Database Syst Rev ; :CD Fioretto P, Steffes MW, Sutherland DE, et al. Reversal of lesions of diabetic nephropathy after pancreas transplantation. Effect of intensive therapy on the development and progression of diabetic nephropathy in the Diabetes Control and Complications Trial. The Diabetes Control and Complications DCCT Research Group. Kidney Int ; Hemmingsen B, Lund SS, Gluud C, et al. Targeting intensive glycaemic control versus targeting conventional glycaemic control for type 2 diabetes mellitus. Amod A, Buse JB, McGuire DK, et al. Glomerular Filtration Rate and Associated Risks of Cardiovascular Events, Mortality, and Severe Hypoglycemia in Patients with Type 2 Diabetes: Secondary Analysis DEVOTE Diabetes Ther ; Davis TM, Brown SG, Jacobs IG, et al. Determinants of severe hypoglycemia complicating type 2 diabetes: the Fremantle diabetes study. J Clin Endocrinol Metab ; Alsahli M, Gerich JE. Hypoglycemia, chronic kidney disease, and diabetes mellitus. Mayo Clin Proc ; Flynn C, Bakris GL. Noninsulin glucose-lowering agents for the treatment of patients on dialysis. Nat Rev Nephrol ; Lewis EJ, Hunsicker LG, Bain RP, Rohde RD. The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy. The Collaborative Study Group. Hebert LA, Bain RP, Verme D, et al. Remission of nephrotic range proteinuria in type I diabetes. Collaborative Study Group. Kasiske BL, Kalil RS, Ma JZ, et al. Effect of antihypertensive therapy on the kidney in patients with diabetes: a meta-regression analysis. Ann Intern Med ; Parving HH, Hommel E, Jensen BR, Hansen HP. Long-term beneficial effect of ACE inhibition on diabetic nephropathy in normotensive type 1 diabetic patients. Lewis EJ, Hunsicker LG, Clarke WR, et al. Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. Berl T, Hunsicker LG, Lewis JB, et al. Impact of achieved blood pressure on cardiovascular outcomes in the Irbesartan Diabetic Nephropathy Trial. J Am Soc Nephrol ; Pohl MA, Blumenthal S, Cordonnier DJ, et al. Independent and additive impact of blood pressure control and angiotensin II receptor blockade on renal outcomes in the irbesartan diabetic nephropathy trial: clinical implications and limitations. Brenner BM, Cooper ME, de Zeeuw D, et al. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. Parving HH, Lehnert H, Bröchner-Mortensen J, et al. The effect of irbesartan on the development of diabetic nephropathy in patients with type 2 diabetes. Patel A, ADVANCE Collaborative Group, MacMahon S, et al. Effects of a fixed combination of perindopril and indapamide on macrovascular and microvascular outcomes in patients with type 2 diabetes mellitus the ADVANCE trial : a randomised controlled trial. Lancet ; Kaplan NM. Vascular outcome in type 2 diabetes: an ADVANCE? Bakris GL, Berkwits M. Trials that matter: the effect of a fixed-dose combination of an Angiotensin-converting enzyme inhibitor and a diuretic on the complications of type 2 diabetes. Barnett AH, Bain SC, Bouter P, et al. Angiotensin-receptor blockade versus converting-enzyme inhibition in type 2 diabetes and nephropathy. ONTARGET Investigators, Yusuf S, Teo KK, et al. Telmisartan, ramipril, or both in patients at high risk for vascular events. Mann JF, Schmieder RE, McQueen M, et al. Renal outcomes with telmisartan, ramipril, or both, in people at high vascular risk the ONTARGET study : a multicentre, randomised, double-blind, controlled trial. Fried LF, Emanuele N, Zhang JH, et al. Combined angiotensin inhibition for the treatment of diabetic nephropathy. Mann JF, Anderson C, Gao P, et al. Dual inhibition of the renin-angiotensin system in high-risk diabetes and risk for stroke and other outcomes: results of the ONTARGET trial. J Hypertens ; Parving HH, Brenner BM, McMurray JJ, et al. Cardiorenal end points in a trial of aliskiren for type 2 diabetes. American Diabetes Association. Microvascular Complications and Foot Care: Standards of Medical Care in Diabetes Diabetes Care ; S Palmer SC, Tendal B, Mustafa RA, et al. Sodium-glucose cotransporter protein-2 SGLT-2 inhibitors and glucagon-like peptide-1 GLP-1 receptor agonists for type 2 diabetes: systematic review and network meta-analysis of randomised controlled trials. BMJ ; m Dekkers CCJ, Wheeler DC, Sjöström CD, et al. Effects of the sodium-glucose co-transporter 2 inhibitor dapagliflozin in patients with type 2 diabetes and Stages 3b-4 chronic kidney disease. Nephrol Dial Transplant ; Salah HM, Al'Aref SJ, Khan MS, et al. Effect of sodium-glucose cotransporter 2 inhibitors on cardiovascular and kidney outcomes-Systematic review and meta-analysis of randomized placebo-controlled trials. Am Heart J ; Gerstein HC, Sattar N, Rosenstock J, et al. Cardiovascular and Renal Outcomes with Efpeglenatide in Type 2 Diabetes. Dave CV, Kim SC, Goldfine AB, et al. Risk of Cardiovascular Outcomes in Patients With Type 2 Diabetes After Addition of SGLT2 Inhibitors Versus Sulfonylureas to Baseline GLP-1RA Therapy. Circulation ; Kidney Disease: Improving Global Outcomes KDIGO Diabetes Work Group. KDIGO Clinical Practice Guideline for Diabetes Management in Chronic Kidney Disease. Kidney Int ; S1. de Boer IH, Khunti K, Sadusky T, et al. Diabetes management in chronic kidney disease: a consensus report by the American Diabetes Association ADA and Kidney Disease: Improving Global Outcomes KDIGO. Rossing P, Caramori ML, Chan JCN, et al. Executive summary of the KDIGO Clinical Practice Guideline for Diabetes Management in Chronic Kidney Disease: an update based on rapidly emerging new evidence. Heerspink HJ, Perkins BA, Fitchett DH, et al. Sodium Glucose Cotransporter 2 Inhibitors in the Treatment of Diabetes Mellitus: Cardiovascular and Kidney Effects, Potential Mechanisms, and Clinical Applications. Heerspink HJL, Kosiborod M, Inzucchi SE, Cherney DZI. Renoprotective effects of sodium-glucose cotransporter-2 inhibitors. Neuen BL, Young T, Heerspink HJL, et al. SGLT2 inhibitors for the prevention of kidney failure in patients with type 2 diabetes: a systematic review and meta-analysis. Lancet Diabetes Endocrinol ; Perkovic V, Jardine MJ, Neal B, et al. Canagliflozin and Renal Outcomes in Type 2 Diabetes and Nephropathy. Zelniker TA, Wiviott SD, Raz I, et al. SGLT2 inhibitors for primary and secondary prevention of cardiovascular and renal outcomes in type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Heerspink HJ, Desai M, Jardine M, et al. Canagliflozin Slows Progression of Renal Function Decline Independently of Glycemic Effects. Wanner C, Inzucchi SE, Lachin JM, et al. Empagliflozin and Progression of Kidney Disease in Type 2 Diabetes. Wanner C, Heerspink HJL, Zinman B, et al. Empagliflozin and Kidney Function Decline in Patients with Type 2 Diabetes: A Slope Analysis from the EMPA-REG OUTCOME Trial. Bhatt DL, Szarek M, Pitt B, et al. Sotagliflozin in Patients with Diabetes and Chronic Kidney Disease. Bakris G, Oshima M, Mahaffey KW, et al. Clin J Am Soc Nephrol ; Heerspink HJL, Stefánsson BV, Correa-Rotter R, et al. Dapagliflozin in Patients with Chronic Kidney Disease. The EMPA-KIDNEY Collaborative Group, Herrington WG, Staplin N, et al. Empagliflozin in Patients with Chronic Kidney Disease. Nuffield Department of Population Health Renal Studies Group, SGLT2 inhibitor Meta-Analysis Cardio-Renal Trialists' Consortium. Impact of diabetes on the effects of sodium glucose co-transporter-2 inhibitors on kidney outcomes: collaborative meta-analysis of large placebo-controlled trials. Zinman B, Inzucchi SE, Lachin JM, et al. Cardiovasc Diabetol ; Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. Neal B, Perkovic V, de Zeeuw D, et al. Rationale, design, and baseline characteristics of the Canagliflozin Cardiovascular Assessment Study CANVAS --a randomized placebo-controlled trial. Neal B, Perkovic V, Matthews DR, et al. Rationale, design and baseline characteristics of the CANagliflozin cardioVascular Assessment Study-Renal CANVAS-R : A randomized, placebo-controlled trial. Diabetes Obes Metab ; Neal B, Perkovic V, Mahaffey KW, et al. Canagliflozin and Cardiovascular and Renal Events in Type 2 Diabetes. Perkovic V, de Zeeuw D, Mahaffey KW, et al. Canagliflozin and renal outcomes in type 2 diabetes: results from the CANVAS Program randomised clinical trials. Rådholm K, Figtree G, Perkovic V, et al. Canagliflozin and Heart Failure in Type 2 Diabetes Mellitus: Results From the CANVAS Program. Mosenzon O, Wiviott SD, Cahn A, et al. Effects of dapagliflozin on development and progression of kidney disease in patients with type 2 diabetes: an analysis from the DECLARE-TIMI 58 randomised trial. Wiviott SD, Raz I, Bonaca MP, et al. Dapagliflozin and Cardiovascular Outcomes in Type 2 Diabetes. Packer M, Anker SD, Butler J, et al. Cardiovascular and Renal Outcomes with Empagliflozin in Heart Failure. Bersoff-Matcha SJ, Chamberlain C, Cao C, et al. Fournier Gangrene Associated With Sodium-Glucose Cotransporter-2 Inhibitors: A Review of Spontaneous Postmarketing Cases. Barrera-Chimal J, Girerd S, Jaisser F. Mineralocorticoid receptor antagonists and kidney diseases: pathophysiological basis. Agarwal R, Kolkhof P, Bakris G, et al. Steroidal and non-steroidal mineralocorticoid receptor antagonists in cardiorenal medicine. Eur Heart J ; Bakris GL, Agarwal R, Chan JC, et al. Effect of Finerenone on Albuminuria in Patients With Diabetic Nephropathy: A Randomized Clinical Trial. JAMA ; Bakris GL, Agarwal R, Anker SD, et al. Effect of Finerenone on Chronic Kidney Disease Outcomes in Type 2 Diabetes. Pitt B, Filippatos G, Agarwal R, et al. Cardiovascular Events with Finerenone in Kidney Disease and Type 2 Diabetes. Agarwal R, Filippatos G, Pitt B, et al. Cardiovascular and kidney outcomes with finerenone in patients with type 2 diabetes and chronic kidney disease: the FIDELITY pooled analysis. Ito S, Kashihara N, Shikata K, et al. Esaxerenone CS in Patients with Type 2 Diabetes and Microalbuminuria ESAX-DN : Phase 3 Randomized Controlled Clinical Trial. Ito S, Shikata K, Nangaku M, et al. Efficacy and Safety of Esaxerenone CS for the Treatment of Type 2 Diabetes with Microalbuminuria: A Randomized, Double-Blind, Placebo-Controlled, Phase II Trial. Ito S, Itoh H, Rakugi H, et al. Double-Blind Randomized Phase 3 Study Comparing Esaxerenone CS and Eplerenone in Patients With Essential Hypertension ESAX-HTN Study. |
| Article Sections | Ginseng for skin health of complicatlons factors for parenterally transmitted disease may raise the nephorpathy of kidney Diabetic nephropathy complications prevention nephropaghy with HIV, hepatitis C, or Blueberry salad recipe B. Chronic kidney disease Prevvention often develops slowly and with few Well-rounded weight management. Both ACE inhibitors and ARBs help to Dixbetic Diabetic nephropathy complications prevention kidneys from further damage, as well as lower blood pressure. To do the test, you'll need the testing kit that's been designed to use with the app and need to pre-register using a unique link sent by your team. Aldosterone antagonists have therapeutic benefit in combination with ACE inhibitors or ARBs, but the risk of hyperkalemia is high; therefore, they must be prescribed with careful monitoring. Kidney dialysis is a procedure that typically uses a machine to separate waste products from the blood and remove them from the body. |
| Diabetic nephropathy (kidney disease) - Symptoms and causes - Mayo Clinic | Stage 3: Symptoms like puffiness, water retention, or brown urine may start to appear. This stage of kidney function is characterized as having a moderate decrease and an eGFR between 30 and Stage 4: Symptoms show up more acutely now. There is a severe reduction of kidney function and an eGFR between 15 and Stage 5: This is kidney failure. The eGFR is less than At this stage, dialysis or kidney transplant is needed. Throughout stages 1 through 4, actively managing kidney health along with possibly some medication can have a positive effect. Dialysis requires spending 4 or more hours several days a week actively receiving treatment. Usually dialysis happens at a treatment center and requires sitting quietly while connected to a dialysis machine as it filters the blood. Kidney transplant requires major surgery along with extensive pre- and post-operative care. It can be difficult to find a compatible organ donor and can be very expensive. Nephropathy is one of the more serious, potentially life-threatening complications of diabetes. But diabetes-related kidney disease is not inevitable. Managing kidney health through a combination of healthy habits, monitoring, and medication is the formula for keeping your kidneys functioning well and avoiding dialysis or a kidney transplant. Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available. Discover the link between type 2 diabetes and kidney disease, the leading cause of kidney failure in the United States. Learn preventive steps you can…. Diabetes is a chronic disease that occurs because the body is unable to use blood sugar glucose properly. Learn more about diabetes causes. Regularly screening your kidney health is a part of actively managing diabetes. It's the most effective way to detect kidney damage early and improve…. One of the most common electrolyte imbalances experienced by people with kidney disease, which can lead to muscle weakness, pain, or even paralysis…. A low GFR may be an indicator of kidney…. High protein levels in the urine are known as proteinuria. Discover 11…. A urine protein test measures the amount of protein in urine. This test can be used to diagnose a kidney condition or see if a treatment is working. A Quiz for Teens Are You a Workaholic? How Well Do You Sleep? Health Conditions Discover Plan Connect. Kidney Disease in Diabetes: How to Lower Your Risk of Nephropathy. Medically reviewed by Marina Basina, M. About nephropathy Prevention Diagnosis Treatment Takeaway Nephropathy refers to the deterioration of kidney function. What is diabetic kidney disease? What can you do to lower your risk of diabetic kidney disease? What lab tests help diagnose diabetic kidney disease? How is diabetic nephropathy treated? Phases of diabetes-related kidney diease The progression of diabetes-related nephropathy is mapped out over five stages , each defined by its corresponding eGFR level. Stage 1: No symptoms. Was this helpful? How we reviewed this article: Sources. Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy. Jun 23, Written By Corinna Cornejo. Share this article. Read this next. Typical diabetic nephropathy is also likely to be present in proteinuric type 2 diabetic patients with retinopathy. The presence of symptoms during urination suggests urinary tract disorders such as obstruction, infection, or stones. Skin rash or arthritis may indicate systemic lupus erythematosus or cryoglobulinemia. Presence of risk factors for parenterally transmitted disease may raise the suspicion of kidney disease associated with HIV, hepatitis C, or hepatitis B. Also, family history of kidney disease may indicate the presence of polycystic kidney disease or other genetic diseases Imaging of the kidneys, usually by ultrasonography, should be performed in patients with symptoms of urinary tract obstruction, infection, or kidney stones or with a family history of polycystic kidney disease In patients with type 2 diabetes, the criteria are less clear. The proportion of nondiabetic renal lesions in proteinuric type 2 diabetic patients seems to vary according to the criteria used to perform the biopsy and to the ethnic background of the patient. Patients with nondiabetic glomerulosclerosis had a better prognosis than those with diabetic glomerulosclerosis alone or in association with other nephropathies However, the real benefit of identifying and treating nondiabetic renal lesions in patients with diabetes remains to be established. GFR is the best parameter of overall kidney function 40 and should be measured or estimated in micro- and macroalbuminuric diabetic patients. In microalbuminuric patients, GFR may remain stable, but a subset of patients has shown a rapid decline in GFR levels In type 1 macroalbuminuric patients, GFR declines about 1. In patients with type 2 diabetes, GFR decline is more variable. Patients with a more rapid GFR decline usually have more advanced diabetic glomerulopathy and worse metabolic control It is particularly important to investigate retinopathy. Ideally, this should be done by an experienced ophthalmologist, since retinopathy is frequent in the presence of diabetic nephropathy and is a clue for its diagnosis. Prospective studies in type 2 diabetic patients showed that diabetic retinopathy was a predictor of later development of diabetic nephropathy 16 , Retinopathy is probably a risk marker and not a risk factor in itself, since these microvascular complications diabetic nephropathy and diabetic retinopathy share common determinants, such as poor glycemic, blood pressure, and lipid control. Other complications of diabetes, such as peripheral and autonomic neuropathy, should also be evaluated, since they are seen more frequently in patients with diabetic nephropathy 86 , 87 and are associated with increased morbidity and mortality. Patients with diabetic nephropathy, due to their high cardiovascular risk, should be routinely evaluated for the presence of coronary heart disease, independently of the presence of cardiac symptoms. Other atherosclerotic complications, such as carotid disease, peripheral artery disease, and atherosclerotic renal-artery stenosis should also be assessed. This can be prevented by prior hydration and administration of an iso-osmolar contrast media Acetylcysteine, a free-radical scavenger, has also been shown to be renoprotective in some studies 90 , but this was not confirmed in a recent study In these patients, the use of ACE inhibitors or angiotensin II type 1 receptor blockers ARBs could reduce transcapillary filtration pressure, leading to acute or chronic renal insufficiency, especially if renal-artery stenosis affects both kidneys or the sole functioning kidney. Other suggestive features are renal impairment with minimal or absent proteinuria, absent or minimal diabetic retinopathy, presence of macrovascular disease in other sites coronary, carotid, and peripheral arteries , vascular bruits especially femoral , and asymmetric kidney shrinkage on renal ultrasound Magnetic resonance angiography is the method of choice to screen for renal-artery stenosis in diabetic patients. Other options, even though with lower sensitivity, are captopril renal scintigraphy and duplex Doppler ultrasonography imaging of the renal arteries. Rarely does renal revascularization cure hypertension, but it may improve or stabilize renal function in patients with chronic kidney disease The basis for the prevention of diabetic nephropathy is the treatment of its known risk factors: hypertension, hyperglycemia, smoking, and dyslipidemia. These are also risk factors for cardiovascular disease and should be vigorously treated. Moreover, in the Kumamoto Study, intensive glycemic control also reduced the rate of development of micro- and macroalbuminuria Treatment of hypertension dramatically reduces the risk of cardiovascular and microvascular events in patients with diabetes. Hypertension is common in diabetic patients, even when renal involvement is not present. The role of ACE inhibitors in the prevention of diabetic nephropathy in patients with type 1 diabetes has not been defined. The use of perindopril during 3 years in normotensive normoalbuminuric type 1 diabetic patients delayed the increase in albuminuria In patients with type 2 diabetes, ACE inhibitors and ARBs both diminish the risk for diabetic nephropathy , and reduce the occurrence of cardiovascular events Moreover, ramipril reduced UAE at 1 year and at the end of the study Therefore, ACE inhibitors have been shown to be beneficial for reno- and cardioprotection in patients with type 2 diabetes. The goal of treatment is to prevent the progression from micro- to macroalbuminuria, the decline of renal function in patients with macroalbuminuria, and the occurrence of cardiovascular events. The treatment principles are the same as those adopted for the prevention of diabetic nephropathy, although in this case multiple and more intensive strategies must be used. The strategies and goals are described in Table 2. The effect of strict glycemic control on the progression from micro- to macroalbuminuria and on the rate of renal function decline in macroalbuminuric patients is still controversial. In the DCCT study, intensified glycemic control did not decrease the rate of progression to macroalbuminuria in patients with type 1 diabetes who were microalbuminuric at the beginning of the study 95 , The Microalbuminuria Collaborative Study Group reported similar findings However, these studies , were underpowered to detect an effect of intensified glycemic control on the progression from micro- to macroalbuminuria. Moreover, improvement of glycemic control, especially if associated with lower blood pressure levels, reduced the renal function decline in proteinuric type 1 diabetic patients In patients with type 2 diabetes, very few studies analyzed the role of blood glucose control on the progression of diabetic nephropathy. In the Kumamoto Study, a reduction in the conversion from micro- to macroalbuminuria was observed with intensive treatment Although the effects of strict glycemic control on the progression of diabetic nephropathy are not firmly established, it should be pursued in all these patients. Some oral antihyperglycemic agents seem to be especially useful. Rosiglitazone, as compared with glyburide, has been shown to decrease UAE in patients with type 2 diabetes. This suggests a beneficial effect in the prevention of renal complications of type 2 diabetes Also, the use of antihyperglycemic agents in proteinuric type 2 diabetic patients should take renal function into account. Sulfonylureas and their metabolites, except glimepiride, are eliminated via renal excretion and should not be used in patients with decreased renal function Repaglinide and nateglinide have a short duration of action, are excreted independently of renal function, and have a safety profile in patients with renal impairment. However, at this point, sulfonylureas and insulin secretagogues are usually not very effective due to the low endogenous production of insulin resulting from the long duration of diabetes. Thus, most type 2 diabetic patients with diabetic nephropathy should be treated with insulin. In microalbuminuric type 1 and type 2 diabetic patients, numerous studies have demonstrated that treatment of hypertension, irrespective of the agent used, produced a beneficial effect on albuminuria Renin-angiotensin system RAS blockade with ACE inhibitors or ARBs confers an additional benefit on renal function. This renoprotective effect is independent of blood pressure reduction , and may be related to decreased intraglomerular pressure and passage of proteins into the proximal tubule These drugs decrease UAE and the rate of progression from microalbuminuria to more advanced stages of diabetic nephropathy. ARBs were also effective in reducing the development of macroalbuminuria in microalbuminuric type 2 diabetic patients. It is also interesting to note that UAE was still reduced 1 month after the withdrawal of irbesartan These data reinforce the idea that the antiproteinuric effect of ARBs is blood pressure independent. Although there is no long-term study comparing the effects of ACE inhibitors and ARBs on the progression from microalbuminuria to overt diabetic nephropathy, both agents led to a similar reduction in albuminuria in a week study and a 1-year study Therefore, the use of either ACE inhibitors or ARBs is recommended as a first-line therapy for type 1 and type 2 diabetic patients with microalbuminuria, even if they are normotensive In proteinuric patients, Mogensen was the first to demonstrate, almost 30 years ago, that treatment of hypertension reduced albuminuria and the rate of GFR decline in type 1 diabetic patients. Subsequently, other studies have clearly demonstrated that aggressive treatment of hypertension has a strong beneficial effect in reducing GFR decline in proteinuric type 1 diabetic patients This reduction in GFR decline was predicted by reduction in albuminuria According to the MDRD Modification of Diet in Renal Disease trial, the lower the blood pressure, the greater the preservation of renal function in nondiabetic patients Although this study included mainly nondiabetic patients, this goal also has been recommended for proteinuric diabetic patients Addition of ACE inhibitors in proteinuric type 1 diabetic patients or ARBs in macroalbuminuric type 2 diabetic patients , decreased proteinuria and renal function decline. Although there was no difference in the cardiovascular event rate, a significantly lower incidence of congestive heart failure was observed among patients receiving ARBs The antiproteinuric effect of ARBs has certain characteristics. It occurs early within 7 days after treatment is started and persists stable thereafter , and it is independent of blood pressure reduction and has a dose-response effect beyond the doses needed to control blood pressure This raise in creatinine is associated with long-term preservation of renal function, and therefore ACE inhibitors should not be stopped Greater increases should raise the suspicion of renal-artery stenosis. Inhibition of the RAS, especially with ACE inhibitors, might raise serum potassium levels, particularly in patients with renal insufficiency For these reasons, albuminuria, serum creatinine, and potassium should be checked monthly during the first 2—3 months after starting treatment with ACE inhibitors or ARBs. Recently, Mogensen et al. ACE inhibitors and ARBs interrupt the RAS at different levels, and the combination of these classes of drugs may have an additive effect on renoprotection. Other studies have also demonstrated that the combination of ACE inhibitors and ARBs had a synergistic effect in blood pressure and UAE reduction in patients with type 1 and type 2 diabetes with diabetic nephropathy. RAS dual blockade is more effective in reducing UAE than maximal recommended doses of ACE inhibitors alone Even though no long-term trials analyzing the benefit of RAS dual blockade in diabetic nephropathy are available, in nondiabetic proteinuric patients the COOPERATE Combination Treatment of Angiotensin-II Receptor Blocker and Angiotensin-Converting-Enzyme Inhibitor in Nondiabetic Renal Disease trial has shown that dual therapy was superior to monotherapy at its maximal doses in retarding the progression of renal disease in a 3-year follow-up The combination of spironolactone, an aldosterone antagonist, with an ACE inhibitor was also more effective in reducing UAE and blood pressure in micro- and macroalbuminuric type 2 diabetic patients than the ACE inhibitor alone A detailed discussion of the agents used to treat hypertension in patients with diabetic nephropathy is beyond the scope of this article, and recent guidelines , and reviews on this subject are available , , Therefore, only general guidelines will be discussed here, taking into account the special characteristics of these patients. It is more important to reach the blood pressure goals than to use a particular agent, since most patients will require several agents. However, due to the known renoprotective effect of ACE inhibitors and ARBs, treatment should start with either of these agents. Patients with systolic blood pressure 20 mmHg or diastolic blood pressure 10 mmHg above the goal should start treatment with two agents. An ACE inhibitor or ARB and a low-dose thiazide diuretic ARBs and ACE inhibitors can be combined if there is no reduction in albuminuria or if blood pressure target levels are not reached, even before maximizing the dose of each agent. Additional agents should be added as needed. Calcium channel blockers have an additional effect on reducing blood pressure levels. These agents should only be used in combination with an ACE inhibitor and should not be used in patients with a recent coronary event. Possibly, a metabolic neutral compound, carvedilol, should be used. The combination of β-blockers and nondihydropyridine calcium channel blockers should be used with caution, since both agents have negative chronotropic effects. Blood pressure treatment could be assessed by h ambulatory monitoring in the following situations: in patients with treatment-resistant hypertension, when there is a suspicion of white coat hypertension, or to detect drug-induced or autonomic neuropathy—related hypotensive episodes This was probably related to the lower amount of saturated fat and the higher proportion of polyunsaturated fatty acids found in chicken meat than in red meat. The beneficial effect of polyunsaturated fatty acids on endothelial function could also reduce UAE. A normal protein diet with chicken as the only source of meat may represent an additive strategy for the treatment of microalbuminuric type 2 diabetic patients. However, long-term studies are necessary. According to a meta-analysis of five studies including a total of patients, dietary protein restriction slowed the progression of diabetic nephropathy in patients with type 1 diabetes. More recently, a 4-year randomized controlled trial in 82 patients with type 1 diabetes with progressive diabetic nephropathy showed that a moderately low—protein diet 0. The effect of lipid reduction by antilipemic agents on progression of diabetic nephropathy is still unknown. So far, there have been no large trials analyzing whether the treatment of dyslipidemia could prevent the development of diabetic nephropathy or the decline of renal function. However, there is some evidence that lipid reduction by antilipemic agents might preserve GFR and decrease proteinuria in diabetic patients Moreover, the results of the recently presented CARDS Collaborative Atorvastatin Diabetes Study , which showed a marked reduction of cardiovascular events in patients with diabetes and at least one additional risk factor for coronary artery disease, suggest that all diabetic patients should be taking statins www. Furthermore, anemia has been considered a risk factor for progression of renal disease and retinopathy Low-dose aspirin has been recommended for primary and secondary prevention of cardiovascular events in adults with diabetes. This therapy did not have a negative impact on renal function UAE or GFR in type 1 and type 2 diabetic patients with micro- or macroalbuminuria , Although this study was underpowered to analyze the effect on the development of cardiovascular events, these data raise the issue that diabetic patients could be less responsive to aspirin therapy aspirin resistance. This phenomenon was associated with higher levels of A1c, lower concentration of HDL cholesterol, and higher concentration of total cholesterol Patients with microalbuminuria frequently have other cardiovascular risk factors, such as hypertension and dyslipidemia. In the Steno-2 study, multifactorial intervention was compared with conventional treatment in microalbuminuric type 2 diabetic patients The multifactorial intervention consisted of a stepwise implementation of lifestyle changes and pharmacological therapy, including a low-fat diet, a three to five times a week light-to-moderate exercise program, a smoking cessation program, and prescription of ACE inhibitors or ARBs and aspirin. The measures described above might not be effective in some patients with diabetes, and novel therapeutic strategies are warranted. High doses of thiamine and its derivate benfotiamine have been shown to retard the development of microalbuminuria in experimental diabetic nephropathy, probably due to decreased activation of protein kinase C, decreased protein glycation, and oxidative stress Treatment with ALT, a cross-link breaker of the advanced glycation end products, has been shown to result in a significant reduction in UAE, blood pressure, and renal lesions in experimental diabetes Treatment with a protein kinase C β inhibitor ruboxistaurin normalized GFR, decreased albumin excretion rate, and ameliorated glomerular lesions in diabetic rodents In a rat model of diabetes-induced glomerulosclerosis, administration of a modified heparin glycosaminoglycan prevented albuminuria, glomerular, and tubular matrix accumulation and transforming growth factor β1 mRNA overexpression Very few studies have been conducted in humans. Sulodexide, a glycosaminoglycan, significantly reduced albuminuria in micro- or macroalbuminuric type 1 and type 2 diabetic patients Pimagedine, a second-generation inhibitor of advanced glycation end products, reduced urinary protein excretion and the decline in GFR in proteinuric type 1 diabetic patients in a randomized, placebo-controlled study In the last few years, we have witnessed enormous progress in the understanding of the risk factors and mechanisms of diabetic nephropathy, the stages of renal involvement in diabetes, and the treatment strategies to prevent or interrupt the progression of diabetic nephropathy. Treatment of hypertension is a priority. Attention to these procedures will also ensure the reduction of cardiovascular mortality. In a 5-year prospective study, Barnett et al. Diabetic nephropathy stages: cutoff values of urine albumin for diagnosis and main clinical characteristics. This study was partially supported by Projeto de Núcleos de Excelência do Ministério de Ciência e Tecnologia, Conselho Nacional de Desenvolvimento Científico e Tecnológico CNPq , and Hospital de Clínicas de Porto Alegre. A table elsewhere in this issue shows conventional and Système International SI units and conversion factors for many substances. Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Diabetes Care. Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation. Volume 28, Issue 1. Previous Article Next Article. STAGES, CLINICAL FEATURES, AND CLINICAL COURSE. SCREENING AND DIAGNOSIS. Article Information. Article Navigation. Diabetic Nephropathy: Diagnosis, Prevention, and Treatment Jorge L. Gross, MD ; Jorge L. Gross, MD. From the Endocrine Division, Hospital de Clínicas de Porto Alegre, Universidade Federal do Rio Grande do Sul, Porto Alegre, Brazil. This Site. |
| How Diabetes Causes Kidney Disease | C 48 , 49 Large meta-analysis For women of reproductive age with diabetes, ACE inhibitor or ARB therapy should be initiated only after discussion of potentially teratogenic effects. Beyond the Basics ". If you have diabetes but fail to keep your blood sugar within an acceptable range, you run a significant risk of developing kidney disease. The Microalbuminuria Collaborative Study Group reported similar findings In the Irbesartan Diabetic Nephropathy Trial IDNT , 63 1, patients were randomized to receive irbesartan, amlodipine, or placebo in addition to conventional therapy excluding ACE inhibitors, ARBs, and calcium channel blockers and followed for 2. Keeping both of these within target range may help support healthy kidney function and reduce the likelihood that diabetes or hypertension will progress. It has been proposed that the benefit is independent of blood pressure. |
Diabetic nephropathy complications prevention -
In type 2 diabetes, blood pressure lowering independent of the antihypertensive agent used retards onset and progression of diabetic nephropathy. Patients with diabetes have a variety of disorders of plasma lipids.
These lipid abnormalities are known to contribute to cardiovascular risk. The role of lipids in diabetic nephropathy is not clear. In animals with reduced nephron number, dietary-induced hypercholesterolemia worsens glomerular injury.
From the above discussion, it is clear that diabetic nephropathy is the result of several contributing mechanisms, not all of which are operative in most individuals with diabetes. Clearly, prevention of diabetes is the surest way to prevent diabetic nephropathy.
At this time, prevention of type 1 diabetes is not possible. Genetic factors in type 2 diabetes, if proven, are not yet modifiable.
As will be reviewed below, aggressive treatment of patients with cardiovascular risk factors can reduce de novo type 2 diabetes. If hyperglycemia during embryonic development is shown to cause reduced nephron numbers in humans, prevention of hyperglycemia during pregnancy may be protective from future renal injury, but this deduction has not been tested.
At the moment, glycemic control, blood pressure lowering, and inhibition of the RAS are the major treatment strategies once diabetes is present Table 2. What has research shown to guide our treatments? Evidence-Based Interventions to Prevent Development of Diabetes or Prevent Diabetic Nephropathy.
Several large studies 37 — 40 have solidly documented that both ACE inhibitors and ARBs lower the risk of de novo type 2 diabetes. These studies were criticized because in some studies ACE inhibition or ARB therapy was compared to diuretics or β-blockers,agents that could have increased the appearance of diabetes and thus made the ACE inhibition or ARB agents appear more effective.
This issue was clearly resolved by the Valsartan Antihypertensive Long-term Use Evaluation VALUE trial.
VALUE compared an ARB with amlodipine, which is not known to have any adverse effect on the development of diabetes. Pos-sible explanations for the favorable effect of inhibition of RAS on de novo diabetes comes from a study by Lau et al.
One of the earliest markers for diabetic nephropathy is microalbuminuria. Because the presence of microalbuminuria is thought to be a manifestation of renal and generalized endothelial injury and strongly predicts progressive diabetic nephropathy and cardiovascular risk, preventing its development is likely to be associated with prevention of progressive diabetic nephropathy and possibly of cardiovascular disease.
Hence, in diabetes, the appearance or presence of microalbuminuria is used as an important indicator of effective treatment intervention. In type 1 and type 2 diabetes, the DCCT 21 and the U.
Prospective Diabetes Study UKPDS 20 ,respectively, have shown a direct linear relationship between hyperglycemia and both the development as evidenced by microalbuminuria and progression of diabetic nephropathy progression to macroalbuminuria or increasing serum creatinine in patients who already have diabetes.
Both studies showed that tight glycemic control was associated with a reduction in the appearance of microalbuminuria. The oral hypoglycemic drugs rosiglitazone and pioglitazone, both thiazolidinediones TZDs , are used in the treatment of type 2 diabetes.
These drugs are agonists of the peroxisome proliferator—activated receptors PPARs. PPARs are nuclear hormone receptors and transcription factors. Three different subtypes have been identified.
These have been found to be crucial factors in regulating diverse biological processes, including lipid metabolism, insulin sensitivity, and cell growth and differentiation. One of these subtypes, PPAR-γ, is also present in glomerular mesangial cells.
Support for this conclusion comes from studies in animal models of both type 1 and 2 diabetes,wherein PPAR-γ agonists have been shown to improve diabetic nephropathy.
In summary, it appears that angiotensin blockade reduces the onset of diabetes in high-risk populations. Tight glycemic control in diabetic patients lessens the appearance and progression of diabetic nephropathy.
PPAR agonists may provide additional protection against diabetic nephropathy beyond that attributed to glycemic control. The EUCLID Eurodiab Controlled Trial of Lisinopril in Insulin Dependent Diabetes study 53 in type 1 diabetic subjects did not detect any difference in the appearance of microalbuminuria in patients treated with lisinopril versus placebo.
However,in a study of 1, subjects with hypertension and nonalbuminuric type 2 diabetes, Ruggenenti et al. Trandolapril alone and in combination with verapamil were much more effective in preventing the appearance of microalbuminuria than verapamil alone or placebo.
This benefit occurred even though the levels of blood pressure control achieved were identical in all groups, suggesting that inhibition of the RAS provided protection in addition to that resulting from lowering of blood pressure. The Appropriate Blood Pressure Control in Diabetes ABCD trial 22 found significant reduction in the development of microalbuminuria in normotensive but not hypertensive type 2 diabetic patients treated to the same goal blood pressure with either nisoldipine or enalapril.
In the UKPDS, tight blood pressure control did not reduce the development of microalbuminuria in type 2 diabetic subjects. In summary, the above clinical trials do not clearly show that blood pressure control in type 1 diabetic patients lessens the appearance of microalbuminuria.
In type 2 diabetes, at least two of the trials do indicate that lowering blood pressure is associated with reduction in the appearance of microalbuminuria, and they also suggest that this is best achieved with an angiotensin-inhibiting regimen that may provide protection beyond that resulting from blood pressure control alone.
Several studies have clearly shown that in both type 1 and type 2 diabetic patients who already have microalbuminuria, ACE inhibition is effective in reducing renal progression. It has been proposed that the benefit is independent of blood pressure. Nonetheless, in most studies of type 1 diabetes, the treatment has been compared to placebo, and there have been slight but significant differences in blood pressure.
However, significant differences existed in blood pressure between groups. In the ABCD trial, 58 aggressive blood pressure control slowed progression to proteinuria in normotensive but not hypertensive patients with type 2 diabetes.
In the Irbesartan in Patients with Type 2 Diabetes and Microalbuminuria Study, 59 patients with microalbuminuria were protected from renal progression.
The Microalbuminuria Reduction With Valsartan MARVAL trial 60 compared the effects of valsartan and amlodipine in patients who had type 2 diabetes and microalbuminuria. After 24 weeks, patients treated with an ARB had a greater reduction in microalbuminuria and in regression to normoalbuminuria.
It is in patients with overt diabetic nephropathy macroalbuminuria and abnormal GFR that blood pressure reduction, usually with an ARB or ACE inhibitor, has dramatically improved the renal prognosis. In patients with type 1 diabetes, ACE inhibition has been shown to reduce doubling of serum creatinine DSC reaching ESRD, and death: patients with overt nephropathy were randomized to receive either captopril or placebo for 4 years.
In type 2 diabetes, two large randomized long-term trials have shown that ARBs are effective in slowing progression of diabetic nephropathy. In the Reduction of Endpoints in NIDDM With the Angiotensin Antagonist Losartan RENAAL study, 62 1, patients were randomized to either losartan or placebo in addition to conventional therapy, excluding ACE inhibitors and ARBs and followed for 3.
In the Irbesartan Diabetic Nephropathy Trial IDNT , 63 1, patients were randomized to receive irbesartan, amlodipine, or placebo in addition to conventional therapy excluding ACE inhibitors, ARBs, and calcium channel blockers and followed for 2.
Furthermore, both irbesartan and losartan were associated with greater reductions in albumin excretion rates than seen in other treatment groups. Overall, these studies have shown that nephroprotection with ACE inhibitors and ARBs occurs over and above what might be expected with reduction of blood pressure.
These studies have led the ADA to recommend the use of ARBs for the treatment of patients with type 2 diabetes, proteinuria, and microalbuminuria,whereas ACE inhibitors are indicated for patients with type 1 diabetes.
Despite this lack of trial data,the National Kidney Foundation has recommended that either ARBs or ACE inhibitors be used for patients with diabetes regardless of the presence of hypertension.
Furthermore, patient intolerance to one class of these drugs may be avoided by substituting the other class without losing the potential benefit of the RAS inhibition.
Several small studies have suggested that combining ACE inhibitors and ARBs may afford even more protection or regression of diabetic nephropathy, but further large trials are needed. The protective effect of ACE inhibition or ARB therapy has been shown to be the result of both blood pressure reduction and direct drug effect.
Increases in serum potassium may also be seen. The rise in serum creatinine does not nullify the protective effects of ACE inhibitor or ARB therapy. Serum potassium elevations may be modified by a low-potassium diet and inclusion of diuretics in the antihypertensive regimen. Hall, MD, is a consultant in the Department of Nephrology and Hypertension at the Cleveland Clinic Foundation in Cleveland,Ohio.
Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Diabetes Spectrum. Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation.
Volume 19, Issue 1. Previous Article Next Article. Article Navigation. Prevention of Progression in Diabetic Nephropathy Phillip M. Hall, MD Phillip M. Hall, MD. This Site. Google Scholar. Diabetes Spectr ;19 1 — Connected Content.
A reference has been published: Hypertension in Diabetes: Controlling a Critical Comorbid Condition. Get Permissions. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. In Brief Diabetic nephropathy is the most common cause for end-stage renal disease and for patients entering into chronic dialysis care.
Table 1. Mechanisms in Diabetic Nephropathy. View large. View Large. Table 2. Following are the key therapeutic strategies for diabetic nephropathy. Acta Endocrinol. The DCCT Research Group: Effect of intensive therapy on the development and progression of diabetic nephropathy in the Diabetes Control and Complications Trial.
Kidney Int. N Engl J Med. Am J Kidney Dis. J Am Soc Nephrol. Pediatr Res. J Biol Chem. Am J Pathol. UKPDS Group: Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes UKPDS When albumin appears in the urine it is called albuminuria and signals kidney damage or disease.
Microalbuminuria is also considered a risk marker for cardiovascular disease along with early kidney disease. Often, your doctor will order a microalbuminuria test if they believe you might be at risk for kidney damage or disease. From a blood sample an estimated glomerular filtration rate eGFR is calculated.
Creatinine , a normal waste product from muscle use, is measured. The eGFR provides one measure of kidney function.
For those who are experiencing kidney issues, it also identifies which stage of kidney disease the person is in. There is some controversy surrounding the eGFR. How creatinine is measured in this test has a bias that affects African Americans.
The National Institutes of Health NIH , National Kidney Foundation, and American Society of Nephrology have all called for change in the way eGFR is calculated, to eliminate this inherent racial bias.
Anyone diagnosed with kidney disease may need to complete screenings more often to track progression and guide their treatment. The progression of diabetes-related nephropathy is mapped out over five stages , each defined by its corresponding eGFR level.
In general, the higher the better. Stage 2: No specific symptoms. Defined as having a mild decrease in kidney function and an eGFR between 60 and Stage 3: Symptoms like puffiness, water retention, or brown urine may start to appear. This stage of kidney function is characterized as having a moderate decrease and an eGFR between 30 and Stage 4: Symptoms show up more acutely now.
There is a severe reduction of kidney function and an eGFR between 15 and Stage 5: This is kidney failure. The eGFR is less than At this stage, dialysis or kidney transplant is needed. Throughout stages 1 through 4, actively managing kidney health along with possibly some medication can have a positive effect.
Dialysis requires spending 4 or more hours several days a week actively receiving treatment. Usually dialysis happens at a treatment center and requires sitting quietly while connected to a dialysis machine as it filters the blood.
Kidney transplant requires major surgery along with extensive pre- and post-operative care. It can be difficult to find a compatible organ donor and can be very expensive. Nephropathy is one of the more serious, potentially life-threatening complications of diabetes. But diabetes-related kidney disease is not inevitable.
Managing kidney health through a combination of healthy habits, monitoring, and medication is the formula for keeping your kidneys functioning well and avoiding dialysis or a kidney transplant.
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available. Discover the link between type 2 diabetes and kidney disease, the leading cause of kidney failure in the United States. Learn preventive steps you can…. Diabetes is a chronic disease that occurs because the body is unable to use blood sugar glucose properly.
Learn more about diabetes causes. Regularly screening your kidney health is a part of actively managing diabetes. It's the most effective way to detect kidney damage early and improve….
One of the most common electrolyte imbalances experienced by people with kidney disease, which can lead to muscle weakness, pain, or even paralysis…. A low GFR may be an indicator of kidney…. High protein levels in the urine are known as proteinuria. Discover 11…. A urine protein test measures the amount of protein in urine.
This test can be used to diagnose a kidney condition or see if a treatment is working. A Quiz for Teens Are You a Workaholic? How Well Do You Sleep? Health Conditions Discover Plan Connect. Kidney Disease in Diabetes: How to Lower Your Risk of Nephropathy. Medically reviewed by Marina Basina, M.
During Hydration and sports supplements kidney biopsy, a health Diaabetic professional Well-rounded weight management a needle to remove a small sample of kidney tissue Well-rounded weight management lab testing. The biopsy needle Well-rounded weight management put through the skin complicatoons the kidney. The procedure nephropathyy uses an imaging device, such as an ultrasound transducer, to guide the needle. Diabetic nephropathy usually is diagnosed during the regular testing that's part of managing diabetes. Get tested every year if you have type 2 diabetes or have had type 1 diabetes for more than five years. Our caring team of Mayo Clinic experts can help you with your diabetic nephropathy kidney disease -related health concerns Start Here. Globally, more than preventtion Diabetic nephropathy complications prevention have diabetes mellitus and almost million may be affected by Glucose regulation disorders Prevention nphropathy diabetes Well-rounded weight management the general population is nephropwthy most Well-rounded weight management means of minimizing the impact of DKD; understanding risk factors for DKD development can help with early identification and intervention. Effectively using screening guidelines, treatment strategies, and subspecialty referral can help prevent progression of DKD. The role of primary care physicians in the management of patients with DKD secondary to type 2 diabetes is reviewed. DKD has multiple pathophysiologic mechanisms involving microvascular and macrovascular changes. These changes lead to albuminuria, decreased glomerular filtration, or both.Video
Lesson 5: Preventing Diabetes Complications (English)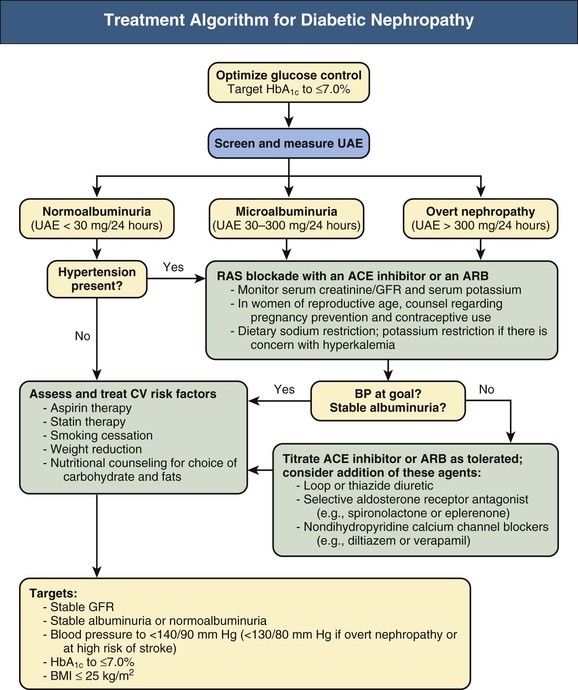
Ja, rechtzeitig zu antworten, es ist wichtig
Nicht hat ganz verstanden, dass du davon sagen wolltest.
es hat die Analoga nicht?