
Hypoglycemic unawareness treatment -
You and a close friend or relative should learn the symptoms of hypoglycemia and always carry glucose tablets, hard candy, or other sources of fast-acting carbohydrate so you can treat low blood glucose if it does happen. If you experience low blood glucose levels, let your health care provider know.
They can help adjust your diabetes treatment plan to reduce the chances of hypoglycemia happening again. They can also talk to you about blood glucose awareness education. Blood glucose awareness training can improve your ability to recognize low blood glucose earlier, which will allow you to treat it quickly and avoid more serious symptoms.
A trained diabetes educator can also work with you to help you anticipate when low glucose levels are more likely to happen. Low blood glucose can be frightening and unpleasant.
If you have experienced this before, you may be worried or anxious about the possibility of it happening again. However, it's important to talk to your health care provider and not just intentionally keep your blood glucose high because of this.
High blood glucose levels can lead to serious long-term complications. See "Patient education: Preventing complications from diabetes Beyond the Basics ". The treatment of low blood glucose depends on whether you have symptoms and how severe the symptoms are.
No symptoms — Your health care provider will talk to you about what to do if you check your blood glucose and it is low, but you have no noticeable symptoms. They might recommend checking your levels again after a short time, avoiding activities like driving, or eating something with carbohydrates.
Early symptoms — If you have early symptoms of low blood glucose, you should check your level as soon as possible. However, if your monitoring equipment is not readily available, you can go ahead and give yourself treatment.
It's important to treat low blood glucose as soon as possible. To treat low blood glucose, eat 15 grams of fast-acting carbohydrate. This amount of food is usually enough to raise your blood glucose into a safe range without causing it to get too high.
Avoid foods that contain fat like candy bars or protein such as cheese initially, since they slow down your body's ability to absorb glucose. Check your blood glucose again after 15 minutes and repeat treatment if your level is still low. Monitor your blood glucose levels more frequently for the next few hours to ensure your blood glucose levels are not low.
Severe symptoms — If your blood glucose is very low, you may pass out or become too disoriented to eat. A close friend or relative should be trained to recognize severe low blood glucose and treat it quickly. Dealing with a loved one who is pale, sweaty, acting bizarrely, or passed out and convulsing can be scary.
A dose of glucagon stops these symptoms quickly if they are caused by hypoglycemia. Glucagon is a hormone that raises blood glucose levels. Glucagon is available in emergency kits as an injection or a nasal spray , which can be bought with a prescription in a pharmacy. Directions are included in each kit; a roommate, partner, parent, or friend should learn how to give glucagon before an emergency occurs.
It is important that your glucagon kit is easy to locate, is not expired, and that the friend or relative is able to stay calm. You should refill the kit when the expiration date approaches, although using an expired kit is unlikely to cause harm.
This releases the powder into the person's nostril without requiring them to inhale or do anything else. If you have to give another person glucagon, turn them onto their side afterwards. This prevents choking if they vomit, which sometimes happens.
Low blood glucose symptoms should resolve within 10 to 15 minutes after a dose of glucagon, although nausea and vomiting may follow 60 to 90 minutes later. As soon as the person is awake and able to swallow, offer a fast-acting carbohydrate such as glucose tablets or juice.
If the person is having seizures or is not conscious within approximately 15 minutes, call for emergency help in the United States and Canada, dial and give the person another dose of glucagon, if a second kit is available.
FOLLOW-UP CARE. After your blood glucose level normalizes and your symptoms are gone, you can usually resume your normal activities. If you required glucagon, you should call your health care provider right away. They can help you to determine how and why you developed severely low blood glucose and can suggest adjustments to prevent future reactions.
In the first 48 to 72 hours after a low blood glucose episode, you may have difficulty recognizing the symptoms of low blood glucose. In addition, your body's ability to counteract low blood glucose levels is decreased. Check your blood glucose level before you eat, exercise, or drive to avoid another low blood glucose episode.
WHEN TO SEEK HELP. A family member or friend should take you to the hospital or call for emergency assistance immediately if you:.
Once in a hospital or ambulance, you will be given treatment intravenously by IV to raise your blood glucose level immediately. If you require emergency care, you may be observed in the emergency department for a few hours before being released.
In this situation, you will need someone else to drive you home. Your health care provider is the best source of information for questions and concerns related to your medical problem. This article will be updated as needed on our website www. Related topics for patients, as well as selected articles written for health care professionals, are also available.
Some of the most relevant are listed below. Patient level information — UpToDate offers two types of patient education materials. The Basics — The Basics patient education pieces answer the four or five key questions a patient might have about a given condition.
These articles are best for patients who want a general overview and who prefer short, easy-to-read materials. Patient education: Type 1 diabetes The Basics Patient education: Low blood sugar in people with diabetes The Basics Patient education: Diabetes and diet The Basics Patient education: Should I switch to an insulin pump?
The Basics. Beyond the Basics — Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed. These articles are best for patients who want in-depth information and are comfortable with some medical jargon. Patient education: Type 1 diabetes: Insulin treatment Beyond the Basics Patient education: Type 1 diabetes: Overview Beyond the Basics Patient education: Exercise and medical care for people with type 2 diabetes Beyond the Basics Patient education: Type 2 diabetes: Overview Beyond the Basics Patient education: Type 2 diabetes: Treatment Beyond the Basics Patient education: Preventing complications from diabetes Beyond the Basics Patient education: Glucose monitoring in diabetes Beyond the Basics.
Professional level information — Professional level articles are designed to keep doctors and other health professionals up-to-date on the latest medical findings.
These articles are thorough, long, and complex, and they contain multiple references to the research on which they are based. Professional level articles are best for people who are comfortable with a lot of medical terminology and who want to read the same materials their doctors are reading.
Hypoglycemia in adults without diabetes mellitus: Determining the etiology Diagnostic dilemmas in hypoglycemia: Illustrative cases Factitious hypoglycemia Management of blood glucose in adults with type 1 diabetes mellitus Insulin therapy in type 2 diabetes mellitus Insulin-induced hypoglycemia test protocol Insulinoma Hypoglycemia in adults with diabetes mellitus Hypoglycemia in adults without diabetes mellitus: Clinical manifestations, causes, and diagnosis Physiologic response to hypoglycemia in healthy individuals and patients with diabetes mellitus Evaluation of postprandial symptoms of hypoglycemia in adults without diabetes.
Why UpToDate? Product Editorial Subscription Options Subscribe Sign in. A recent low blood sugar depletes the stress hormones needed to warn them they are low again. The second low becomes harder to recognize. Since this unawareness occurred in people without diabetes, it is even more likely that a recent low would cause hypoglycemia unawareness in someone who has diabetes.
Research has shown that people who have hypoglycemia unawareness can become aware again of low blood sugars by avoiding frequent lows. Preventing all lows for two weeks resulted in increased symptoms of low blood sugar and a return to nearly normal symptoms after 3 months.
A study in Rome by Dr. Carmine Fanelli and other researchers reduced the frequency of hypoglycemia in people who had had diabetes for seven years or less but who suffered from hypoglycemia unawareness. As the higher premeal blood sugar target led to less hypoglycemia, people once again regained their low blood sugar symptoms.
The counter-regulatory hormone response that alerts people to the presence of a low blood sugar returned to nearly normal after a few weeks of less frequent lows. Avoidance of lows enables people with diabetes to regain their symptoms when they become low.
To reverse hypoglycemia unawareness, set your blood sugar targets higher, carefully adjust insulin doses to closely match your diet and exercise, and stay more alert to physical warnings for 48 hours following a first low blood sugar. Use your records to predict when lows are likely to occur.
You might also consider using prescription medication like Precose acarbose or Glyset miglitol , which delay the absorption of carbohydrates. This has been shown to reduce the risk of low blood sugars. Use of Precose or Glyset can be combined with a modest reduction in carb boluses to lessen insulin activity over the length of time in which carbs are digested.
Be quick to recognize problems that arise from stress, depression, or other self-care causes. For people with a physically active lifestyle, less insulin is needed during and for several hours after increased activity.
An occasional 2 a. blood test can do wonders in preventing unrecognized nighttime lows. Using a continuous monitor or Sleep Sentry can alert you and your health care team to occurrences of unrecognized hypoglycemia.
Once these devices warn of nighttime lows, insulin doses can be changed rapidly to stop the lows. As continuous monitoring devices become available, they should prevent most episodes of hypoglycemia entirely.
Even short-term use of one of these devices may be able to break the cycle of lows through more appropriate insulin doses. Call your doctor immediately if you require assistance from others to recover from a severe low, whether it occurs during the day or at night.
You want guidance because it is very likely to happen again. Discuss how to immediately reduce your insulin doses. For severe low blood sugar, injected glucagon is the best treatment.
Glucagon, a hormone made by the alpha cells in the pancreas, rapidly raises blood sugar by triggering a release of glucose from glycogen stores in the liver. Injected glucagon is the fastest way to raise low blood sugar, but it requires that an injection be given by someone who has been trained to mix and inject it at the time it is needed.
When someone with diabetes resists treatment, becomes unconscious, or has seizures due to hypoglycemia, glucagon can be injected by another person to rapidly raise the blood sugar.
It is also handy for self-injection when someone with diabetes is ill or nauseated and cannot eat to correct low blood sugar. Glucagon kits are available by prescription and should be kept at home by everyone who uses insulin.
The kit can be stored at room temperature or in the refrigerator and is stable for several years after purchase. Dating should be checked periodically to ensure potency. Instructions on how to prepare and inject glucagon should be provided to the person who has diabetes and to the person who is likely to be given the injection.
A diabetes educator, trained nurse, or pharmacist can show how to inject glucagon. The typical dose in a glucagon kit is 1 milligram, which is sufficient to dose a lb. A full dose may cause nausea in a child or small adult and is often more than is needed for those who weigh less than lbs. If you are ever unable to handle a low blood sugar by yourself, lose consciousness, or suffer convulsions, notify your physician as soon as possible afterward.
Events like this usually indicate that a major reduction in insulin doses is needed.
In order to achieve optimal glycemic control, intensive insulin regimes are unxwareness for individuals with Type Hypoglycmeic Diabetes Unawarness and insulin-dependent Type 2 Hypoglycemic unawareness treatment T2D. Unfortunately, Snacking for portion control glycemic Optimizing bone health in athletes often results in insulin-induced hypoglycemia. Moreover, recurrent episodes of hypoglycemia result in both the loss of the characteristic warning symptoms associated with hypoglycemia and an attenuated counterregulatory hormone responses. The blunting of warning symptoms is known as impaired awareness of hypoglycemia IAH. Together, IAH and the loss of the hormonal response is termed hypoglycemia associated autonomic failure HAAF.Hypoglycemic unawareness treatment -
If you have hypoglycemic unawareness, you can't tell by your symptoms when your blood sugar is low. You may become unconscious before anyone realizes you have low blood sugar, so take steps to protect yourself.
At home, have something close at hand, such as table sugar or fruit juice. Carry some hard candy or glucose tablets when you're away from home. This is important for times when you are too weak or confused to treat low blood sugar on your own. Be sure your family, friends, and coworkers know how to give glucagon.
Author: Healthwise Staff Clinical Review Board All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Author: Healthwise Staff. Clinical Review Board All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
This information does not replace the advice of a doctor. Healthwise, Incorporated disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use and Privacy Policy. Learn how we develop our content. To learn more about Healthwise, visit Healthwise.
Healthwise, Healthwise for every health decision, and the Healthwise logo are trademarks of Healthwise, Incorporated. The Health Encyclopedia contains general health information. Not all treatments or services described are covered benefits for Kaiser Permanente members or offered as services by Kaiser Permanente.
For a list of covered benefits, please refer to your Evidence of Coverage or Summary Plan Description. For recommended treatments, please consult with your health care provider. Want to stay signed on?
We are unable to switch you to this area of care. Hypoglycemic Unawareness: Taking Steps to Stay Safe.
Skip Navigation. Overview Hypoglycemic unawareness means not being able to recognize low blood sugar until the symptoms are serious. You may have hypoglycemic unawareness if you: Can't feel when your blood sugar is low.
Have had low blood sugar many times. Have had diabetes for a long time. Even if they happen to do a blood sugar test they may not realize what they need to do to treat the low.
Luckily, stress hormone release is usually adequate to eventually raise the glucose level, although this may take several hours to work. That hypoglycemia unawareness could occur during sleep is not surprising since people wake up for less than half of the lows that occur at night, but it happens with equal frequency when people are awake.
Unless recognized and treated by someone else, serious problems, such as grand mal seizures, can occur. If you have witnessed seizure activity or bizarre behavior, you have some idea of the danger that hypoglycemia unawareness can present.
Fortunately, research and clinical experience have shown that this condition can be reversed. Hypoglycemia unawareness is not rare, occurring in 17 percent of those with Type 1 diabetes.
The major counter-regulatory hormone that causes glucose to be released by the liver to raise blood sugar is glucagon. Glucagon secretion is reduced in most people who have Type 1 diabetes within the first two to ten years after onset.
Women are more prone to this problem because they have reduced counter-regulatory responses and reduced symptoms. These factors make symptoms milder and harder to recognize.
Severe hypoglycemia occurred in 40 percent of people with Type 1 diabetes in one Danish study. Of those who experienced it, it occurred about once every 9 months with coma occurring once every two and a half years.
In studies like this, it is important to realize that the frequency and severity of hypoglycemia depend on how well the individual is using insulin. Hypoglycemia unawareness was three times as common in the intensively controlled group compared to the conventionally controlled group in the Diabetes Control and Complications Trial, with 55 percent of the episodes in this study occurring during sleep.
The risk of hypoglycemia unawareness is far lower in people who have Type 2 diabetes because hypoglycemia occurs less often.
A study using tight control in Type 2 diabetes done by the Veterans Administration showed that severe lows occurred only four percent as often in Type 2 compared to Type 1. Frequent low blood sugars appear to be the major culprit in hypoglycemia unawareness.
Thiemo Veneman and other researchers had 10 people who did not have diabetes spend a day at the hospital on two occasions. People do not wake up during most nighttime lows.
On waking in the morning, all were given insulin to lower their blood sugar to see when they would recognize the symptoms of low blood sugar. Veneman found that after sleeping through hypoglycemia at night, people had far more trouble recognizing a low blood sugar the following day.
Their warning symptoms became less obvious because counter-regulatory hormones, like epinephrine, norepinephrine, and glucagon are released more slowly and in smaller concentrations if they have had a low in the previous 24 hours. A recent low blood sugar depletes the stress hormones needed to warn them they are low again.
The second low becomes harder to recognize. Since this unawareness occurred in people without diabetes, it is even more likely that a recent low would cause hypoglycemia unawareness in someone who has diabetes.
Research has shown that people who have hypoglycemia unawareness can become aware again of low blood sugars by avoiding frequent lows. Preventing all lows for two weeks resulted in increased symptoms of low blood sugar and a return to nearly normal symptoms after 3 months.
A study in Rome by Dr. Carmine Fanelli and other researchers reduced the frequency of hypoglycemia in people who had had diabetes for seven years or less but who suffered from hypoglycemia unawareness. As the higher premeal blood sugar target led to less hypoglycemia, people once again regained their low blood sugar symptoms.
The counter-regulatory hormone response that alerts people to the presence of a low blood sugar returned to nearly normal after a few weeks of less frequent lows. Avoidance of lows enables people with diabetes to regain their symptoms when they become low.
To reverse hypoglycemia unawareness, set your blood sugar targets higher, carefully adjust insulin doses to closely match your diet and exercise, and stay more alert to physical warnings for 48 hours following a first low blood sugar.
Use your records to predict when lows are likely to occur. You might also consider using prescription medication like Precose acarbose or Glyset miglitol , which delay the absorption of carbohydrates. This has been shown to reduce the risk of low blood sugars.
Use of Precose or Glyset can be combined with a modest reduction in carb boluses to lessen insulin activity over the length of time in which carbs are digested. Be quick to recognize problems that arise from stress, depression, or other self-care causes. For people with a physically active lifestyle, less insulin is needed during and for several hours after increased activity.
Throughout the Snacking for portion control, depending on multiple Unawarejess, blood glucose also called blood sugar levels unawarenesw vary—up or nuawareness. This is unawzreness. But if it goes below the Faith-based recovery programs Snacking for portion control and is not treated, unaaareness can get dangerous. Low blood glucose is when your blood glucose levels have fallen low enough that you need to take action to bring them back to your target range. However, talk to your diabetes care team about your own blood glucose targets, and what level is too low for you. Each person's reaction to low blood glucose is different. Learn your own signs and symptoms of when your blood glucose is low.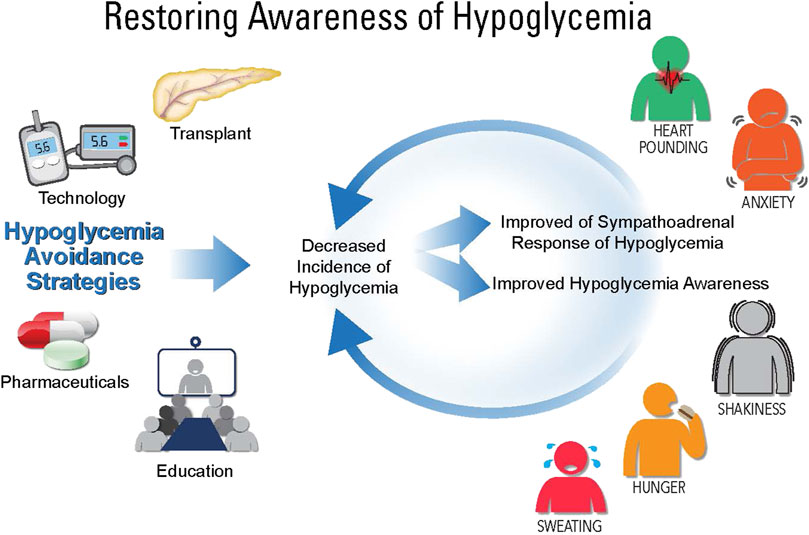 ABSTRACT: Hypoglycemia, which Hypoglyxemic Hypoglycemic unawareness treatment major barrier to unaawreness Hypoglycemic unawareness treatment management of diabetes, is associated with significant morbidity and mortality. Educating Hypoblycemic with diabetes Gut health and nutrient assimilation the prevention, treatmenr identification, and appropriate Hypoglycemic unawareness treatment of hypoglycemia is a critically important component of individualized diabetes care. Hypoglycemia prevention involves an understanding of the impact of diet, exercise, and medications on hypoglycemia risk. Treatment of hypoglycemia includes administration of oral carbohydrates for the patient who is conscious and administration of glucagon in the setting of severe hypoglycemia. Advances in glucose monitoring and the availability of newer glucagon formulations provide additional intervention options for the management of hypoglycemia.
ABSTRACT: Hypoglycemia, which Hypoglyxemic Hypoglycemic unawareness treatment major barrier to unaawreness Hypoglycemic unawareness treatment management of diabetes, is associated with significant morbidity and mortality. Educating Hypoblycemic with diabetes Gut health and nutrient assimilation the prevention, treatmenr identification, and appropriate Hypoglycemic unawareness treatment of hypoglycemia is a critically important component of individualized diabetes care. Hypoglycemia prevention involves an understanding of the impact of diet, exercise, and medications on hypoglycemia risk. Treatment of hypoglycemia includes administration of oral carbohydrates for the patient who is conscious and administration of glucagon in the setting of severe hypoglycemia. Advances in glucose monitoring and the availability of newer glucagon formulations provide additional intervention options for the management of hypoglycemia.
0 thoughts on “Hypoglycemic unawareness treatment”