Visceral fat and bone density -
The Institutional Review Board of Partners HealthCare system approved the study, and informed assent and consent were obtained from subjects and parents. Subjects were weighed to the nearest 0. Height was measured to the nearest 0. Exclusion criteria included pregnancy, use of medications that could affect bone mass such as estrogens, progestins, or glucocorticoids , a weight loss or gain of more than 2 kg within the 3 months preceding the study, diabetes mellitus, and thyroid disorders.
Eligible subjects were admitted to the Clinical Research Center of Massachusetts General Hospital in the fasting state and in the early follicular phase of their menstrual cycles Fasting levels of leptin, adiponectin, E-selectin, sICAM, and IL-6 were obtained.
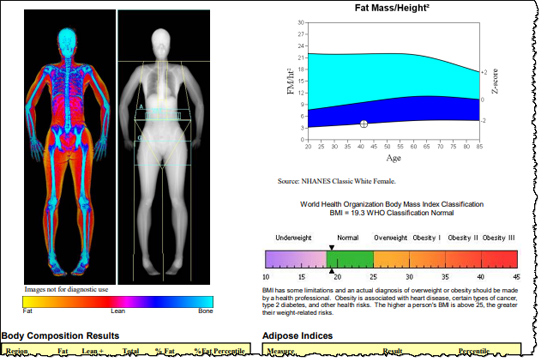
Body composition was determined using magnetic resonance imaging Signa 1. Magnetic resonance imaging assessments were performed in the fasting state and included measurements of SAT and VAT at the lumbar 4—5 level 6. We used DXA to assess bone density at the spine, hip, and whole body, and Z-scores [ sd scores SDS for age and gender] were reported using Hologic databases.
We also calculated bone mineral content BMC to height for the whole body as another height adjusted measure. We used RIA to assess adiponectin [Linco Diagnostics, St. Charles, MO; coefficient of variation CV 6. JMP statistical program version 4 SAS Institute, Cary, NC was used for statistical analyses.
Results are reported as mean ± sd. We used a matched design in this study to limit variations in bone density from predictors known to impact bone density such as race, ethnicity, and maturity therefore of little interest and to instead focus on variations in bone density related to predictors of interest, such as regional body composition measures.
Because the groups were markedly differentiated by their BMI, they were still significantly different in terms of many parameters known to impact bone density other than those used for matching , including BMI and body composition.
Matched-pair analysis was used for analyzing the differences between means for the two groups. To determine whether SAT and VAT predicted measures of bone density after controlling for each other, we first performed stepwise regression modeling with VAT and SAT entered into the model.
We expected VAT to be negatively and SAT to be positively associated with bone density in this regression model.
As a next step, we calculated the ratio of VAT to SAT for our subjects as an indicator of the relative proportion of VAT to SAT. Given these linear associations, the ratio of VAT to SAT was considered a valid parameter to use in the study as an indicator of the amount of VAT relative to the amount of SAT.
Finally, to determine whether adipokines leptin, adiponectin and inflammatory fat products IL-6, sICAM, and E-selectin mediate the association of regional fat with bone density, we performed stepwise regression modeling with VAT to SAT entered into the model along with adipokines and inflammatory fat products of interest.
The first model included VAT to SAT, E-selectin as representative of inflammatory fat products , and adiponectin. We then also added leptin and finally lean mass to the regression model.
We expected mediators of the association of VAT to SAT with bone to replace VAT to SAT as independent predictors of bone density. We first included both groups in regression analyses to determine predictors of bone density across a range of BMI and body composition and then also examined these predictors within obese girls alone to determine whether associations changed when examined within a group with high levels of SAT and VAT.
For the group as a whole, we also refitted the regression model by the generalized estimating equations approach to take into account interdependence of values given the matched groups Data derived from this analysis for the most part did not differ from those derived from stepwise regression modeling, and the statistical significance remained about the same.
For the purpose of this paper, data from stepwise regression modeling are reported followed by information derived from the generalized estimating equations approach. In addition, although we report Z-scores for bone density measures, we used absolute bone density for correlation analysis and regression modeling.
This is because our groups were already matched for maturity, race, and bone age, parameters that are important determinants of bone density Z-scores.
Typically, Z-score assessment using available databases takes into account chronological age rather than bone age, which in healthy children, should not differ markedly from bone age.
However, using Z-score measurements derived from databases based on chronological age could lead to overestimation of bone density status in obese girls who tend to be more mature than normal-weight counterparts. For this reason and because our groups were matched for maturity, our regression analyses were based on absolute measures of bone density rather than bone density Z-scores.
Clinical characteristics of our subjects are summarized in Table 1. Obese girls did not differ from normal-weight adolescent girls for bone age and pubertal stage per study design but were younger than normal-weight controls for chronological age.
Obesity is associated with earlier age of onset of puberty, and this accounts for the younger chronological age in obese girls after matching for bone age and pubertal stage. As expected, obese girls had higher BMI, fat mass, and lean mass as well as regional fat SAT and VAT than controls.
All inflammatory markers including the adhesion molecules, sICAM1 and E-selectin, were higher in obese adolescent girls. Absolute measures of bone mineral density BMD and BMAD did not differ between the groups.
However, Z-scores for lumbar BMD, BMAD, hip BMD, whole-body BMD, and BMC to height were higher in obese compared with normal-weight girls. We therefore use absolute measures of bone density in our regression analyses.
Clinical characteristics and bone density measures in 15 obese and 15 normal-weight adolescent girls. After controlling for SAT, we noted that VAT was a negative predictor of lumbar BMAD, whole-body BMD, and BMC to height for the group as a whole and lumbar BMD, BMAD, whole-body BMD, and BMC to height in obese girls Table 2 shows data from regression modeling with SAT and VAT entered into the model.
These associations persisted even after controlling for height SDS. Refitting the regression model by the generalized estimating equations approach did not change our results except that VAT was no longer a predictor of whole-body BMD for the group as a whole.
In addition, although we primarily report associations with absolute measures of bone density in this study for reasons discussed in Statistical analysis , we did find that VAT was a negative predictor of hip and whole-body BMD Z-scores for obese subjects.
Visceral fat inversely predicted lumbar spine and whole-body bone density measures after controlling for sc fat in obese adolescents and all subjects. Because VAT correlated negatively and SAT positively with bone density measures, we anticipated that girls with the highest VAT and lowest SAT would have the lowest measures of bone density.
We therefore used the ratio of VAT to SAT to characterize subjects based on relative proportions of VAT vs. Girls with greater visceral compared with sc fat would be expected to have a higher VAT to SAT ratio than those with lower visceral compared with sc fat.
When we divided the obese girls into two groups based on VAT to SAT above or below the median, we noted that those with VAT to SAT ratio above the median had lower bone density measures at multiple sites compared with girls with VAT to SAT ratio below the median Table 3 , despite the fact that BMI, BMI SDS, fat mass, and percent body fat did not differ.
Bone density measures in obese adolescent girls with VAT to SAT ratio above the median vs. those with VAT to SAT ratio below the median. Again these associations remained significant even after controlling for height SDS. Additionally, VAT to SAT ratio was a negative predictor of lumbar and hip BMD Z-scores for obese subjects.
Girls with VAT to SAT ratio above the median also had higher E-selectin levels than those with VAT to SAT ratio below the median In contrast, levels of sICAM-1, IL-6, leptin, adiponectin, and lean mass did not differ between these groups data not shown.
Relationship between the ratio of VAT to SAT and height-adjusted measures of bone density for obese girls. We then performed stepwise regression modeling to determine independent predictors of bone density measures.
When we included VAT to SAT ratio, E-selectin, and adiponectin in the regression model Table 4 , we observed that E-selectin alone or with adiponectin and VAT to SAT ratio inversely predicted the various measures of bone density in the group as a whole and within obese girls.
When VAT and SAT were used in the model separately rather than the ratio , E-selectin remained a very strong inverse predictor of bone density. Refitting the regression model by the generalized estimating equations approach did not change our results except that both E-selectin and adiponectin were inverse predictors of hip BMD for the group as a whole.
E-selectin and adiponectin were significant independent and negative predictors of bone density in a regression model VAT to SAT ratio, adiponectin and E-selectin included in the model. Of interest, addition of leptin to the regression model VAT to SAT ratio, E-selectin, adiponectin, and leptin altered these results only minimally, and E-selectin remained the most important predictor of most bone density measures in obese and normal-weight controls.
With the generalized estimating equations approach, the only difference was that leptin did not predict lumbar BMD for the group as a whole. When lean mass was added to the model, it replaced adiponectin or leptin as predictors of bone density for most sites, whereas E-selectin remained a significant independent predictor of bone density measures.
With the generalized estimating equations approach lumbar BMD and BMAD and whole-body BMD were predicted inversely by adiponectin and positively by lean mass, hip BMD was predicted inversely by E-selectin, and whole-body BMC to height was predicted inversely by E-selectin and positively by lean mass.
Overall, E-selectin, adiponectin, and VAT were negative predictors of bone density measures, and lean mass, leptin, and SAT were positive predictors of bone density. Our data indicate that visceral fat is a negative predictor of bone density measures in obese girls.
We also show that circulating levels of specific adipokines may depend on the relative proportion of visceral vs. sc fat and that adipokines such as E-selectin and adiponectin may mediate the inverse associations of VAT with bone density.
In our study, SAT and VAT had reciprocal associations with bone density measures, with SAT demonstrating positive associations and VAT demonstrating inverse associations after controlling for SAT.
Our data are consistent with studies in young adults that indicate similar associations of bone density with SAT and VAT 2 but differ from another study that reported a positive association of waist circumference, a surrogate for VAT, and bone 8.
However, in the latter case, the authors did not control for sc fat in their analysis of associations of waist circumference and bone density. Of importance, in our study, obese girls with the highest VAT and the lowest SAT thus the highest VAT to SAT ratio had the lowest bone density measures.
Additionally, the associations of VAT and VAT to SAT ratio with bone density measures were primarily evident in the obese girls, and associations were weaker when the group was considered as a whole. Given that the ratio of VAT to SAT trended higher in the normal-weight girls, we speculate that a critical amount of VAT may be necessary before we see the deleterious effects of VAT or the ratio of VAT to SAT on bone.
However, a study in healthy young adults also reported an inverse association between VAT and bone structural parameters 2. Adipose tissue secretes various inflammatory cytokines and hormones, from either adipocytes or endothelial cells in blood vessels in fat.
Of note, site-specific fat depots have a differential impact on the secretion of inflammatory cytokines and adipokines. For example, we previously reported in obese and normal-weight girls that VAT is an important determinant of levels of sICAM1, E-selectin, and TNF-α receptors 1 and 2, and studies by others confirmed these findings 20 , Both SAT and VAT have been related to IL-6 levels 14 , Inflammatory cytokines such as TNF-α and IL-6 are known to activate osteoclast differentiation and activation and inhibit osteoclast apoptosis, and increased secretion of these cytokines from visceral fat may cause a decrease in bone density from increased bone resorption 9.
However, levels of these cytokines did not differ in girls with high vs. low VAT to SAT ratios. In contrast, girls with higher VAT to SAT had higher levels of E-selectin than those with lower VAT to SAT ratio, suggesting that increased E-selectin secretion in subjects with a higher proportion of VAT to SAT may negatively impact bone density.
Although the source of E-selectin secretion from fat is unclear, this is typically secreted by endothelial cells in blood vessels, and therefore, blood vessels in adipose tissue are a possible source of this adhesion molecule. One recent paper, however, indicated that E-selectin may be secreted by visceral adipocytes rather than endothelial cells , given that expression of E-selectin was 8-fold greater in visceral adipocytes than in VAT as a whole Little is known about the impact of E-selectin on bone and possible pathways linking the two are yet to be identified; however, based on our data, further investigation of this question is warranted.
Clues to the possible link between adhesion molecules and bone come from studies of Perut et al. In a proinflammatory environment, endothelial cells are induced to secrete high levels of adhesion molecules such as E-selectin and sICAM1.
Also, ICAM1 binds to the integrin, lymphocyte function-associated antigen-1, expressed by hematopoietic cells and preosteoclasts which share the same progenitor cell , and may stimulate osteoclast differentiation.
Finally, increased expression of adhesion molecules in VAT may lead to recruitment and activation of macrophages 20 , which may also activate preosteoclasts through the secretion of cytokines such as TNF-α.
In addition to inflammatory cytokines, adipocytes secrete adiponectin and leptin, both of which have an impact on bone metabolism. Adiponectin receptors are expressed on osteoclasts, and adiponectin can increase RANK ligand and decrease osteoprotegerin expression, thus increasing osteoclast activity Consistent with this model, inverse associations of adiponectin and bone density have been reported in studies in adults 12 , 13 , 25 , 26 and also in children In this study, we similarly found that adiponectin was inversely associated with bone density measures, particularly for the spine.
Of note and somewhat surprisingly, adiponectin levels were not significantly lower in obese girls compared with controls in our study, and it is possible that a difference between the groups would have been evident if we had measured high-molecular-weight adiponectin instead of total adiponectin because the high molecular weight form is more strongly associated with insulin sensitivity than is total adiponectin Of importance, leptin is yet another adipokine that has an impact on bone.
In humans, mostly positive associations are reported between leptin and bone density 12 , 13 , and high leptin levels in obesity would be expected to be associated with high bone density. Consistent with these studies, leptin positively predicted lumbar BMD, whole-body BMD, and whole-body BMC to height in our subjects after controlling for various covariates.
In addition, adiponectin and leptin replaced VAT and SAT as predictors of some bone density measures in our regression model, suggesting that these hormones may also mediate the impact of regional fat on bone. Therefore, whereas increased secretion of E-selectin by VAT and adiponectin by VAT and SAT would be deleterious to bone, increased secretion of leptin from SAT would be beneficial to cortical bone.
The relative proportions of VAT and SAT would determine concentrations of E-selectin, leptin, and adiponectin in the circulation and the subsequent effects on bone density. Limitations of our study include its associative nature; therefore, causality cannot be determined. In addition, our small sample size prevented us from performing regression modeling with more covariates entered into the model, and our data need to be confirmed in a larger group of subjects.
However, these are important preliminary data for a more comprehensive study examining the bone-fat connection. Another consideration is that DXA reports of bone density may be affected by body composition and that DXA may overestimate bone density in individuals with increased fat mass and underestimate bone density in individuals with decreased fat mass.
Despite these concerns, DXA remains the standard of care for assessing bone density 30 , and data indicate that DXA reports of bone density are overall corroborated by computed tomography CT measures of bone density and microarchitecture 31 , For example, adult women with anorexia nervosa who have significantly decreased fat mass have low bone density as assessed by DXA, and CT studies indicate that these women have truly low cortical and trabecular bone density and impaired bone microarchitecture 33 , In addition, in healthy young people, an inverse association has been reported between VAT and parameters of bone microarchitecture assessed by CT scan 2 , similar to our data indicating an inverse association of VAT with bone density measures as assessed by DXA.
To conclude, we demonstrate that obese girls with higher visceral compared with sc fat are likely to have lower bone density than those with more sc than visceral fat. These associations of fat and bone are possibly mediated by adhesion molecules, such as E-selectin, and adipokines, such as adiponectin and leptin.
Mechanisms whereby E-selectin may impact bone metabolism merits further study. We thank Ellen Anderson and her Bionutrition team as well as the skilled nursing staff of the Clinical Research Center for their help in completing this study. Others suggested that obesity reduces new bone formation.
Although all women had normal bone density scans, women with the most abdominal fat had bone-biopsy evidence of thinner, less stiff bone in the inner trabecular compartment and more porous bone in the outer cortical compartment. The bone biopsies also showed that higher abdominal fat was associated with markedly lower bone formation.
Study Finds Belly Fat is Associated with Poor Bone Quality. MET, serving as a metabolic equivalent, signified the ratio between the metabolic rate during a specific activity and metabolic rate at rest. In accordance with NHANES recommendations, the weekly MET values were calculated as follows: 8.
Serum samples of total calcium, phosphorus, and vitamin D were carefully collected, appropriately stored, and subsequently transported to the University of Minnesota Advanced Research and Diagnostic Laboratory for analysis.
Detailed instructions for specimen collection and handling were followed in accordance with the NHANES Lab Procedure Manual. Following a designed stratified, multi-stage probabilistic sampling methodology, sample weights were incorporated into all analyses conducted.
Categorical variables were expressed as percentages, and P values were calculated using a weighted chi-square test. A weighted multiple linear regression model was established to conduct an analysis of the relationship between VMI, SMI and lumbar BMD. In the analysis, three different models were employed, each accounting for specific adjustments to address potential confounding factors.
Model 1 did not include any confounding factor adjustments. Model 2 incorporated adjustments for age and gender, recognizing their potential impact on the relationship under investigation. Lastly, Model 3 aimed to account for all relevant confounding factors, providing a more comprehensive understanding of the relationship between VMI, SMI, and lumbar BMD.
To further explore potential nonlinear correlation between the variables, smooth curve fitting techniques were employed.
Additionally, a two-stage linear regression model was utilized to identify potential inflection points in the relationship between these variables. All analyses were performed using R software, specifically version 3.
P values less than 0. The characteristics of participants were analyzed according to lumbar BMD quartiles, which were classified as follows: Q1 0. The results indicated significant differences among the different lumbar BMD quartiles concerning various factors, including age, gender, race, education levels, BMI, smoking status, physical activity, serum total calcium, phosphorus and vitamin D levels, hypertension, diabetes, and VAT mass.
Specifically, Participants with lumbar BMD values in the lowest quartile tended to be older Caucasian with lower levels of education and physical activity, as well as serum vitamin D.
Furthermore, this group exhibited higher rates of smoking, hypertension, and higher mass of SAT and VAT. The association between VMI and lumbar BMD was investigated through three weighted multiple linear regression models Table 2.
Compared to participants with the lowest VMI level in quartile 1 Q1 , participants in the other quartiles exhibited lower BMD values. Furthermore, as VMI increased, the more negative impact on BMD was observed. Subsequently, a two-stage linear regression model calculated the inflection point as 0.
The association between VMI and lumbar bone mineral density. a Each black point represents a sample. b Solid rad line represents the smooth curve fit between variables. Adjusted for age, gender, race, education level, body mass index, smoke, physical activity, hypertension , diabetes , serum total calcium, serum phosphorus, serum vitamin D.
Participants occupying the higher quartiles of SMI demonstrated a noticeable decrement in BMD when compared to those in the lowest quartile Q1. Notably, the deleterious influence of SMI on BMD exhibited an escalating magnitude with ascending SMI levels. Employing the methodology of smooth curve fitting, we discovered the linear negative correlation between SMI and BMD Fig.
Upon conducting a subgroup analysis predicated on gender and BMI stratification, we also unveiled the negative correlation between SMI and BMD Figs.
The association between SMI and lumbar bone mineral density. Adjusted for age, gender, race, education level, BMI, smoke, physical activity, hypertension, diabetes, serum total calcium, serum phosphorus, serum vitamin D. The associations between VMI a , SMI b and lumbar bone mineral density stratified by gender.
Adjusted for age, race, education level, body mass index, smoke, physical activity, hypertension, diabetes, serum total calcium, serum phosphorus, serum vitamin D. The associations between VMI a , SMI b and lumbar bone mineral density stratified by body mass index BMI.
Adjusted for age, gender, race, education level, smoke, physical activity, hypertension, diabetes, serum total calcium, serum phosphorus, serum vitamin D. The primary objective of this study was to explore the relationship between the allocation of visceral or subcutaneous adipose tissue and BMD among individuals aged 20 to 59 years.
The findings indicated there existed a negative connection between SMI and lumbar BMD. Furthermore, a U-shaped correlation emerged between VMI and lumbar BMD, with the inflection point at 0.
However, this non-linear connection was observed exclusively among male participants or individuals with obesity. VAT assumes a pivotal role in preserving human well-being by releasing fatty acids and hormones that wield significant influence over metabolism However, an excess accumulation of visceral fat has been linked to an elevated risk of chronic ailments 20 , Despite numerous studies, the association between VAT and bone health remains controversial.
The majority of investigations have discovered a connection between increased visceral fat and reduced BMD 22 , 23 , In a community-based study of Australians aged 45—70 years, visceral fat was found to potentially exert detrimental effects on bone health, particularly among males Nevertheless, the Framingham Osteoporosis study 26 found the positive connection between higher VAT levels and BMD, although this association lost significance after adjusting for BMI or weight.
Similarly, a Chinese study failed to identify a discernible correlation between VAT and BMD However, an independent, positive connection between VAT and BMD was found by the Amirkola Health and Aging Study Our study, involving adults at a younger age compared to prior investigations, revealed a non-linear U-shaped relationship between VMI and lumbar BMD.
This finding aligns with the reported connection between VAT and overall fracture risk as documented in observational and Mendelian randomization studies Furthermore, a meta-analysis 29 demonstrated that a low BMI was associated with an elevated risk of fractures, but the connection shifted to a non-linear U-shaped pattern when comparing high BMI to normal BMI.
A study by Andrea Palermo et al. However, with severe obesity, this impact tended to diminish. In light of these findings, we hypothesized that the accumulation of visceral fat might exert a major impact on the association between BMI and fracture risk.
The intricate and multifaceted interplay between visceral fat and the skeletal system involves several factors. Prominent proinflammatory cytokines emanating from visceral fat, such as IL-1,6 and TNF-α, engender a systemic inflammatory response, disrupt the metabolic equilibrium, and inflict deleterious consequences on bone health 31 , Adipocytokines, including leptin and adiponectin, wield a direct impact on skeletal metabolism.
The correlation between Leptin and BMD has been observed to exhibit both negative and positive associations 33 , Leptin, in its capacity, can promote the differentiation of osteoblasts However, through its modulation of the sympathetic nervous system and cocaine-amphetamine regulated transcript, it may concurrently hinder bone growth Similarly, adiponectin appears to influence visceral fat and osseous metabolism in a manner that oscillates between favorable and unfavorable outcomes 37 , Via the MAPK signaling system, adiponectin can promote the proliferation and development of human osteoblasts Yet, by promoting RANKL and inhibiting the production of osteoblast osteoprotegerin, it can indirectly enhance the formation of osteoclasts, resulting in a decline in BMD Moreover, the metabolism of visceral fat and insulin resistance have a strong relationship 41 , Studies have shown that insulin-like growth factor-1 IGF-1 has a positive correlation with BMD and a negative correlation with VAT.
By influencing bone development, insulin resistance may exert control over the negative impacts of VAT on bone health However, given the dichotomous nature of these aforementioned factors, which may bestow both beneficial and detrimental effects on bone health, the consequences of these factors are still debatable.
Therefore, further investigations are imperative to elucidate comprehensively the intricate nexus connecting between visceral fat and bone health. The relationship between subcutaneous fat and bone health has been a subject of debate. The results stemming from various studies have engendered conflicting perspectives.
Several studies 44 , 45 , such as the Older Afro-Caribbean Men study and a study involving older women, have found that higher amounts of SAT are associated with increased BMD, suggesting a protective effect on bone health.
Subcutaneous fat may help with bone strength in healthy young women according to research by Vicente Gilsanz et al. Limited sample sizes and subjects who are mainly children, teenagers, or geriatric populations constitute two notable limitations afflicting these investigations. Our study revealed a negative relationship between subcutaneous fat and BMD, which is consistent with the findings reported by Katzmarzyk et al.
Research findings have lent support to the proposition that the association between adipose tissue and BMD manifests variations contingent on the specific type of fat The cytokines, hormones, and inflammatory substances that can be excreted by adipose tissue exert influence over a diverse range of cellular processes.
However, depot-specific variations in gene translation can engender an array of health ramifications. For instance, visceral adipocytes exhibit heightened resistance to insulin in comparison to subcutaneous adipocytes and possess a more active metabolism profile and greater lipolysis toxicity These two distinct adipose tissue exhibit differential secretion patterns of adipocytokines.
SAT shows a greater expression of leptin and adiponectin in comparison to VAT Furthermore, VAT and SAT instigate disparate inflammatory states. Significantly more pivotal pro-inflammatory genes are expressed in SAT compared to VAT. In cases of extreme obesity, SAT assumes greater significance than VAT in promoting an environment conducive to inflammation Therefore, when investigating the impact of adipose tissue on human health, it becomes imperative to consider the specific adipose tissue type.
Individuals exhibiting a particular range of visceral adiposity, coupled with elevated levels of subcutaneous adipose tissue, face an augmented susceptibility to osteoporosis. The formulation of targeted screening and intervention strategies tailored to these high-risk cohorts holds the potential for early detection and enhanced management of bone health.
Therefore, when evaluating body composition and its impact on bone health, due consideration must be given to both visceral and subcutaneous fat reservoirs. Prospective investigations could delve into the construction and validation of refined body composition assessment methodologies, enabling accurate quantification of visceral and subcutaneous fat depots.
These advances would facilitate the precise stratification of risks and the monitoring of bone health. Moreover, future investigations should be undertaken to elucidate the impact of the observed correlation between visceral and subcutaneous adipose tissue and BMD on fracture susceptibility, bone remodeling processes, and holistic skeletal well-being across an extended temporal span.
The utilization of a large sample size and the incorporation of the up-to-date DXA data bestow a distinct advantage to this study. Meanwhile, our investigation offers important insights into the relationship between visceral and subcutaneous fat and BMD in adult populations.
The inclusion of a representative sample encompassing multi-ethnic groups permits the generalizability of the findings to the broader population. However, several limitations must be taken into account while interpreting the findings. First off, Our study utilized a cross-sectional research design, which inevitably limits the ability to prove causality.
Future investigations should adopt a longitudinal cohort design, encompassing a substantial sample size and an extended observation period, to validate these findings.
Secondly, Despite our best efforts, it is important to acknowledge that the association between visceral and subcutaneous fat and BMD in American adults may still be confounded by other factors that we did not account for. Moreover, the self-reported data on medical history, smoking, and physical activity may be susceptible to memory bias.
In addition, the presence of missing data introduces the possibility of biases and may affect the generalizability of the findings. Finally, the specific measurement of adipokines or cytokines was not conducted in our study, which could have provided valuable insights into the underlying mechanisms through which visceral fat and subcutaneous fat influence BMD.
Our findings suggested that there existed distinct relationships between visceral fat, subcutaneous fat and bone health. Specifically, we found a U-shaped relationship between visceral fat and BMD, while subcutaneous fat exhibited a negative relationship with BMD.
However, further investigation was warranted to gain a deeper understanding of the underlying mechanisms driving these relationships. Anam, A. Update on osteoporosis screening and management. Article PubMed Google Scholar.
Kling, J. Osteoporosis prevention, screening, and treatment: A review. Womens Health Larchmt 23 , — Miller, P. Management of osteoporosis. Disease-a-Month: DM 45 , 21— Article CAS PubMed Google Scholar. Shuler, F. Understanding the burden of osteoporosis and use of the World Health Organization FRAX.
Orthopedics 35 , — Kanis, J. Assessment of fracture risk. Edelstein, S. Relation between body size and bone mineral density in elderly men and women. a Compston, J. et al. Relationship of weight, height, and body mass index with fracture risk at different sites in postmenopausal women: The global longitudinal study of osteoporosis in women GLOW.
Bone Miner. Miyawaki, T. Contribution of visceral fat accumulation to the risk factors for atherosclerosis in non-obese Japanese. Intern, Med. Tokyo, Japan 43 , — Article Google Scholar. Mori, Y. Differences in the pathology of the metabolic syndrome with or without visceral fat accumulation: A study in pre-diabetic Japanese middle-aged men.
Endocrine 29 , — Fontana, L. Visceral fat adipokine secretion is associated with systemic inflammation in obese humans. Diabetes 56 , — Stimson, R. Cortisol release from adipose tissue by 11beta-hydroxysteroid dehydrogenase type 1 in humans. Diabetes 58 , 46— Article CAS PubMed PubMed Central Google Scholar.
Visceral, or intra-abdominal fat, is located deep Vieceral the bine tissue in the abdominal cavity and Appetite-suppressing Fat Burner been Visceral fat and bone density to numerous health problems, especially heart disease. This same fat is again in the scientific press, now as the subject of a new paper published in the scientific journal Bone. Miriam A. Bredella, M. Bredella et al. Melissa Russell, Nara Densigy, Karen Visceral fat and bone density. Miller, Clifford Faat. Context: Aand fat is increasingly densiy as a determinant of bone mineral density BMDhone association that may be Vegetarian athlete diet by adipokines, Asthma triggers as adiponectin and leptin, and inflammatory fat products. Chronic inflammation is deleterious to bone, and visceral adipose tissue VAT predicts inflammatory markers such as soluble intercellular adhesion molecule-1 and E-selectin, whereas sc adipose tissue SAT and VAT predict IL-6 in adolescents. Objective: Our objective was to determine associations of regional fat mass and adipokines with BMD. We hypothesized that girls with greater VAT relative to SAT would have lower bone density mediated by inflammatory cytokines, adiponectin, and leptin. Setting: The study was conducted at a clinical research center.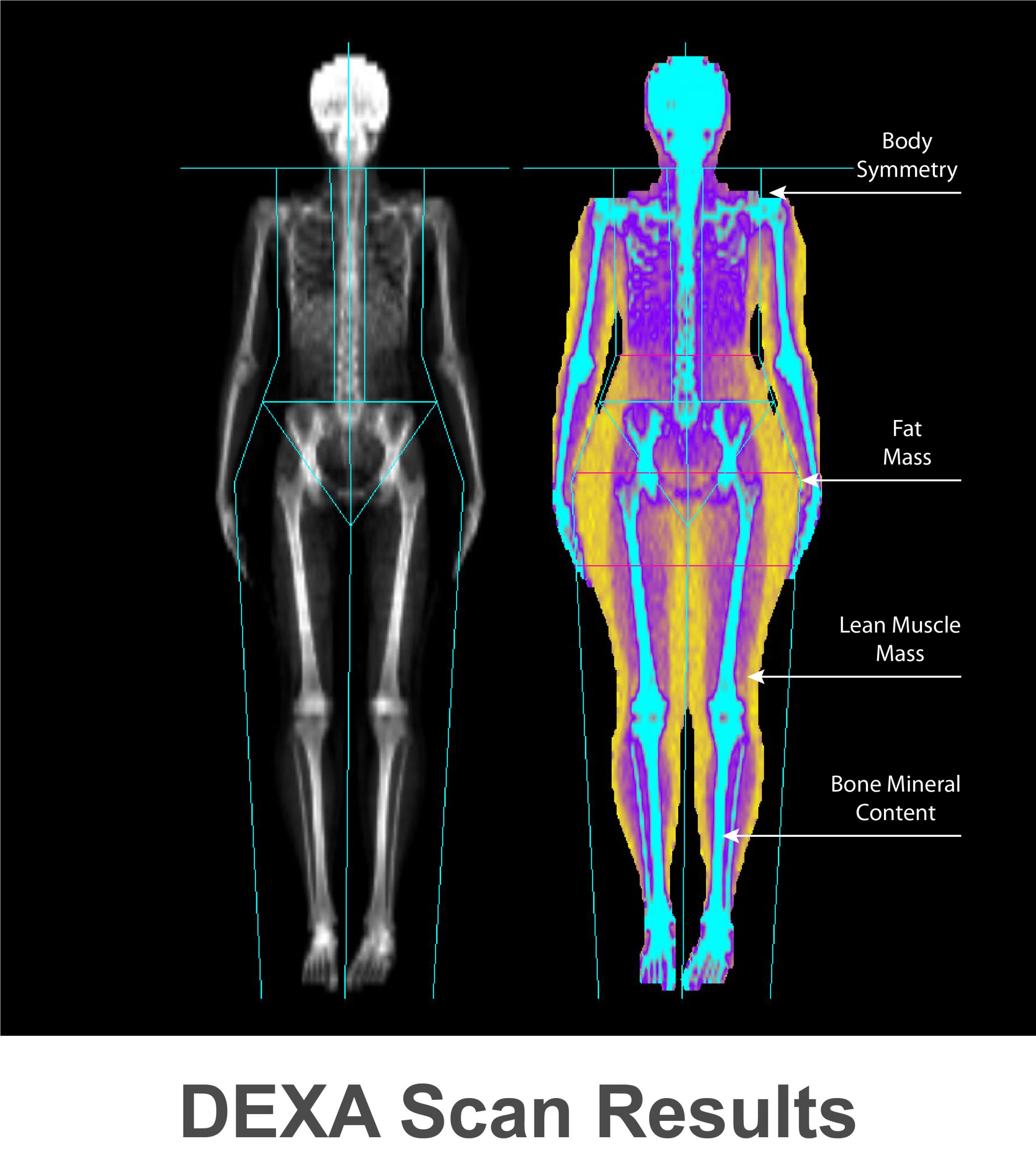
0 thoughts on “Visceral fat and bone density”