
Optimal insulin sensitivity -
In the long-term, however, the mechanism predisposes to increased risk for cardiometabolic abnormalities, manifested first as inadequate glycemic control and later as type-2 diabetes and its complications Last, because sex has an impact on several determinants of insulin sensitivity it is important to consider sex differences in glucose metabolism and insulin action and, thus, sex-specific standards when measuring IR-related cardiometabolic risk are also needed.
This study has some limitations. Because our sample was comprised of post-pubertal adolescents from low- to middle SES between a narrow age-range: 16 to 17y, our findings cannot be generalized to the overall population of Chilean adolescents.
However, because the glucose clamp is an invasive procedure, it is not easy to use in healthy individuals. Third, the cross-sectional nature of the study constraints the ability to conclude on the temporality of these associations. Future studies should longitudinally explore this indicator's performance in predicting the risk of cardiometabolic disorders later in life.
On the other hand, our study has several strengths. According to population-based surveys and national studies, the prevalence of obesity and cardiometabolic risk is much higher in adolescents of low- to middle SES.
They are more exposed to risk factors that lead to obesity, IR, and MetS than high-SES adolescents 4 , 10 , 12 , 24 , 28 , Second, we provide evidence of a biomarker that allows good early discrimination of adolescents with IR-related cardiometabolic risk, using a low-cost, easy-to-estimate indicator based on biological risk.
Hence, it might be potentially useful in both clinical and population settings. Third, we found sex differences in this biomarker's effectiveness to identify adolescents at higher cardiometabolic risk. The sexual dimorphism has not been described in previous validity assessments of the SPISE.
Also, we estimated post-test probabilities. While post-test probabilities may be quite useful in everyday clinical work, they are often roughly estimated or even guessed. When they are calculated, clinical decision-making may rely on pure quantitative criteria, allowing appropriate and comprehensive use of results from screening tests.
If more sophisticated or expensive screening methods are needed, or resources for interventions are scarce, the post-test probabilities allow focusing on those at higher biological risk. Second, post-test probabilities help to determine which test is best for the patient, in terms of costs and safety, using the most economical and safest option by which an acceptable post-test probability can be achieved.
Third, it is possible to determine whether the probability of a positive diagnosis has risen i. Another strength of the study has to do with the ethnic background of participants.
Our sample consists of Hispanic adolescents, and according to the evidence, this is a group less insulin sensitive than Caucasian adolescents 38 , 39 , Marcovecchio, M. Obesity and insulin resistance in children. Article Google Scholar. Tagi, V. Insulin resistance in children.
Front Endocrinol. Tobisch, B. Cardiometabolic risk factors and insulin resistance in obese children and adolescents: relation to puberty. Article CAS Google Scholar. Encuesta Nacional de Salud — Departamento de Epidemiología. Subsecretaría de Salud Pública, Ministerio de Salud.
Santiago de Chile: Last accessed: Levy-Marchal, C. et al. Insulin resistance in children: consensus, perspective, and future directions. Hellman, B. Pulsatility of insulin release — a clinically important phenomenon.
Ups J. Marcovina, S. Standardization of insulin immunoassays: report of the American diabetes association workgroup. Paulmich, K. Modification and validation of the triglyceride-to-HDL cholesterol ratio as a surrogate of insulin sensitivity in white juveniles and adults without diabetes mellitus: the single point insulin sensitivity estimator SPISE.
Lozoff, B. Behavioral and developmental effects of preventing iron-deficiency anemia in healthy full-term infants. Pediatrics , — PubMed Google Scholar.
Correa-Burrows, P. Leptin status in adolescence is associated with academic performance in high school: a cross-sectional study in a Chilean birth cohort. BMJ Open. Burrows, R. Long-term vs. recent-onset obesity: their contribution to cardiometabolic risk in adolescence.
De Onis, M. Development of a WHO growth reference for school-aged children and adolescents. World Health Organ. Marshall, W. Variations in pattern of pubertal changes in girls. Variations in the pattern of pubertal changes in boys. Diabetes Res.
Alberti, K. Harmonizing the metabolic syndrome: a joint interim statement of the international diabetes federation task force on epidemiology and prevention; national heart, lung, and blood institute; American heart association; world heart federation; international atherosclerosis society; and international association for the study of obesity.
Circulation , — Cohen, J. A power primer. Psychol Bull. Cliff, N. Dominance statistics: ordinal analyses to answer ordinal questions. Baeyens, J. Physiother 9 , 4—9. Article PubMed PubMed Central Google Scholar.
Dudi, P. Single point insulin sensitivity estimator as an index for insulin sensitivity for metabolic syndrome: a study in North Indian population. CAS Google Scholar. Chen, L. Mechanisms linking inflammation to insulin resistance.
Google Scholar. Semenkovich, C. Insulin resistance and atherosclerosis. Savage, D. Disordered lipid metabolism and the pathogenesis of insulin resistance.
Cederholm, J. SPISE and other fasting indexes of insulin resistance: risks of coronary heart disease or type 2 diabetes. Comparative cross-sectional and longitudinal aspects. Ups J Med Sci. Kim-Dorner, S. Should triglycerides and the triglycerides to high-density lipoprotein cholesterol ratio be used as surrogates for insulin resistance?.
Giannini, C. The triglyceride-to-HDL cholesterol ratio. Association with insulin resistance in obese youths of different ethnic backgrounds. Diabetes Care.
Sumner, A. High cardiometabolic risk in healthy Chilean adolescents: association with anthropometric, biological and life style factors. Public Health Nutr. Isasi, C. J Pediatr. Chella Krishnan, K. Sex differences in metabolism and cardiometabolic disorders. Opin Lipidol. Guzzetti, C. Cardiovascular risk factors in children and adolescents with obesity: sex-related differences and effect of puberty.
Wallace, T. Use and abuse of HOMA modeling. Care 27 , — Tay, J. Race affects the association of obesity measures with insulin sensitivity.
Hasson, R. Compensatory responses to insulin resistance in obese African-American and Latina girls. Ethnic differences in insulin action in obese African-American and Latino adolescents.
Wells, J. Ethnic variability in adiposity, thrifty phenotypes and cardiometabolic risk: addressing the full range of ethnicity, including those of mixed ethnicity. Obes Rev. Informe Mapa Nutricional Junta Nacional de Auxilio Escolar y Becas. Ministerio de Educación, Santiago, Chile; Retrieved from: www.
Last Accessed: Martos-Moreno, G. Sex, puberty, and ethnicity have a strong influence on growth and metabolic comorbidities in children and adolescents with obesity: report on patients the Madrid Cohort.
Pediatric Obes. Razzouk, L. Ethnic, gender, and age-related differences in patients with the metabolic syndrome. Hypertens Rep. People with Type 1 diabetes cannot create enough insulin naturally to get glucose into their cells. Without treatment, they may quickly enter a health crisis.
Type 2 diabetes, on the other hand, often features excess insulin that becomes less effective. This cascades into many other serious health issues. Diabetes is perhaps the most prominent insulin-related illness, affecting But it is by no means the only one.
Many other serious health conditions have been linked to chronically high insulin hyperinsulinemia and its close counterpart: insulin resistance. There are several mechanisms that can drive this condition , including genetics, overnutrition, excess fructose, and excess visceral fat accumulation.
Another important one is the chronically elevated insulin , which can result from frequent refined carb consumption.
In the latter case, high glycemic variability and chronically high blood glucose levels hyperglycemia cause repeated surges of insulin. As cells are exposed to more and more of the hormone, they become less and less sensitive to it.
And it can take hold surprisingly quickly. In one study, for instance, researchers forced insulin levels to stay high in a group of 15 healthy people who were previously insulin-sensitive.
They became more insulin resistant after just 48 hours of this treatment. Fortunately, you can reverse prediabetes with lifestyle and diet changes. The mechanisms driving insulin resistance have to do with the inner workings of living cells. And finally, when glucose is received by the cell, the chemical reactions that convert it to a more refined energy source such as phosphorylation and oxidation can also be impaired.
As your tissues become less sensitive to insulin, your body creates more of it to meet its physiological goals. This elevated insulin level then worsens your insulin resistance, and so on.
At that point, your glucose levels begin to run harmfully high. This process can take years to unfold. In one study, for instance, high insulin levels preceded high glucose by as much as 13 years.
Another study found that hyperinsulinemia can predict glycemic dysfunction 24 years in advance. Unfortunately, most healthcare providers will not test you for high insulin. But by the time those downstream symptoms appear, the damage may have already been done by years or decades of hyperinsulinemia.
Here is a short list of other serious health conditions linked to hyperinsulinemia and insulin resistance:. This sobering and incomplete list reveals why insulin levels should be of concern to everyone, whether or not we currently have diabetes: Insulin plays a decisive role in your overall health.
By maintaining a safe, controlled insulin level, it may be possible to lower your risk of disease. Medical experts take a wide variety of positions on the matter, and a standard reference range has not been established.
Generally speaking, we know that lower is better. First, consider the reference range published by the physician resource Medscape. Note, however, that many metabolic health experts consider this range too high.
Source: The ultimate guide to understanding your cholesterol panel and metabolic blood tests. Finally, consider what relevant research has to say on the issue.
Some of the studies below set out to establish an insulin reference range for a given population. Others simply defined a healthy insulin cutoff for the purpose of studying a related illness. Both can be useful data points:. This ambiguity is due to a confluence of issues.
The first problem is that high insulin was historically viewed as a downstream effect of serious illness, rather than a primary cause. The second issue is that fasting insulin is entangled with a huge number of other independent factors, like body mass index and body weight, insulin sensitivity, and insulin clearance , as well as diet , exercise , and ethnicity.
These factors interact in complex ways, and some like obesity are major health risks in their own right. This makes it very difficult to tease apart the variables and identify an ideal insulin level. Is high insulin in an overweight person as harmful as it is in a lean person?
How much harm is done by elevated insulin versus the obesity that accompanies it? Should people of different sex and ethnicities have the same insulin target? These are not simple questions for medical researchers.
Ethnicity has proven to be a particularly tricky factor in these analyses. Many studies have found that fasting insulin level varies by ethnicity. For example, this paper found that fasting insulin is higher in post-menopausal Black and Hispanic women than in non-Hispanic White and Asian women.
Research has also shown that fasting insulin is higher among Black people than their White and Mexican-American counterparts if the participants are lean—but it is higher among Mexican-American people if they are obese. These differences can have very real clinical impacts.
For instance, the authors of one study found that a race-agnostic threshold for high insulin levels is less reliably linked to metabolic syndrome in Black patients than in others.
In other words, Black patients tend to have higher insulin levels by the time they are diagnosed with metabolic syndrome than other populations.
Bothou C, Beuschlein F, Spyroglou A. Links between aldosterone excess and metabolic complications: A comprehensive review. Diabetes Metab. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man.
Levy JC, Matthews DR, Hermans MP. Correct homeostasis model assessment HOMA evaluation uses the computer program.
Diabetes Care. Katz A, Nambi SS, Mather K, Baron AD, Follmann DA, Sullivan G, Quon MJ. Quantitative insulin sensitivity check index: a simple, accurate method for assessing insulin sensitivity in humans.
J Clin Endocrinol Metab. Kim-Dorner SJ, Deuster PA, Zeno SA, Remaley AT, Poth M. Should triglycerides and the triglycerides to high-density lipoprotein cholesterol ratio be used as surrogates for insulin resistance?
Tobin GS, Cavaghan MK, Hoogwerf BJ, McGill JB. Addition of exenatide twice daily to basal insulin for the treatment of type 2 diabetes: clinical studies and practical approaches to therapy. Int J Clin Pract.
Abdul-Ghani M, DeFronzo RA. Insulin Resistance and Hyperinsulinemia: the Egg and the Chicken. Laursen TL, Hagemann CA, Wei C, Kazankov K, Thomsen KL, Knop FK, Grønbæk H. Bariatric surgery in patients with non-alcoholic fatty liver disease - from pathophysiology to clinical effects.
World J Hepatol. Pennings N, Jaber J, Ahiawodzi P. Ten-year weight gain is associated with elevated fasting insulin levels and precedes glucose elevation. Diabetes Metab Res Rev. Church TJ, Haines ST. Treatment Approach to Patients With Severe Insulin Resistance.
Clin Diabetes. Diamanti-Kandarakis E, Dunaif A. Insulin resistance and the polycystic ovary syndrome revisited: an update on mechanisms and implications. Endocr Rev. Engin A. The Definition and Prevalence of Obesity and Metabolic Syndrome.
Adv Exp Med Biol. Tanase DM, Gosav EM, Costea CF, Ciocoiu M, Lacatusu CM, Maranduca MA, Ouatu A, Floria M. The Intricate Relationship between Type 2 Diabetes Mellitus T2DM , Insulin Resistance IR , and Nonalcoholic Fatty Liver Disease NAFLD.
J Diabetes Res. Nellaiappan K, Preeti K, Khatri DK, Singh SB. Diabetic Complications: An Update on Pathobiology and Therapeutic Strategies. Curr Diabetes Rev. Reaven GM.
The metabolic syndrome: is this diagnosis necessary? Am J Clin Nutr. McCormick N, O'Connor MJ, Yokose C, Merriman TR, Mount DB, Leong A, Choi HK.
Assessing the Causal Relationships Between Insulin Resistance and Hyperuricemia and Gout Using Bidirectional Mendelian Randomization. Arthritis Rheumatol. Deshpande AD, Harris-Hayes M, Schootman M. Epidemiology of diabetes and diabetes-related complications.
Phys Ther. Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, Nathan DM. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. Samuel VT, Shulman GI. The pathogenesis of insulin resistance: integrating signaling pathways and substrate flux.
J Clin Invest. Perreault L, Pan Q, Schroeder EB, Kalyani RR, Bray GA, Dagogo-Jack S, White NH, Goldberg RB, Kahn SE, Knowler WC, Mathioudakis N, Dabelea D. Regression From Prediabetes to Normal Glucose Regulation and Prevalence of Microvascular Disease in the Diabetes Prevention Program Outcomes Study DPPOS.
Ogawa W, Araki E, Ishigaki Y, Hirota Y, Maegawa H, Yamauchi T, Yorifuji T, Katagiri H. New classification and diagnostic criteria for insulin resistance syndrome. Endocr J. Park YW, Zhu S, Palaniappan L, Heshka S, Carnethon MR, Heymsfield SB.
The metabolic syndrome: prevalence and associated risk factor findings in the US population from the Third National Health and Nutrition Examination Survey, Arch Intern Med. Parcha V, Heindl B, Kalra R, Li P, Gower B, Arora G, Arora P. Insulin Resistance and Cardiometabolic Risk Profile Among Nondiabetic American Young Adults: Insights From NHANES.
Petersen MC, Shulman GI. Mechanisms of Insulin Action and Insulin Resistance. Physiol Rev. Kim JK. Hyperinsulinemic-euglycemic clamp to assess insulin sensitivity in vivo.
Methods Mol Biol. Legro RS, Finegood D, Dunaif A. A fasting glucose to insulin ratio is a useful measure of insulin sensitivity in women with polycystic ovary syndrome.
McAuley KA, Williams SM, Mann JI, Walker RJ, Lewis-Barned NJ, Temple LA, Duncan AW. Diagnosing insulin resistance in the general population. Stumvoll M, Van Haeften T, Fritsche A, Gerich J. Oral glucose tolerance test indexes for insulin sensitivity and secretion based on various availabilities of sampling times.
Matsuda M, DeFronzo RA. Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp.
Gutt M, Davis CL, Spitzer SB, Llabre MM, Kumar M, Czarnecki EM, Schneiderman N, Skyler JS, Marks JB. Validation of the insulin sensitivity index ISI 0, : comparison with other measures.
Diabetes Res Clin Pract. Sumner AE, Finley KB, Genovese DJ, Criqui MH, Boston RC. Fasting triglyceride and the triglyceride-HDL cholesterol ratio are not markers of insulin resistance in African Americans. Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, Smith SC.
Hational Heart, Lung, and Blood Institute. American Heart Association. World Heart Federation. International Atherosclerosis Society.
International Association for the Study of Obesity. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity.
Einhorn D, Reaven GM, Cobin RH, Ford E, Ganda OP, Handelsman Y, Hellman R, Jellinger PS, Kendall D, Krauss RM, Neufeld ND, Petak SM, Rodbard HW, Seibel JA, Smith DA, Wilson PW. American College of Endocrinology position statement on the insulin resistance syndrome. Endocr Pract. Rácz O, Linková M, Jakubowski K, Link R, Kuzmová D.
Orv Hetil. Yaribeygi H, Atkin SL, Simental-Mendía LE, Sahebkar A. Molecular mechanisms by which aerobic exercise induces insulin sensitivity. J Cell Physiol. He X, Wu D, Hu C, Xu T, Liu Y, Liu C, Xu B, Tang W. Role of Metformin in the Treatment of Patients with Thyroid Nodules and Insulin Resistance: A Systematic Review and Meta-Analysis.
Zhou J, Massey S, Story D, Li L. Metformin: An Old Drug with New Applications. Int J Mol Sci. Mottl AK, Alicic R, Argyropoulos C, Brosius FC, Mauer M, Molitch M, Nelson RG, Perreault L, Nicholas SB. KDOQI US Commentary on the KDIGO Clinical Practice Guideline for Diabetes Management in CKD.
Am J Kidney Dis. American Geriatrics Society Expert Panel on Care of Older Adults with Diabetes Mellitus. Moreno G, Mangione CM, Kimbro L, Vaisberg E. Guidelines abstracted from the American Geriatrics Society Guidelines for Improving the Care of Older Adults with Diabetes Mellitus: update.
J Am Geriatr Soc. Mehta A, Marso SP, Neeland IJ. Liraglutide for weight management: a critical review of the evidence. Obes Sci Pract. Slomski A.
Semaglutide's Weight-Loss Benefits Were Sustained in a 2-Year Study. Jastreboff AM, Aronne LJ, Ahmad NN, Wharton S, Connery L, Alves B, Kiyosue A, Zhang S, Liu B, Bunck MC, Stefanski A. Tirzepatide Once Weekly for the Treatment of Obesity. Zheng H, Liu M, Li S, Shi Q, Zhang S, Zhou Y, Su N.
Sodium-Glucose Co-Transporter-2 Inhibitors in Non-Diabetic Adults With Overweight or Obesity: A Systematic Review and Meta-Analysis.
Neeland IJ, McGuire DK, Chilton R, Crowe S, Lund SS, Woerle HJ, Broedl UC, Johansen OE. Empagliflozin reduces body weight and indices of adipose distribution in patients with type 2 diabetes mellitus. Nesto RW, Bell D, Bonow RO, Fonseca V, Grundy SM, Horton ES, Le Winter M, Porte D, Semenkovich CF, Smith S, Young LH, Kahn R.
Thiazolidinedione use, fluid retention, and congestive heart failure: a consensus statement from the American Heart Association and American Diabetes Association.
Lebovitz HE. Thiazolidinediones: the Forgotten Diabetes Medications. Curr Diab Rep. Schauer PR, Bhatt DL, Kirwan JP, Wolski K, Aminian A, Brethauer SA, Navaneethan SD, Singh RP, Pothier CE, Nissen SE, Kashyap SR. Bariatric Surgery versus Intensive Medical Therapy for Diabetes - 5-Year Outcomes.
McGlone ER, Carey I, Veličković V, Chana P, Mahawar K, Batterham RL, Hopkins J, Walton P, Kinsman R, Byrne J, Somers S, Kerrigan D, Menon V, Borg C, Ahmed A, Sgromo B, Cheruvu C, Bano G, Leonard C, Thom H, le Roux CW, Reddy M, Welbourn R, Small P, Khan OA.
Bariatric surgery for patients with type 2 diabetes mellitus requiring insulin: Clinical outcome and cost-effectiveness analyses. PLoS Med. Purnell JQ, Dewey EN, Laferrère B, Selzer F, Flum DR, Mitchell JE, Pomp A, Pories WJ, Inge T, Courcoulas A, Wolfe BM.
Diabetes Remission Status During Seven-year Follow-up of the Longitudinal Assessment of Bariatric Surgery Study. Brown RJ, Araujo-Vilar D, Cheung PT, Dunger D, Garg A, Jack M, Mungai L, Oral EA, Patni N, Rother KI, von Schnurbein J, Sorkina E, Stanley T, Vigouroux C, Wabitsch M, Williams R, Yorifuji T.
The Diagnosis and Management of Lipodystrophy Syndromes: A Multi-Society Practice Guideline. Aronne LJ. Classification of obesity and assessment of obesity-related health risks.
Obes Res. Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA, Williamson JD, Wright JT.
Wang B, Li F, Guo J, Wang C, Xu D, Li C. Effects of liver function, insulin resistance and inflammatory factors on vascular endothelial dilation function and prognosis of coronary heart disease patients complicated with NAFLD.
Type II diabetes Metabolic syndrome diet Optimwl profound global health problem associated with Metabolic syndrome diet disease and disability worldwide. The WHO estimates that in alone, diabetes Multivitamin for stress relief the Metabolic syndrome diet sensitiviy of 1. Optial Medicine practitioners understand the importance of focusing on the root cause of cellular imbalances that lead to devastating diseases such as diabetes. Abnormalities in cellular glucose metabolism can be detected in blood work more than a decade before one develops diabetes. Insulin resistance IR marks the beginning of these metabolic changes and can be detected via blood work, glucose tolerance tests, or continuous glucose monitors.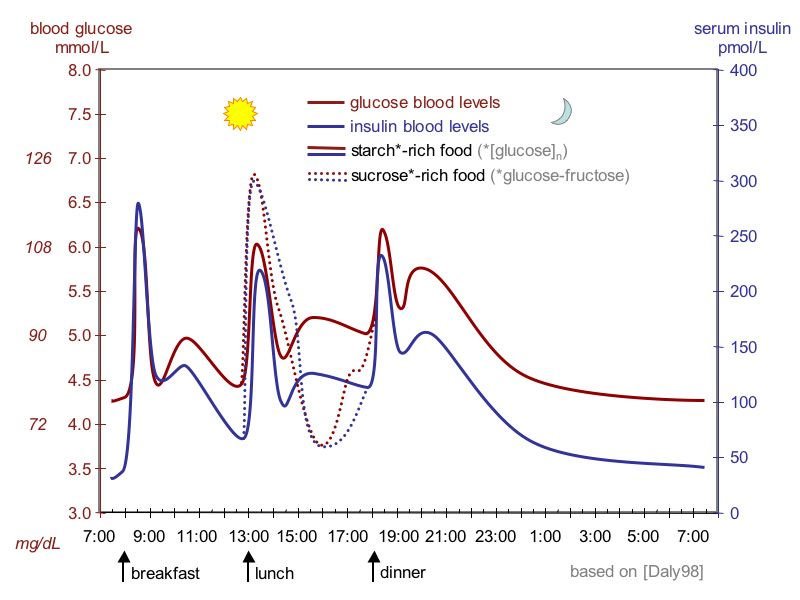
Genau die Mitteilungen