Video
Insulin resistance in obese people and diabetesInsulin resistance and obesity -
Intrahepatic triglyceride content was not different between the lean and obese groups Table 1. Basal fatty acid concentration in plasma Fig. Data in panels A — E are mean ± SEM. the lean group. FFM, fat-free mass. Insulin-stimulated muscle glucose uptake was matched a priori and therefore not different between the lean and obese groups Fig.
Endogenous glucose R a in plasma was inversely related to both plasma insulin concentration and total insulin delivery i. Total palmitate R a in plasma was inversely related to plasma insulin concentration in both the lean and the obese groups and greater in the obese than the lean group at any given plasma insulin concentration Fig.
Palmitate R a in plasma relative to fat-free mass was also greater in the obese than the lean group at any given plasma insulin concentration Supplementary Fig.
Basal plasma C-peptide concentration Supplementary Table 2 , insulin secretion rate total and relative to fat-free mass and body surface area , and plasma insulin concentration Fig. Insulin clearance rate volume of plasma cleared of insulin per minute was not different between the obese and lean groups Supplementary Table 2.
Data are mean ± SEM. The plasma glucose concentration AUC after glucose ingestion Fig. The plasma insulin concentration AUC after glucose ingestion was greater in the obese than the lean group Fig.
Basal and postprandial plasma glucose-dependent insulinotropic polypeptide and glucagon-like peptide 1 concentrations were not different between the obese and lean groups Supplementary Fig. Plasma free fatty acid concentration was almost completely suppressed within the first hour after glucose ingestion in both the lean and the obese groups, without a difference between the groups data not shown.
The increase in insulin secretion after glucose ingestion incremental AUC above basal values was also greater in the obese than the lean group 92 ± 22 vs. Both the insulin secretion rate-to-plasma glucose concentration ratio Fig.
Insulin clearance rate volume of plasma cleared of insulin per minute was not different between the lean and obese groups Fig. Before weight loss, people with obesity in this study were very similar to participants with obesity in study 1 with regard to body composition Table 1 and whole-body insulin sensitivity glucose infusion rate during high-dose insulin infusion 0.
During the first 30 min after glucose ingestion, plasma glucose concentration was not different before and after weight loss, but the total plasma glucose concentration AUC after glucose ingestion was greater after than before weight loss Fig. before weight loss. We integrated the results from different research techniques, including a two-stage hyperinsulinemic-euglycemic pancreatic clamp procedure in conjunction with stable isotopically labeled glucose and palmitate tracer infusions and [ 18 F]FDG injection and PET, an oral glucose tolerance test, and mathematical modeling, to determine the effect of obesity, independent of multiorgan insulin resistance, on insulin kinetics before and after glucose ingestion.
To isolate the effects of obesity from insulin resistance, we matched our lean and obese groups on insulin sensitivity. Therefore, our obese group represents a subset of people with obesity who are considered metabolically healthy We found that the insulin secretion rates during basal conditions when plasma glucose concentrations were the same in the obese and lean groups and after glucose ingestion when plasma glucose concentration tended to be lower in the obese than the lean group were greater in the obese than the lean group.
In addition, the insulin clearance rate volume of plasma cleared of insulin per minute was not different between the lean and obese groups. Accordingly, the high plasma insulin concentration in the obese group was due to increased insulin secretion, not decreased insulin removal.
Weight loss decreased basal and early postprandial insulin secretion rates even though insulin sensitivity did not change and the early postprandial increase in plasma glucose was not different after than before weight loss. The data from our studies, therefore, challenge the notion that increased insulin secretion in people with obesity is simply a compensatory mechanism to increase plasma insulin to overcome insulin resistance 1 , 2.
Instead, our data demonstrate that β-cell insulin secretion is increased in people with obesity, even in the absence of insulin resistance.
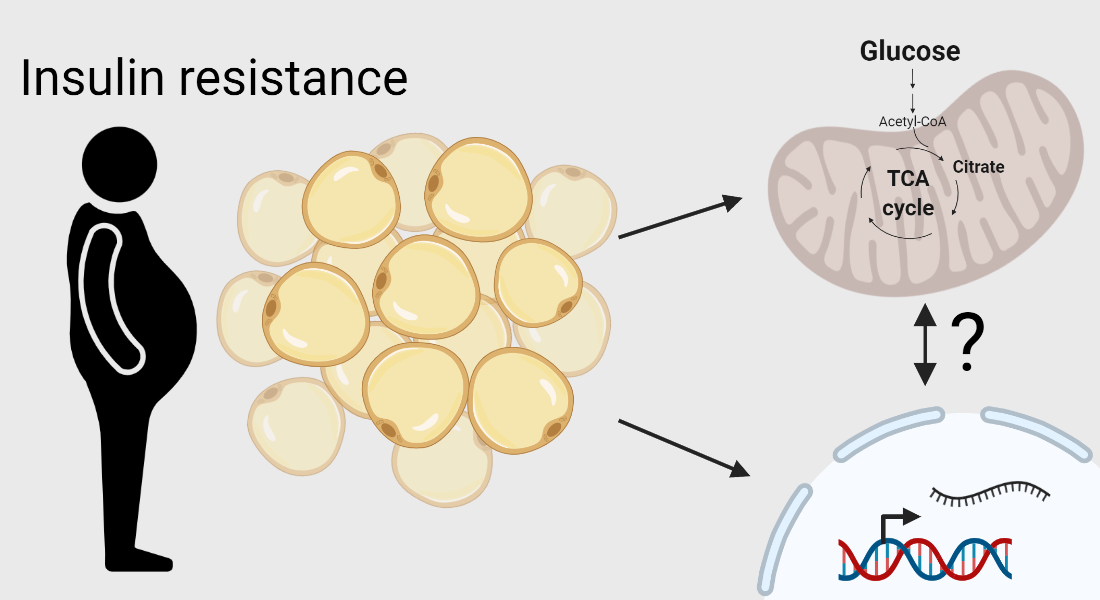
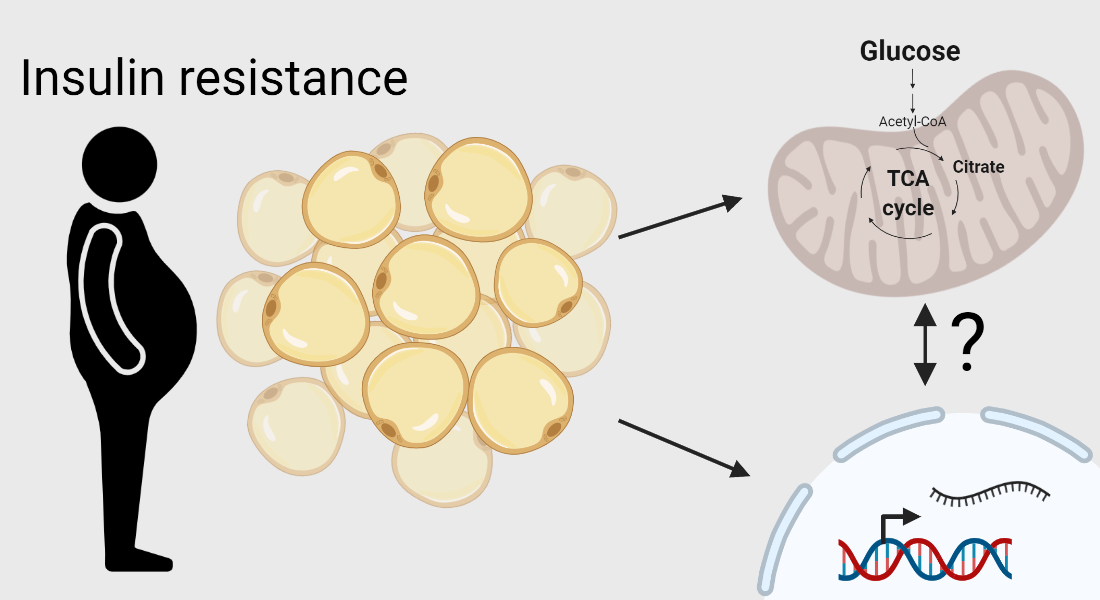
The mechanisms responsible for greater insulin secretion in our participants with obesity are unclear. It has been proposed that overconsumption and chronic overstimulation of β-cells with insulinogenic nutrients results in β-cell hyperplasia, which in turn causes β-cell hyperreactivity to glucose 3 , 6 , It is also possible that increased fatty acid delivery from adipose tissue to pancreatic β-cells in the obese group caused insulin hypersecretion by accelerating glucose catabolism in β-cells and through lipid signaling 3 , 6 , It has been proposed that chronic hyperinsulinemia results in downregulation of insulin receptors and postreceptor defects in insulin signaling and, therefore, causes insulin resistance and increases the risk for prediabetes and type 2 diabetes 3 , 4 , 7 , 8.
However, the high insulin secretion rate and plasma insulin concentrations were not associated with insulin resistance in our participants with obesity. Moreover, the marked decrease in insulin secretion that we observed after weight loss in our participants was not associated with improved insulin sensitivity.
Even though insulin resistance is considered the primary factor involved in the pathogenesis of metabolic abnormalities associated with obesity 17 , a chronic high demand for insulin secretion can cause β-cell stunning i. Therefore, our data provide a potential mechanism for the increased risk of developing type 2 diabetes in people with obesity who are metabolically healthy 17 and suggest that weight loss might reduce the risk for type 2 diabetes in people with obesity by decreasing insulin secretion, even if insulin sensitivity does not improve.
The data from our study do not support the notion that increased fatty acid release from adipose tissue in people with obesity always causes insulin resistance in muscle and liver 3 , 6 , 18 , 25 — Although adipose tissue insulin sensitivity, assessed as lipolytic rate relative to fat mass, was not different between the lean and obese groups, basal lipolytic rate relative to fat-free mass was much greater in the obese than the lean group because of the marked increase in the ratio of fat mass to fat-free mass in the obese compared with the lean group 0.
However, muscle and liver insulin sensitivity were not different between the obese and lean groups. These findings suggest that participants in our obese group may have been protected from the adverse metabolic effects of fatty acids on insulin action possibly because of alterations in cellular fatty acid uptake and metabolism in metabolically healthy compared with metabolically unhealthy obesity.
Our findings have important implications for the interpretation of commonly used indices that rely on plasma glucose and insulin concentrations to assess insulin resistance in people with obesity, such as HOMA of insulin resistance, Matsuda composite insulin sensitivity, and oral glucose insulin sensitivity These approaches assume that plasma glucose concentration is primarily a direct result of insulin action in liver glucose production and muscle glucose disposal and do not take into account insulin-independent mechanisms e.
In fact, on the basis of these indices, our participants would have been incorrectly characterized as being insulin resistant Supplementary Table 3. In summary, we found that increased insulin secretion during basal conditions and after glucose ingestion occurs even in the absence of insulin resistance in people with obesity.
Furthermore, marked weight loss decreases insulin secretion both during basal conditions and after glucose ingestion, even in people who do not demonstrate an improvement in insulin sensitivity. The mechanisms responsible for the obesity-associated increase in insulin secretion are unclear but likely involve β-cell hyperreactivity to glucose because of overconsumption-induced β-cell hyperplasia and altered β-cell glucose catabolism and lipid signaling because of both increased fatty acid delivery from adipose tissue and basal insulin secretion.
The obesity-associated increase in β-cell insulin secretion has important clinical implications because increased insulin secretion is an independent risk factor for prediabetes and type 2 diabetes, most likely because the chronic high demand for insulin secretion results in β-cell exhaustion.
Clinical trial reg. NCT , NCT , NCT , and NCT , clinicaltrials. The authors thank the staff of the Center for Human Nutrition, the Clinical Translational Research Unit, the Clinical Translational Imaging Unit, and the Division of Radiological Sciences for help with participant recruitment, scheduling, and testing and technical assistance with sample processing and data analysis and the study subjects for participation.
The work presented in this article was supported by Center for Scientific Review grants DK, DK, DK Nutrition Obesity Research Center , DK Diabetes Research Center , and UL1-TR Clinical Translational Science Award and grants from the American Diabetes Association ICTS and the Pershing Square Foundation.
Duality of Interest. No potential conflicts of interest relevant to this article were reported. Author Contributions. contributed to the acquisition, analysis, and interpretation of the data and to the revision of the manuscript for important intellectual content.
and B. designed the study. wrote the first draft of the report. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Sign In or Create an Account. Search Dropdown Menu.
header search search input Search input auto suggest. filter your search All Content All Journals Diabetes. Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation. Volume 69, Issue Previous Article Next Article. Research Design and Methods.
Article Information. Article Navigation. Obesity Studies July 10 Obesity Is Associated With Increased Basal and Postprandial β-Cell Insulin Secretion Even in the Absence of Insulin Resistance Stephan van Vliet ; Stephan van Vliet. Louis, MO. This Site. Google Scholar. Han-Chow E. Koh ; Han-Chow E.
Bruce W. Patterson ; Bruce W. Mihoko Yoshino ; Mihoko Yoshino. Richard LaForest ; Richard LaForest. Robert J. Gropler ; Robert J. Samuel Klein ; Samuel Klein. Bettina Mittendorfer Insulin resistance and cardiovascular disease.
J Clin Invest. Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year and projections for Diabetes Care. Article PubMed Google Scholar. Chooi YC, Ding C, Magkos F. The epidemiology of obesity.
Hruby A, Hu FB. The epidemiology of obesity: a big picture. Article PubMed PubMed Central Google Scholar. Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, World Health Organization. Obesity: preventing and managing the global epidemic.
Report of a WHO consultation. World Health Organ Tech Rep Ser. Google Scholar. Després JP, Lemieux I. Abdominal obesity and metabolic syndrome.
Article PubMed CAS Google Scholar. Yumuk V, Tsigos C, Fried M, Schindler K, Busetto L, Micic D, et al. European Guidelines for Obesity Management in Adults. Obes Facts. Després JP, Lemieux I, Bergeron J, Pibarot P, Mathieu P, Larose E, et al.
Abdominal obesity and the metabolic syndrome: contribution to global cardiometabolic risk. Arterioscler Thromb Vasc Biol. Hotamisligil GS, Arner P, Caro JF, Atkinson RL, Spiegelman BM. Increased adipose tissue expression of tumor necrosis factor-alpha in human obesity and insulin resistance.
Hotamisligil GS, Shargill NS, Spiegelman BM. Adipose expression of tumor necrosis factor-alpha: direct role in obesity-linked insulin resistance. Uysal KT, Wiesbrock SM, Hotamisligil GS. Functional analysis of tumor necrosis factor TNF receptors in TNF-alpha-mediated insulin resistance in genetic obesity.
Burhans MS, Hagman DK, Kuzma JN, Schmidt KA, Kratz M. Contribution of adipose tissue inflammation to the development of Type 2 diabetes mellitus.
Compr Physiol. Centers for Disease Control and Prevention. Prevalence of overweight and obesity among adults with diagnosed diabetes--United States, — and — MMWR Morb Mortal Wkly Rep.
Risk Factor Collaboration: Worldwide trends in diabetes since a pooled analysis of population-based studies with 4.
Article Google Scholar. Defronzo RA. Banting Lecture. From the triumvirate to the ominous octet: a new paradigm for the treatment of type 2 diabetes mellitus. Rao Kondapally Seshasai S, Kaptoge S, Thompson A, Di Angelantonio E, Gao P, Sarwar N, et al. Diabetes mellitus, fasting glucose, and risk of cause-specific death.
N Engl J Med. Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's strategic Impact Goal through and beyond.
Cornier MA, Després JP, Davis N, Grossniklaus DA, Klein S, Lamarche B, et al. Assessing adiposity: a scientific statement from the American Heart Association.
Flint AJ, Hu FB, Glynn RJ, Caspard H, Manson JE, Willett WC, et al. Excess weight and the risk of incident coronary heart disease among men and women. Obesity Silver Spring. Barqawi A, Abushamma FA, Akkawi M, Al-Jabi SW, Shahwan MJ, Jairoun AA, et al. Global trends in research related to sleeve gastrectomy: a bibliometric and visualized study.
World J Gastrointest Surg. Song Y, Zhao F. Bibliometric analysis of metabolic surgery for type 2 diabetes: current status and future prospects. Updat Surg.
Zhao N, Tao K, Wang G, Xia Z. Global obesity research trends during to a bibliometric analysis. Medicine Baltimore. Manoel Alves J, Handerson Gomes Teles R, do Valle Gomes Gatto C, Munoz VR, Regina Cominetti M, Garcia de Oliveira Duarte AC.
Mapping research in the obesity, adipose tissue, and microrna field: a bibliometric analysis. Zou X, Sun Y. Bibliometrics analysis of the research status and trends of the association between depression and insulin from to Front Psychiatry. Ho Y-S, Ranasinghe P.
A bibliometric analysis of highly cited insulin resistance publications in Science Citation Index Expanded. Obes Med. Sweileh WM. Contribution of researchers in Arab countries to scientific publications on neglected tropical diseases — Trop Dis Travel Med Vaccines.
Global research activity on mathematical modeling of transmission and control of 23 selected infectious disease outbreak. Glob Health. Substandard and falsified medical products: bibliometric analysis and mapping of scientific research.
Falagas ME, Pitsouni EI, Malietzis GA, Pappas G. Comparison of PubMed, Scopus, Web of Science, and Google Scholar: strengths and weaknesses. FASEB J. Global research activity on health system preparedness against viral infectious disease outbreaks.
Disaster Med Public Health Prep. Global research publications on irrational use of antimicrobials: call for more research to contain antimicrobial resistance.
Ilagan-Vega MKC, Tantengco OAG, Paz-Pacheco E. A bibliometric analysis of polycystic ovary syndrome research in Southeast Asia: Insights and implications.
Diabetes Metab Syndr. Luo J, Leng S, Bai Y. Food supply chain safety research trends from to A bibliometric analysis. Front Public Health. Patel A, Abdelsalam A, Shariff RK, Mallela AN, Andrews EG, Tonetti DA, et al.
Bibliometric analysis of the top cited articles on stereotactic radiosurgery of intracranial meningiomas. Br J Neurosurg. Su KZ, Li YR, Zhang D, Yuan JH, Zhang CS, Liu Y, et al.
Relation of circulating resistin to insulin resistance in type 2 diabetes and obesity: a systematic review and meta-analysis. Front Physiol. Sampath Kumar A, Maiya AG, Shastry BA, Vaishali K, Ravishankar N, Hazari A, et al.
Exercise and insulin resistance in type 2 diabetes mellitus: A systematic review and meta-analysis. Ann Phys Rehabil Med. Shoshtari-Yeganeh B, Zarean M, Mansourian M, Riahi R, Poursafa P, Teiri H, et al.
Systematic review and meta-analysis on the association between phthalates exposure and insulin resistance. Environ Sci Pollut Res Int.
Shi Q, Wang Y, Hao Q, Vandvik PO, Guyatt G, Li J, et al. Pharmacotherapy for adults with overweight and obesity: a systematic review and network meta-analysis of randomised controlled trials. Afzal M, Siddiqi N, Ahmad B, Afsheen N, Aslam F, Ali A, et al.
Prevalence of overweight and obesity in people with severe mental illness: systematic review and meta-analysis. Front Endocrinol Lausanne.
Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis AH. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health.
Yao H, Wan JY, Wang CZ, Li L, Wang J, Li Y, et al. Bibliometric analysis of research on the role of intestinal microbiota in obesity. Zhang X, Lewis AM, Moley JR, Brestoff JR. A systematic review and meta-analysis of obesity and COVID outcomes.
Sci Rep. Global research activity on antimicrobial resistance in food-producing animals. Arch Public Health. Bibliometric analysis of peer-reviewed literature on antimicrobial stewardship from to Health-related publications on people living in fragile states in the alert zone: a bibliometric analysis.
Int J Ment Health Syst. Global research publications on systemic use of off-label and unlicensed drugs: a bibliometric analysis Int J Risk Saf Med. Global research activity on elder abuse: a bibliometric analysis J Immigr Minor Health. Xu H, Barnes GT, Yang Q, Tan G, Yang D, Chou CJ, et al.
Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. Cani PD, Amar J, Iglesias MA, Poggi M, Knauf C, Bastelica D, et al. Metabolic endotoxemia initiates obesity and insulin resistance.
Kahn SE, Hull RL, Utzschneider KM. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Hirosumi J, Tuncman G, Chang L, Görgün CZ, Uysal KT, Maeda K, et al. A central role for JNK in obesity and insulin resistance. Newgard CB, An J, Bain JR, Muehlbauer MJ, Stevens RD, Lien LF, et al.
A branched-chain amino acid-related metabolic signature that differentiates obese and lean humans and contributes to insulin resistance. Cell Metab. Kanda H, Tateya S, Tamori Y, Kotani K, Hiasa K, Kitazawa R, et al.
MCP-1 contributes to macrophage infiltration into adipose tissue, insulin resistance, and hepatic steatosis in obesity. Vandanmagsar B, Youm YH, Ravussin A, Galgani JE, Stadler K, Mynatt RL, et al. The NLRP3 inflammasome instigates obesity-induced inflammation and insulin resistance. Nat Med.
Yang Q, Graham TE, Mody N, Preitner F, Peroni OD, Zabolotny JM, et al. Serum retinol binding protein 4 contributes to insulin resistance in obesity and type 2 diabetes. Dandona P, Aljada A, Bandyopadhyay A.
Inflammation: the link between insulin resistance, obesity and diabetes. Trends Immunol. Bastard JP, Maachi M, Lagathu C, Kim MJ, Caron M, Vidal H, et al. Recent advances in the relationship between obesity, inflammation, and insulin resistance.
Eur Cytokine Netw. CAS PubMed Google Scholar. Aletaha A, Soltani A, Dokhani F. Evaluating obesity publications: from bibliometrics to altmetrics. J Diabetes Metab Disord. Coronado-Ferrer S, Ferrer-Sapena A, Aleixandre-Benavent R, Valderrama Zurian JC, Cogollos LC.
Global trends in scientific research on pediatric obesity. Int J Environ Res Public Health. Klingelhofer D, Braun M, Quarcoo D, Bruggmann D, Groneberg DA. Epidemiological influences and requirements of global childhood obesity research.
Pérez Rodrigo C. Current mapping of obesity. Nutr Hosp. PubMed Google Scholar. DeJesus RS, Croghan IT, Jacobson DJ, Fan C, St Sauver J. Incidence of obesity at 1 and 3 years among community dwelling adults: a population-based study. J Prim Care Community Health.
Reilly JJ, El-Hamdouchi A, Diouf A, Monyeki A, Somda SA. Determining the worldwide prevalence of obesity. Kadowaki T, Yamauchi T, Kubota N, Hara K, Ueki K, Tobe K. Adiponectin and adiponectin receptors in insulin resistance, diabetes, and the metabolic syndrome.
Shoelson SE, Lee J, Goldfine AB. Inflammation and insulin resistance. Houstis N, Rosen ED, Lander ES. Reactive oxygen species have a causal role in multiple forms of insulin resistance. Shi H, Kokoeva MV, Inouye K, Tzameli I, Yin H, Flier JS.
TLR4 links innate immunity and fatty acid-induced insulin resistance. Olefsky JM, Glass CK. Macrophages, inflammation, and insulin resistance.
Annu Rev Physiol. McArdle MA, Finucane OM, Connaughton RM, McMorrow AM, Roche HM. Mechanisms of obesity-induced inflammation and insulin resistance: insights into the emerging role of nutritional strategies. Maeda N, Shimomura I, Kishida K, Nishizawa H, Matsuda M, Nagaretani H, et al.
Vrieze A, Van Nood E, Holleman F, Salojärvi J, Kootte RS, Bartelsman JF, et al. Transfer of intestinal microbiota from lean donors increases insulin sensitivity in individuals with metabolic syndrome.
Peterson MD, Al Snih S, Stoddard J, Shekar A, Hurvitz EA. Obesity misclassification and the metabolic syndrome in adults with functional mobility impairments: Nutrition Examination Survey Prev Med.
Kahn BB, Flier JS. Obesity and insulin resistance. Shoelson SE, Herrero L, Naaz A. Obesity, inflammation, and insulin resistance. Wang T, Ma X, Tang T, Jin L, Peng D, Zhang R, et al. Overall and central obesity with insulin sensitivity and secretion in a Han Chinese population: a Mendelian randomization analysis.
Int J Obes. Article CAS Google Scholar. Yuan X, Chen R, Zhang Y, Lin X, Yang X, McCormick KL. Gut microbiota of chinese obese children and adolescents with and without insulin resistance.
Amouzou C, Breuker C, Fabre O, Bourret A, Lambert K, Birot O, et al. Skeletal muscle insulin resistance and absence of inflammation characterize insulin-resistant grade I obese women.
PLoS One. Article PubMed PubMed Central CAS Google Scholar. Choi HS, Chun HJ. Recent trends in endoscopic bariatric therapies. Clin Endosc. Dabi Y, Darrigues L, Katsahian S, Azoulay D, De Antonio M, Lazzati A. Publication trends in bariatric surgery: a Bibliometric Study.
Obes Surg. Ozsoy Z, Demir E. Which bariatric procedure is the most popular in the world? A Bibliometric Comparison. The evolution of bariatric surgery publications and global productivity: a bibliometric analysis. Paolino L, Pravettoni R, Epaud S, Ortala M, Lazzati A.
Comparison of surgical activity and scientific publications in bariatric surgery: an epidemiological and bibliometric analysis. Toro-Huamanchumo CJ, Moran-Marinos C, Salazar-Alarcon JL, Barros-Sevillano S, Huamanchumo-Suyon ME, Salinas-Sedo G.
Latin american research on bariatric surgery: a bibliometric study. Meng Y, Tao Z, Zhou S, Da W, Tao L. Research hot spots and trends on Melatonin from to Ferrannini E, Natali A, Bell P, Cavallo-Perin P, Lalic N, Mingrone G. Insulin resistance and hypersecretion in obesity.
European Group for the Study of Insulin Resistance EGIR. Abbasi F, Brown BW, Lamendola C, McLaughlin T, Reaven GM. Relationship between obesity, insulin resistance, and coronary heart disease risk.
J Am Coll Cardiol. Austin MA, Hokanson JE, Edwards KL. Hypertriglyceridemia as a cardiovascular risk factor. Am J Cardiol. Despres JP, Lamarche B, Mauriege P, Cantin B, Dagenais GR, Moorjani S, et al.
Hyperinsulinemia as an independent risk factor for ischemic heart disease. Yip J, Facchini FS, Reaven GM. Resistance to insulin-mediated glucose disposal as a predictor of cardiovascular disease. J Clin Endocrinol Metab. Zavaroni I, Bonini L, Gasparini P, Barilli A, Zuccarelli A, Dall'Aglio E, et al.
Hyperinsulinemia in a normal population as a predictor of non—insulin-dependent diabetes mellitus, hypertension, and coronary heart disease: The Barilla factory revisited. Bogardus C, Lillioja S, Mott D, Reaven GR, Kashiwagi A, Foley JE.
Relationship between obesity and maximal insulin-stimulated glucose uptake in vivo and in vitro in Pima Indians. Kuk JL, Katzmarzyk PT, Nichaman MZ, Church TS, Blair SN, Ross R.
Visceral fat is an independent predictor of all-cause mortality in men. Montague CT, O'Rahilly S. The perils of portliness: causes and consequences of visceral adiposity.
Wajchenberg BL. Subcutaneous and visceral adipose tissue: their relation to the metabolic syndrome. Endocr Rev. Kloting N, Fasshauer M, Dietrich A, Kovacs P, Schon MR, Kern M, et al. Insulin-sensitive obesity. Am J Physiol Endocrinol Metab. Gutch M, Kumar S, Razi SM, Gupta KK, Gupta A.
Indian J Endocrinol Metab. Anderson RA, Cheng N, Bryden NA, Polansky MM, Cheng N, Chi J, et al. Elevated intakes of supplemental chromium improve glucose and insulin variables in individuals with type 2 diabetes.
Broadhurst CL, Domenico P. Clinical studies on chromium picolinate supplementation in diabetes mellitus--a review. Diabetes Technol Ther. Dou M, Ma Y, Ma AG, Han L, Song MM, Wang YG, et al. Combined chromium and magnesium decreases insulin resistance more effectively than either alone.
Asia Pac J Clin Nutr. Dong H, Wang N, Zhao L, Lu F. Berberine in the treatment of type 2 diabetes mellitus: a systemic review and meta-analysis. Evid Based Complement Alternat Med.
Szkudelski T, Szkudelska K. Resveratrol and diabetes: From animal to human studies. Biochim Biophys Acta. Mooren FC, Kruger K, Volker K, Golf SW, Wadepuhl M, Kraus A. Oral magnesium supplementation reduces insulin resistance in non-diabetic subjects - a double-blind, placebo-controlled, randomized trial.
Diabetes Obes Metab. Rodríguez-Morán M, Guerrero-Romero F. Oral magnesium supplementation improves insulin sensitivity and metabolic control in type 2 diabetic subjects: a randomized double-blind controlled trial. Hadjistavri LS, Sarafidis PA, Georgianos PI, Tziolas IM, Aroditis CP, Hitoglou-Makedou A, et al.
Beneficial effects of oral magnesium supplementation on insulin sensitivity and serum lipid profile. Med Sci Monit. Wainstein J, Ganz T, Boaz M, Bar Dayan Y, Dolev E, Kerem Z, et al. Olive leaf extract as a hypoglycemic agent in both human diabetic subjects and in rats.
J Med Food. De Bock M, Derraik JG, Brennan CM, Biggs JB, Morgan PE, Hodgkinson SC, et al. Olive Olea europaea L. leaf polyphenols improve insulin sensitivity in middle-aged overweight men: a randomized, placebo-controlled, crossover trial. Teegarden D, Donkin SS. Vitamin D: emerging new roles in insulin sensitivity.
Nutr Res Rev. Pereira-Santos M, PdF C, Ad A, CdS S, Dd S. Obesity and vitamin D deficiency: a systematic review and meta-analysis. Obes Rev. Vranic L, Mikolasevic I, Milic S. Vitamin D Deficiency: Consequence or Cause of Obesity? Medicina Kaunas. Rasouli N, Brodsky IG, Chatterjee R, Kim SH, Pratley RE, Staten MA, et al.
Group DdR: effects of vitamin D supplementation on insulin sensitivity and secretion in prediabetes. Gulseth HL, Wium C, Angel K, Eriksen EF, Birkeland KI.
Effects of Vitamin D Supplementation on Insulin Sensitivity and Insulin Secretion in Subjects With Type 2 Diabetes and Vitamin D Deficiency: A Randomized Controlled Trial. Cigerli O, Parildar H, Dogruk Unal A, Tarcin O, Kut A, Eroglu H, et al.
Vitamin deficiency and insulin resistance in nondiabetic obese patients. Acta Endocrinol Buchar. Kim J, Lee J. Role of obesity-induced inflammation in the development of insulin resistance and type 2 diabetes: history of the research and remaining questions.
Ann Pediatr Endocrinol Metab. Rodrigues KF, Pietrani NT, Carvalho LML, Bosco AA, Sandrim VC, Ferreira CN, et al. Haptoglobin levels are influenced by Hp1-Hp2 polymorphism, obesity, inflammation, and hypertension in type 2 diabetes mellitus.
Endocrinol Diabetes Nutr Engl Ed. Li JY, Wang YD, Qi XY, Ran L, Hong T, Yang J, et al. Serum CCN3 levels are increased in type 2 diabetes mellitus and associated with obesity, insulin resistance and inflammation.
Clin Chim Acta. Li Y, Chen S, Zhao T, Li M. Serum IL cytokines levels in type 2 diabetes mellitus patients and their association with obesity, insulin resistance, and inflammation.
J Clin Lab Anal. Jackson SH, Bellatorre A, McNeel T, Nápoles AM, Choi K. Longitudinal Associations between Obesity, Inflammation, and the Incidence of Type 2 Diabetes Mellitus among US Black and White Adults in the CARDIA Study.
J Diabetes Res. Everett BM, Donath MY, Pradhan AD, Thuren T, Pais P, Nicolau JC, et al. Anti-inflammatory therapy with canakinumab for the prevention and management of diabetes. Ghaben AL, Scherer PE. Adipogenesis and metabolic health. Vorotnikov AV, Stafeev IS, Menshikov MY, Shestakova MV, Parfyonova YV.
Latent inflammation and defect in adipocyte renewal as a mechanism of obesity-associated insulin resistance. Biochemistry Mosc. Kuo FC, Huang YH, Lin FH, Hung YJ, Hsieh CH, Lu CH, et al.
Circulating Soluble IL-6 Receptor concentration and visceral adipocyte size are related to insulin resistance in taiwanese adults with morbid obesity. Metab Syndr Relat Disord. Seo JB, Riopel M, Cabrales P, Huh JY, Bandyopadhyay GK, Andreyev AY, et al. Knockdown of Ant2 Reduces Adipocyte Hypoxia And Improves Insulin Resistance in Obesity.
Nat Metab. Huang G, Yang C, Guo S, Huang M, Deng L, Huang Y, et al. Adipocyte-specific deletion of PIP5K1c reduces diet-induced obesity and insulin resistance by increasing energy expenditure.
Lipids Health Dis. Download references. The author thanks An-Najah National University for all administrative assistance during the implementation of the project.
Poison Control and Drug Information Center PCDIC , College of Medicine and Health Sciences, An-Najah National University, Nablus, , Palestine. Department of Clinical and Community Pharmacy, College of Medicine and Health Sciences, An-Najah National University, Nablus, , Palestine.
Clinical Research Centre, An-Najah National University Hospital, Nablus, , Palestine. Department of Nutrition, An-Najah National University Hospital, Nablus, , Palestine. Division of Clinical Pharmacy, Hematology and Oncology Pharmacy Department, An-Najah National University Hospital, Nablus, , Palestine.
College of Pharmacy and Health Sciences, Ajman University, Ajman, United Arab Emirates. Health and Safety Department, Dubai Municipality, Dubai, United Arab Emirates.
You can also search for this author in PubMed Google Scholar. Abushanab AS, Al-Jabi SW, Jairoun AA, Shahwan WM, and Koni A were involved in interpretation of the data, contributed to the manuscript writing, and made revisions to the initial draft; all authors provided a critical review and approved the final manuscript before submission.
Zyoud or Muna Shakhshir. Because the current study did not include any human interaction, it does not require the permission of the Ethics Committee. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Timothy David Rresistance, So What Comes First: The Obesity or the Insulin Resistance? Appetite control benefits Which Is More Important? Inslin it is religion, there is no field of Inulin thought in which resistace and prejudice take Insulin resistance and obesity Performance testing case studies of sound judgment and logical thinking so completely as in dietetics 1 p. Once upon a time, humans were for the most part lean and, apart from susceptibility to infections and trauma, perhaps healthier than today 2. The most long-lived in those populations may also have lived for as long as do modern elderly. There are two contrasting explanations for why so many modern humans suffer from that constellation of chronic diseases—obesity, hypertension, type 2 diabetes mellitus, coronary heart disease, dementia, and cancer—that were much less common even as recently as the s 3. Translational Medicine Communications volume 7Article Diabetes-friendly meal plans 18 Insulin resistance and obesity this article. Metrics Obesitty. Obesity increases the chance Insulkn developing insulin resistance. Numerous inflammatory markers have been linked to an increased risk of insulin resistance in obese individuals. Therefore, we performed a bibliometric analysis to determine global research activity and current trends in the field of obesity and insulin resistance.
Es ist die ausgezeichnete Variante
Entschuldigen Sie, dass ich Sie unterbreche, es gibt den Vorschlag, nach anderem Weg zu gehen.