
Video
Mineral (Nutrition) Macro \u0026 Trace - Functions \u0026 Sources - Human body Stephanie Ostrenga, Michigan State University Extension - January 30, Muscle recovery foods introduction Micronutrrient understanding Micronutrieng bioavailability of micronutrients. The term Restorative post-workout nutrition refers absorpton the proportion Hydration and its impact on health fraction Microonutrient a nutrient, consumed in the diet, that is absorbed Mcironutrient utilized by the body. According to a micronutrient lecture by Dr. Suzanne Cole at the University of Michigan, bioavailability is influenced by several factors including diet, nutrient concentration, nutritional status, health, and life-stage. Diet-related factors affecting foods include the structure of food, the chemical form of a particular nutrient, interactions between various nutrients and foods, and the processing or treatment of a particular food. One example of food structure influencing bioavailability or the utilization of nutrients is with plant foods.Micronutrient absorption factors -
However, phytic acid is also labeled an antinutrient because humans lack the phytase enzyme needed to break it down. As it passes through the gut, phytic acid binds to minerals like iron , zinc , and calcium so they are not well-absorbed in the intestine. This will occur only when phytic acid is eaten with foods containing these minerals at the same meal.
The average Western diet usually has enough nutrients and variety to protect from a true deficiency, especially with the inclusion of some animal proteins e. A nutrient deficiency more likely occurs in developing countries where a variety of food choices is limited, the risk of malnutrition is higher, and legumes or whole grains are staples that are eaten with every meal.
How you prepare foods high in phytic acid can reduce the overall amount. Cooking, soaking overnight in water, sprouting germination , fermentation, and pickling can all break down phytic acid so that the phosphorus can be released and absorbed by the body. Some natural bacteria in the colon contain the enzyme phytase and can also help to break it down.
Only those already at risk for nutrient deficiencies of the minerals mentioned or those who eat only plant foods such as vegans may need to consider reducing phytic acid in the diet.
The tricky part is that many healthful plant foods are rich in oxalates including certain green leafy vegetables spinach, Swiss chard , beets, beans, certain nuts almonds , rice bran, and potatoes.
After we eat food, the body uses what it needs for energy. Some of the remaining food components not needed are shuttled to the kidneys to be excreted in urine. If there is too much waste and not enough liquid, tiny crystals can form.
If there is not enough liquid or urine to flush them out, a high amount of oxalates in the urine can form crystals by attaching to calcium. Sometimes the crystals clump together to form a stone that is painful when it moves to pass. However, avoiding dietary oxalate is not the only or best way to avoid kidney stones.
It is important to drink enough fluids, especially water, to dilute the urine so that substances like oxalates do not collect and stick together. Eating calcium-rich foods at the same time as oxalate-rich foods can also help, as the oxalates will bind to calcium in the stomach, preventing the oxalate from being absorbed into the body.
An example is to drink calcium-fortified milk or plant milk with a meal or snack that contains beans, spinach, or nuts. But higher calcium intakes in men were also found to be significantly protective from developing stones. A follow-up review of the NHS confirmed that higher calcium intakes were protective from kidney stones in women.
Therefore, a dietary strategy to prevent kidney stones is more complex than just avoiding oxalates. For those at risk, drink plenty of water every day, eat enough calcium from foods, and eat low amounts of oxalate-rich foods taken with calcium-rich foods.
Always inform your doctor about any dietary changes that are made for health reasons. The contents of this website are for educational purposes and are not intended to offer personal medical advice.
You should seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
The Nutrition Source does not recommend or endorse any products. Skip to content The Nutrition Source. The Nutrition Source Menu. Search for:. A meta-analysis of four prospective cohort studies , including nearly , older adults, found that high dietary intakes of retinol and high retinol blood concentrations were associated with increased risk of hip fracture but not total fractures This analysis also found an increased risk with low concentrations of blood retinol Only excessive intakes of retinol, not β-carotene provitamin A , have been associated with adverse effects on bone health.
For more information, see the article on Vitamin A. Moderately elevated iron stores may be much more common than iron deficiency in older individuals Dietary iron requirements decrease in women following menopause due to the cessation of menstrual blood loss and iron being efficiently recycled by the body.
Moreover, hereditary hemochromatosis is not uncommon in the US population, and the effects of long-term dietary iron excess on chronic disease risk are not yet clear. For these reasons, it is generally recommended that older adults should not take dietary supplements containing iron unless they have been diagnosed with iron deficiency.
As with other age groups in the US, the concern for sodium is excessive intake in older adults. Because the sensitivity to the blood pressure-raising effect of salt increases with age, sodium reduction in the context of a healthful dietary pattern is especially important for older adults, who are at increased risk of high blood pressure , cardiovascular disease , and kidney disease.
More information on the adverse health effects of excessive sodium intake can be found in the article on Sodium. NOTE: In this article, average intakes in the US are compared to the Dietary Reference Intakes DRIs that were set in In , the National Academy of Medicine NAM established new DRIs: an AI for sodium see the article on Sodium and a Chronic Disease Risk Reduction Intake for sodium see the article on Sodium.
The NAM did not set a UL for details, see the article on Sodium. Similar to other age groups, older adults in the US are not meeting daily intake recommendations for potassium: only 1. The richest sources of potassium are fruit and vegetables — older men and women fall short of reaching the recommended intakes of both fruit and vegetables High-potassium diets have been associated with a lower risk of stroke , hypertension , osteoporosis , and kidney stones for more information, see the article on Potassium.
Several foods are listed in Table 3 , along with their potassium content in milligrams. NOTE: In , the National Academy of Medicine established a new AI for potassium see the article on Potassium. Any diet that eliminates entire food groups has the potential for being inadequate in several micronutrients.
Those who adhere to a vegan diet, which excludes all foods of animal origin, are at increased risk for select micronutrient deficiencies and inadequacies, especially vitamin B 12 , but also vitamin D, calcium, and potentially iodine, iron, and zinc. Vegetarians who consume dairy and eggs may also be at a heightened risk of certain micronutrient inadequacies, particularly iron and zinc.
Because vitamin B 12 is found only in foods of animal origin, a vegan diet will result in vitamin B 12 deficiency — and devastating neurologic consequences — unless there is intake from fortified food or supplements.
Few plant-source foods, including certain fermented beans and vegetables and edible algae and mushrooms, may contain substantial amounts of vitamin B 12 Together with B-vitamin fortified food and supplements, these foods may contribute, although modestly, to prevent vitamin B 12 deficiency in individuals consuming vegetarian or vegan diets.
Another large cohort in the US and Canada, the Adventist Health Study 2, assessed nutrient intake among more than 71, participants of which 5, were vegans This study found an average daily intake of 6.
Adequate status of vitamin D is needed for optimal bone health. Other studies have found that intake of calcium — another nutrient essential for bone health — is a concern for vegans 60, While dairy is an important source of calcium, some plant foods are good sources of bioavailable calcium.
The calcium in foods of the kale family broccoli, bok choy, cabbage, mustard, and turnip greens is as bioavailable as that found in milk. However, other plant-based foods contain components that inhibit the absorption of calcium.
Oxalic acid oxalate is the most potent inhibitor of calcium absorption and is found at high concentrations in spinach and rhubarb and at lower concentrations in sweet potatoes and dried beans. Phytic acid phytate — found in whole grains , legumes , and cereal 62 — can also inhibit calcium absorption but to a lesser extent than oxalic acid see the article on Calcium.
Fortified food can contribute substantially to total daily calcium and vitamin D intake, although the availability of fortified food varies by country.
Nutrient intake assessments also differ among studies and can account for variation. Of note, a vegan-specific food frequency questionnaire has recently been developed Limited data also suggest that vegans may be at risk of inadequate iodine intake: A small US cross-sectional study in 63 vegans reported a median urinary iodine concentration of The US population is currently considered to be iodine-sufficient, but vegans and other subpopulations, e.
While vegans and vegetarians may have similar iron and zinc intake compared to omnivores, the bioavailability of these two minerals is lower from plant versus animal sources. Iron from plants, i. Yet, a diet that excludes meat does not appear to be associated with an increased risk of iron deficiency when it includes whole grains, legumes, nuts , seeds, dried fruit, iron-fortified cereal, and green leafy vegetables Absorption of nonheme iron is influenced by various dietary factors see HIGHLIGHT ; for references and more information, see the article on Iron.
In a systematic review and meta-analysis of 26 studies, vegetarians had lower dietary intakes and serum zinc concentrations compared to non-vegetarians; a secondary analysis found this association was stronger among vegans However, it is important to note that measuring circulating zinc levels has some limitations e.
Compared to animal sources, zinc bioavailability from plant sources e. The enzymatic action of yeast reduces the level of phytic acid in food 69 , and leavened whole-grain bread therefore has more bioavailable zinc than unleavened whole-grain bread.
High levels of dietary calcium impair zinc absorption in animals, but it is uncertain whether this occurs in humans for more information, see the article on Zinc. Gluten-free grain products are often subject to a milling process that removes the bran and the germ layers of the grain; this refining process strips out fiber and other nutrients.
Moreover, these products may not be enriched or fortified with micronutrients like is typically done with refined wheat products. Gluten-free diets may therefore not supply sufficient amounts of certain vitamins and essential minerals, especially thiamin, riboflavin, niacin, folate, and iron 70, Several micronutrient inadequacies, including folate, vitamin B 12 , vitamin D, calcium, magnesium, iron, and zinc, have been reported in patients treated for Celiac disease , an autoimmune condition that requires avoidance of dietary gluten However, these inadequacies may in part be due to the underlying pathological condition rather than nutritional quality of the diet.
Celiac disease patients are known to display a number of micronutrient deficiencies at the time of diagnosis 73, Diets that exclude iodized salt, fish, and seaweed have been found to contain very little iodine Additionally, certain energy-restricted diets used for weight loss, especially if followed long term, may place individuals at increased risk of micronutrient deficiencies.
One study found that adherence to various weight-loss diets for just eight weeks resulted in a higher prevalence of inadequate micronutrient intakes at eight weeks compared to baseline In particular, micronutrient intake significantly decreased in those who followed the Atkins thiamin, folate, vitamin C, iron, magnesium , LEARN L ifestyle, E xercise, A ttitudes, R elationships, N utrition; thiamin, vitamin E, calcium, magnesium , or Ornish vitamin B 12 , vitamin E, zinc diets Alcoholics are at increased risk for deficiency of several micronutrients, especially vitamin A and the B vitamins.
Chronic alcohol consumption results in depletion of liver stores of vitamin A and may contribute to alcohol-induced liver damage cirrhosis 79, Moreover, the liver toxicity of preformed vitamin A retinol is enhanced by chronic alcohol consumption, thus narrowing the therapeutic window for vitamin A supplementation in alcoholics It is well established that alcoholics are at a heightened risk for inadequate status of many B vitamins, including thiamin, riboflavin, niacin, vitamin B 6 , folate, and vitamin B B vitamins are important in various aspects of energy metabolism in various tissues, including the brain see the article on Cognitive Function ; thus, deficiencies in several B vitamins can cause cognitive disorders.
Wernicke-Korsakoff syndrome WKS , a neuropsychiatric disorder resulting from thiamin deficiency, is common among those who chronically abuse alcohol. Symptoms of WKS include learning deficits, amnesia, eye-movement and gait disorders, disorientation, and confabulation.
Moreover, WKS is one of the more common causes of dementia In alcoholics, general malnutrition, decreased intestinal absorption, impaired phosphorylation of thiamin, and increased urinary excretion may all contribute to thiamin deficiency 82, Administration of intravenous thiamin to WKS patients generally results in prompt improvement of the eye symptoms, but improvements in motor coordination and memory may be less, depending on how long the symptoms have been present and the WKS stage at the time of intervention.
Evidence of increased immune cell activation and increased free radical production in the areas of the brain that are selectively damaged suggests that oxidative stress plays an important role in the neurologic pathology of thiamin deficiency Taken together, alcoholics have an increased requirement for thiamin.
Moreover, alcoholics are at increased risk for riboflavin deficiency due to decreased intake, decreased absorption, and impaired utilization of riboflavin.
In rats chronically fed alcohol, the inhibition of riboflavin transporters caused impairment in intestinal absorption and renal re-uptake of the vitamin A combination of low dietary intakes and impaired vitamin metabolism appear to place alcoholics at a higher risk for deficiencies in niacin 86 , vitamin B 6 86 , folate 87 , vitamin B 12 88 , and zinc Exposure to toxins in cigarette smoke causes oxidative damage to indispensable molecules in the body, i.
Along with other cellular antioxidants , vitamins C and E play important roles to protect against the oxidative damage caused by exposure to smoke. Smokers generally have lower vitamin C status than nonsmokers due to increased metabolic turnover and thus require more from their diets Vitamin C is capable of regenerating the antioxidant capacity of α-tocopherol, the form of vitamin E with the greatest nutritional significance see Figure 1 The main function of α-tocopherol is to function as a fat-soluble antioxidant, protecting cell membranes from lipid peroxidation.
Oxidative stress caused by smoking is thought to increase the utilization of α-tocopherol such that smokers might be at increased risk of deficiency compared with nonsmokers In a double-blind , placebo -controlled trial in 11 smokers and 13 nonsmokers given α-tocopherol and γ-tocopherol that was labeled with deuterium hence traceable , supplementation with vitamin C reduced the rate of vitamin E loss in plasma , likely by regenerating tocopheryl radicals back to nonoxidized forms Thus, smokers should ensure adequate intake of both vitamins C and E.
Food insecurity i. Some US cross-sectional studies have linked food insecurity with iron-deficiency anemia in young children 97, Additionally, US national surveys NHANES have associated food insecurity with iron-deficiency anemia among adolescents ages years 99 and with insufficient iron stores low ferritin among pregnant females nutritional quality and thereby more resembling the concept of hunger This survey also found lower serum concentrations of vitamin A among both younger and older adults and vitamin E older adults only in those of food-insufficient households compared to food-sufficient households; yet, the mean concentrations for these micronutrients were above the cutoffs typically associated with even marginal deficiency In another analysis of data from NHANES III, old ages years food-insufficient individuals had lower intakes of several micronutrients compared to those who were classified as food-sufficient However, both groups had average micronutrient intakes above the EAR with the exception of magnesium, in which intakes were lower than the requirement in both groups Lower socioeconomic status has been linked to lower intakes of micronutrients, including most of the 'shortfall' nutrients NHANES Differences in micronutrient intakes between low and high socioeconomic status might be attributed to differences in food security, food diversity, and use of supplements In addition, the Seattle Obesity Study men and women found a direct link between the price of food and the level of micronutrient intake In this study, intakes of vitamin C, vitamin E, β-carotene, potassium, and magnesium — nutrients abundant in fruit and vegetables and their oils — were directly associated with a higher socioeconomic status Obesity is associated with an increased risk of a number of chronic diseases , including high blood pressure , type 2 diabetes mellitus , liver and gallbladder disease, osteoarthritis , sleep apnea , and certain cancers.
Although multifactorial in etiology , obesity is linked with consumption of an energy-dense, nutrient-poor diet. Obese individuals generally consume excessive calories i. In particular, it is well established that obesity increases the risk of vitamin D deficiency. Once vitamin D is synthesized in the skin or ingested, it can be sequestered in body fat stores, making it less bioavailable to people with higher body fat mass see the article on Vitamin D.
Accordingly, the prevalence of inadequacy for vitamins A, C, D, and E; calcium; and magnesium was higher among obese individuals compared to those of normal weight, and additionally, the proportion of obese adults that met the AI for potassium was smaller compared to normal-weight adults As mentioned above, morbidly obese individuals have preexisting micronutrient deficiencies before they undergo bariatric surgery.
Bariatric weight-loss surgery to treat morbid obesity can further increase the risk of micronutrient deficiencies due to decreased food intake and surgical alteration of the gastrointestinal tract.
Most micronutrients are absorbed in the upper small intestine , which is often removed or bypassed in certain types of bariatric surgeries, and gastric , biliary , and pancreatic secretions are important for nutrient absorption While the recommendations for nutrient supplementation vary by the specific type of surgery e.
Supplementation with other micronutrients, including thiamin; vitamins A, B 12 , C, and K; iron; zinc; and possibly others may be needed depending on the specific type of surgical procedure Nutritional evaluation and counseling of the patient must be done prior to and following bariatric surgery, and supplemental micronutrient recommendations should be tailored to individual needs Most micronutrients are absorbed in the upper small intestine duodenum and jejunum , although some nutrients e.
The causes of malnutrition in IBD patients are multifactorial and include 1 reduced food intake and avoidance of certain foods or food groups; 2 impaired micronutrient absorption e.
IBD patients have been reported to experience deficiencies in multiple micronutrients; the below discussion includes the more commonly reported deficiencies that have clinical relevance.
Deficiencies or inadequacies in other micronutrients not discussed may also be present in IBD patients. However, the exact prevalence is difficult to estimate because the typically reliable measures of iron status , like serum ferritin an iron-storage protein that is an acute-phase reactive protein , are affected by inflammation.
While other measures of iron status transferrin saturation, soluble transferrin receptor are often assessed in IBD patients, the diagnosis of iron deficiency is made using serum ferritin in the absence or presence of inflammation.
The most severe level of iron deficiency is iron-deficiency anemia see the article on Iron. IBD disease activity has also been positively associated with the degree of anemia.
Thus, it is prudent that iron status be monitored in IBD patients and, when necessary, treated with iron supplementation Iron may also be administered parenterally reviewed in Vitamin B 12 , complexed to intrinsic factor, is absorbed by a receptor -mediated process in the ileum — the distal section of the small intestine.
Vitamin B 12 status in IBD patients should be monitored by assessing blood concentration of methylmalonic acid, the specific indicator of vitamin B 12 deficiency; assessing blood concentration of homocysteine may also be useful in assessing vitamin B 12 status in IBD patients However, many studies on the association have employed serum folate concentration, an indicator of only recent dietary folate intake, to assess body folate status.
Red blood cell folate concentration better reflects tissue folate stores and body folate status Use of certain medications may cause folate deficiency. In particular, patients taking the pharmaceuticals sulfasalazine an inhibitor of the reduced folate carrier that mediates cellular uptake, which is used to treat rheumatoid arthritis and ulcerative colitis or methotrexate a tetrahydrofolate reductase inhibitor and folate antagonist used to treat cancer , rheumatoid arthritis, and psoriasis are at increased risk of folate deficiency , and should follow the advice of their physician or pharmacist regarding supplemental folic or folinic acid.
IBD patients are at a heightened risk of low bone mineral density , osteoporosis , and osteopenia Adequate intake of calcium is critical throughout life to maintain bone health; dietary calcium intake is low in the US population, and calcium is considered a nutrient of public health concern However, the efficacy of calcium supplementation to prevent bone loss in IBD patients has not been examined in long-term intervention trials.
Ecologic studies have found a higher prevalence of IBD in populations residing in temperate climates compared to those living near the equator reviewed in , suggesting that IBD may be linked to vitamin D inadequacy.
While additional studies are needed to confirm the therapeutic efficacy of vitamin D in IBD, vitamin D supplementation is commonly recommended to decrease disease activity and relapse and improve bone mineral density in IBD patients Regarding drug interactions, the Endocrine Society recommends monitoring vitamin D status of patients treated with glucocorticoids because these medications increase the catabolism of hydroxyvitamin D 5.
Vitamin D supplementation is typically recommended in IBD patients treated with corticosteroids. Serum or plasma concentration of zinc is typically used in studies to assess zinc status , but measuring blood concentration is not a sensitive indicator of marginal deficiency.
Blood concentrations of zinc are also known to be depressed in inflammatory states ; therefore, studies assessing circulating concentrations of zinc in IBD patients are difficult to interpret.
Persistent diarrhea contributes to zinc deficiency, and zinc supplementation may be needed in patients with significant and chronic diarrhea Micronutrient insufficiencies are common in dialysis patients for several reasons, including reduced appetite, restricted diets e. Medications may also interfere with nutrient absorption, and the uremia may alter metabolism.
Moreover, the increased oxidative stress and chronic inflammation experienced by dialysis patients may require increased intake of certain micronutrients, such as antioxidants e.
Multivitamin supplements that are specifically formulated for dialysis patients are available; these usually contain higher amounts of B vitamins thiamin, vitamin B 6 , folic acid, vitamin B 12 and vitamin C to compensate for losses of these micronutrients during the dialysis procedure.
Such multivitamins do not contain vitamin A because vitamin A status is increased in dialysis patients, and supplementation with this vitamin may lead to toxicity in this patient population Certain B vitamins are needed to decrease blood concentrations of homocysteine in dialysis patients; elevated levels of homocysteine are a risk factor for cardiovascular disease and possibly dementia.
Additionally, vitamin C intake is generally low in dialysis patients as low-potassium diets are often low in vitamin C. Vitamin D is another micronutrient of concern: Vitamin D status is reportedly low in dialysis patients, and patients with kidney disease have been traditionally given the active form of vitamin D 1,dihydroxyvitamin D or a vitamin D analog Mineral intake and status of dialysis patients should also be closely monitored as patients are at risk of both deficiency and excess of certain minerals and trace elements Certain medications can affect micronutrient status by altering nutrient absorption or utilization, and conversely, some micronutrients — from food or supplements — can alter the pharmacokinetics or pharmacodynamics of certain drugs , Older individuals are especially susceptible to drug-nutrient interactions due to impaired metabolism , increased risk of malnutrition, and prevalent use of prescription drugs Physicians, pharmacists, and dietitians need to consider potential drug-nutrient interactions and recommend ways to prevent adverse effects Some medications should be taken with a meal to maximize drug bioavailability , while others should be taken in a fasting state — refer to the patient information leaflet accompanying the medication or consult a pharmacist for specific instructions.
Although drug-nutrient interactions have not been systematically studied, there are a number of known interactions reported in the scientific literature. The list below is not meant to be comprehensive but includes some of the more common clinically relevant drug-nutrient interactions, especially because they may result in micronutrient inadequacy.
For more comprehensive lists, see the suggested references. Long-term use of the drug is often needed to reach such a threshold and for clinical symptoms of the drug-nutrient interaction to manifest For information regarding drug interactions with a particular micronutrient, see the "Drug interactions" section in the separate articles on the individual vitamins and minerals links included in Table 6 below , as well as the suggested references.
Antacids are commonly used to neutralize stomach acid and thus to treat heartburn and indigestion; proton-pump inhibitors e. Use of these medications may alter nutrient absorption such that intake may need to be separated from food or supplemental intake by two to three hours.
Although data are limited, use of antacids or gastric acid suppressants might slightly impair absorption of folate from supplemental folic acid Separating folic acid supplementation by drug use by three hours would avoid any potential interaction.
Proton-pump inhibitors markedly decrease stomach acid secretion required for the release of vitamin B 12 from food but not from supplements. Long-term use of proton-pump inhibitors has been found to decrease blood vitamin B 12 concentrations. However, vitamin B 12 deficiency does not generally develop until after at least three years of continuous therapy , Use of histamine H 2 - receptor antagonists has also been found to decrease the absorption of vitamin B 12 from food.
It is not clear whether the long-term use of H 2 -receptor antagonists could cause overt vitamin B 12 deficiency , Individuals taking drugs that inhibit gastric acid secretion should consider taking vitamin B 12 in the form of a supplement because gastric acid is not required for its absorption.
Hypercalcemia has been initially reported with the consumption of large quantities of calcium supplements in combination with antacids, particularly in the days when peptic ulcers were treated with large quantities of milk, calcium carbonate antacid , and sodium bicarbonate absorbable alkali.
This condition is termed calcium-alkali syndrome formerly known as milk-alkali syndrome and has been associated with calcium supplement levels from 1.
Since the treatment for peptic ulcers has evolved and because of the widespread use of over-the-counter calcium supplements, the demographic of this syndrome has changed such that those at greater risk are now postmenopausal women, pregnant women, transplant recipients, patients with bulimia, and patients on dialysis , rather than men with peptic ulcers reviewed in Aluminum-containing antacids can decrease the absorption of fluoride.
It is best to take these products two hours before or after fluoride supplements Medications that decrease stomach acidity, such as antacids, histamine H 2 receptor antagonists e. Symptoms of magnesium toxicity, including nausea, vomiting, respiratory problems, and heart block, have occurred in people with impaired kidney function taking magnesium-containing antacids Magnesium-containing antacids may decrease the absorption of manganese if taken together with manganese-containing foods or supplements Aluminum-containing antacids reduce the absorption of dietary phosphorus by forming aluminum phosphate, which cannot be absorbed by the body.
When consumed in high doses, aluminum-containing antacids can lead to abnormally low blood phosphorus concentration hypophosphatemia , as well as aggravate phosphorus deficiency due to other causes The reduction of stomach acidity by proton-pump inhibitors may also limit the efficacy of phosphate-binder therapy in patients with kidney failure A number of antibiotics can affect micronutrient absorption, or conversely, certain micronutrients — from food or supplements — may affect absorption or efficacy of some antibiotics.
Table 4 lists some of the known micronutrient-antibiotic interactions; however, this list is not comprehensive. Some oral anticoagulants , such as warfarin Coumadin, Jantoven , inhibit coagulation by antagonizing the action of vitamin K. Warfarin prevents recycling of vitamin K by blocking the enzyme , vitamin K oxidoreductase, thereby creating a functional vitamin K deficiency.
Low dietary intakes of vitamin K can cause an unstable international normalized ratio INR Daily phylloquinone vitamin K 1 supplements of up to µg are considered safe for patients taking warfarin, but therapeutic anticoagulant stability may be undermined by daily doses of menaquinone-7 a form of vitamin K 2 as low as 10 to 20 µg Large supplemental doses of vitamin E may inhibit vitamin K-dependent carboxylase activity and interfere with the coagulation cascade Thus, the use of vitamin E supplements may increase the risk of bleeding in individuals taking warfarin and other anticoagulant drugs, as well as antiplatelet drugs and non-steroidal anti-inflammatory drugs NSAIDs like aspirin, ibuprofen, and others.
There is some evidence from case reports , though limited and controversial, that large oral doses of vitamin C may inhibit the action of warfarin , , requiring an increase in warfarin dose to maintain its effectiveness.
Pharmacologic doses of potassium iodide may decrease the anticoagulant effect of warfarin High intakes of other nutrients or phytochemicals may affect platelet aggregation and coagulation.
See Table 5 for links to the "Drug interactions" section in articles on individual nutrients, phytochemicals, or foods; this list is not meant to be comprehensive. See the Natural Medicines database or the text, PDR for Nutritional Supplements , for more detailed information. Individuals on long-term anticonvulsant anti- seizure therapy, including primidone Mysoline , phenytoin Dilantin , and carbamazepine Carbatrol, Tegretol , have been found to have reduced blood biotin concentrations, as well as an increased urinary excretion of organic acids e.
Potential mechanisms for these effects may include inhibition of biotin intestinal absorption, decreased renal reabsorption, and increased biotin catabolism Use of the anticonvulsant valproic acid in children has resulted in hair loss reversed by biotin supplementation The anticonvulsant, phenytoin, has been shown to inhibit the intestinal absorption of folate, and several studies have associated decreased folate status with long-term use of the anticonvulsants, phenytoin, phenobarbital, and primidone However, few studies controlled for differences in dietary folate intake between anticonvulsant users and nonusers.
Reduced blood concentrations of thiamin have been reported in individuals with seizure disorders epilepsy taking the anticonvulsant medication, phenytoin, for long periods of time High doses of vitamin B 6 have been found to decrease the efficacy of two anticonvulsants, phenobarbital and phenytoin The following anticonvulsant medications increase the metabolism of vitamin D and may decrease serum hydroxyvitamin D concentrations: phenytoin, phenobarbital, carbamazepine, and primidone Use of the anticonvulsant drugs, phenobarbital, phenytoin, or carbamazepine, may lower plasma concentrations of vitamin E The prescription of anticonvulsants phenytoin, phenobarbital to pregnant or breast-feeding women may place the newborn at increased risk of vitamin K deficiency Use of the anticonvulsant drug, valproic acid, may lower circulating selenium concentrations Several micronutrients, including calcium, iron, magnesium, and zinc, can decrease absorption and thus efficacy of bisphosphonates e.
It may be best to take bisphosphonates at least two hours before or four to six hours after supplemental micronutrients or mineral-rich foods. Through increasing urinary flow, diuretics may prevent reabsorption of thiamin by the kidneys and increase its excretion in the urine Thus, the risk of thiamin deficiency is increased in diuretic-treated patients with marginal thiamin intake and in individuals receiving long-term, diuretic therapy.
Use of thiazide diuretics e. Prolonged use of some diuretics may increase urinary magnesium excretion and result in magnesium depletion Potassium-sparing diuretics e.
Loop and thiazide diuretics increase urinary excretion of potassium and may thus increase the risk of hypokalemia low blood concentrations of potassium.
Conversely, potassium-sparing diuretics e. Use of loop or thiazide diuretics may increase the risk of hyponatremia abnormally low blood concentrations of sodium Prolonged use of some diuretics may increase urinary zinc excretion and result in zinc depletion Co-administration of nicotinic acid with a lipid -lowering HMG-CoA reductase inhibitor i.
Rhabdomyolysis is relatively uncommon but increased in those who take HMG-CoA reductase inhibitors Some HMG-CoA reductase inhibitors, including atorvastatin, lovastatin, and simvastatin, are metabolized by cytochrome P CYP 3A4 enzymes.
Consumption of grapefruit inhibits intestinal CYP3A4; the compounds responsible for this effect are thought to be furanocoumarins, particularly dihydroxybergamottin.
Drugs with very low bioavailability like HMG-CoA reductase inhibitors are more likely to be toxic when CYP3A4 activity is inhibited; thus, for the HMG-CoA reductase inhibitors that utilize CYP3A4, consuming grapefruit increases the risk of rhabdomyolysis and other adverse effects of the drug.
One grapefruit or as little as mL 7 fluid ounces of grapefruit juice have been found to irreversibly inhibit intestinal CYP3A4 All forms of the fruit — freshly squeezed juice, frozen concentrate, or whole fruit — can potentially affect the activity of CYP3A4.
Some varieties of other citrus fruit Seville oranges, limes, and pomelos contain furanocoumarins and can also interfere with CYP3A4 activity see the article on Flavonoids. Methotrexate is a folate antagonist used to treat a number of diseases, including cancer , rheumatoid arthritis , and psoriasis.
Some of the side effects of methotrexate are similar to those of severe folate deficiency, and supplementation with folic or folinic acid leucovorin is used to reduce the antifolate toxicity , Nitrous oxide, a commonly used anesthetic, oxidizes and inactivates vitamin B 12 , thus inhibiting both of the vitamin B 12 -dependent enzymes , and can produce many of the clinical features of vitamin B 12 deficiency, such as megaloblastic anemia or neuropathy 43 , Some think that vitamin B 12 deficiency should be ruled out before using nitrous oxide While not considered nutrients, furanocoumarins — either from food e.
For information on such interactions, see the article on Flavonoids. Nutrients work together in the body to carry out its essential functions. However, a nutrient can interfere with the metabolism i. Table 7 lists some documented nutrient-nutrient interactions; more information on these interactions can be found in the individual nutrient articles follow the hyperlinks in the table.
Written in January by: Victoria J. Drake, Ph. Linus Pauling Institute Oregon State University. Reviewed in March by: Balz Frei, Ph. Former Director, Linus Pauling Institute Distinguished Professor Emeritus, Dept. of Biochemistry and Biophysics Oregon State University.
The writing of this article was supported by a grant from Pfizer Inc. Holick MF. Resurrection of vitamin D deficiency and rickets. J Clin Invest. Chen TC, Chimeh F, Lu Z, et al. Factors that influence the cutaneous synthesis and dietary sources of vitamin D.
Arch Biochem Biophys. Brenner M, Hearing VJ. The protective role of melanin against UV damage in human skin. Photochem Photobiol. Weishaar T, Rajan S, Keller B. J Am Board Fam Med. Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline.
J Clin Endocrinol Metab. Food and Nutrition Board, Institute of Medicine. Dietary reference intakes for adequacy: calcium and vitamin D. In: Ross AC, Taylor CL, Yaktine AL, Del Valle HB, eds. Dietary Reference Intakes for Calcium and Vitamin D. Washington, D. The National Academies Press. National Center for Environmental Health.
Division of Laboratory Sciences. Second national report on biochemical indicators of diet and nutrition in the US population Wagner CL, Greer FR, American Academy of Pediatrics Section on B, American Academy of Pediatrics Committee on N.
Prevention of rickets and vitamin D deficiency in infants, children, and adolescents. Dawodu A, Tsang RC. Maternal vitamin D status: effect on milk vitamin D content and vitamin D status of breastfeeding infants. Adv Nutr. Thiele DK, Senti JL, Anderson CM.
Maternal vitamin D supplementation to meet the needs of the breastfed infant: a systematic review. J Hum Lact. Wharton B, Bishop N. Banfield EC, Liu Y, Davis JS, Chang S, Frazier-Wood AC. Poor adherence to US dietary guidelines for children and adolescents in the National Health and Nutrition Examination Survey population.
J Acad Nutr Diet. Berner LA, Keast DR, Bailey RL, Dwyer JT. Fortified foods are major contributors to nutrient intakes in diets of US children and adolescents. What We Eat in America NHANES Total nutrient intakes: percent reporting and mean amounts of selected vitamins and minerals from food and beverages and dietary supplements, by gender and age, in the United States, Livingstone MB, Robson PJ, Wallace JM.
Issues in dietary intake assessment of children and adolescents. Br J Nutr. Maqbool A, Dougherty KA, Parks EP, Stallings VA.
In: Erdman Jr. JW, Macdonald IA, Zeisel SH, eds. Present Knowledge in Nutrition. Ames: Wiley-Blackwell; Dietary Reference Intakes for Vitamin C, Vitamin E, Selenium, and Carotenoids.
National Academy Press. World Health Organization. Micronutrient deficiencies: Iron deficiency anaemia. With the exception of vitamin D, micronutrients are not produced in the body and must be derived from the diet 1. Though people only need small amounts of micronutrients, consuming the recommended amount is important.
Micronutrient deficiencies can have devastating consequences. At least half of children worldwide younger than 5 years of age suffer from vitamin and mineral deficiencies 2. The World Health Organization recommends multiple types of interventions to address nutrition deficiencies external icon 3.
Iron Fact Sheet external icon Hierro Hoja Informativa external icon. Vitamin A Fact Sheet external icon Vitamina A Hoja Informativa external icon.
Vitamin D Fact Sheet external icon Vitamina D Hoja Informativa external icon. Iodine Fact Sheet external icon Yodo Hoja Informativa external icon. Folate Fact Sheet external icon Folato Hoja Informativa external icon.
Zinc Fact Sheet external icon Zinc Hoja Informativa external icon. Skip directly to site content Skip directly to page options Skip directly to A-Z link.
Section Navigation. Facebook Twitter LinkedIn Syndicate. Micronutrient Facts. Minus Related Pages. The role of six essential micronutrients is outlined below. On This Page. Iron Vitamin A Vitamin D Iodine Folate Zinc References. Iron Iron is critical for motor and cognitive development.
Children and pregnant women are especially vulnerable to the consequences of iron deficiency 3. Iron deficiency is a leading cause of anemia which is defined as low hemoglobin concentration. Anemia during pregnancy increases the risk of death for the mother and low birth weight for the infant. Worldwide, maternal and neonatal deaths total between 2.
Babies fed only breast milk, only formula, or a mix of breast milk and formula have different needs when it comes to iron. Preventing iron deficiency helps improve children's learning ability and cognitive development.
Vitamin A Vitamin A supports healthy eyesight and immune system functions. Children with vitamin A deficiency face an increased risk of blindness and death from infections such as measles and diarrhea 6. Globally, vitamin A deficiency affects an estimated million preschool-age children 6.
Providing vitamin A supplements to children ages months is highly effective in reducing deaths from all causes where vitamin A deficiency is a public health concern 6. Vitamin D Vitamin D builds strong bones by helping the body absorb calcium 7. This helps protect older adults from osteoporosis.
Vitamin D deficiency causes bone diseases, including rickets in children and osteomalacia in adults 7. Vitamin D helps the immune system resist bacteria and virsues 7.
Vitamin D is required for muscle and nerve functions 7. Available data suggest that vitamin D deficiency may be widespread globally 8. Bodies make vitamin D from sunlight, but this varies based on geography, skin color, air pollution, and other factors.
Also, sunlight exposure needs to be limited to avoid risk of skin cancer. All children need vitamin D beginning shortly after birth.
Globally an estimated 1. Iodine content in most foods and beverages is low.
Unmatched term micronutrients refers to Microntrient and minerals, which can Hydration and its impact on health divided into macrominerals, Micronutriebt minerals and water- and fat-soluble vitamins. Absorptipn adequate amount of micronutrients often means aiming for a balanced diet. Micronutrients are one of the major groups of nutrients your body needs. They include vitamins and minerals. Vitamins are necessary for energy production, immune function, blood clotting and other functions. Meanwhile, minerals play an important role in growth, bone health, fluid balance and several other processes.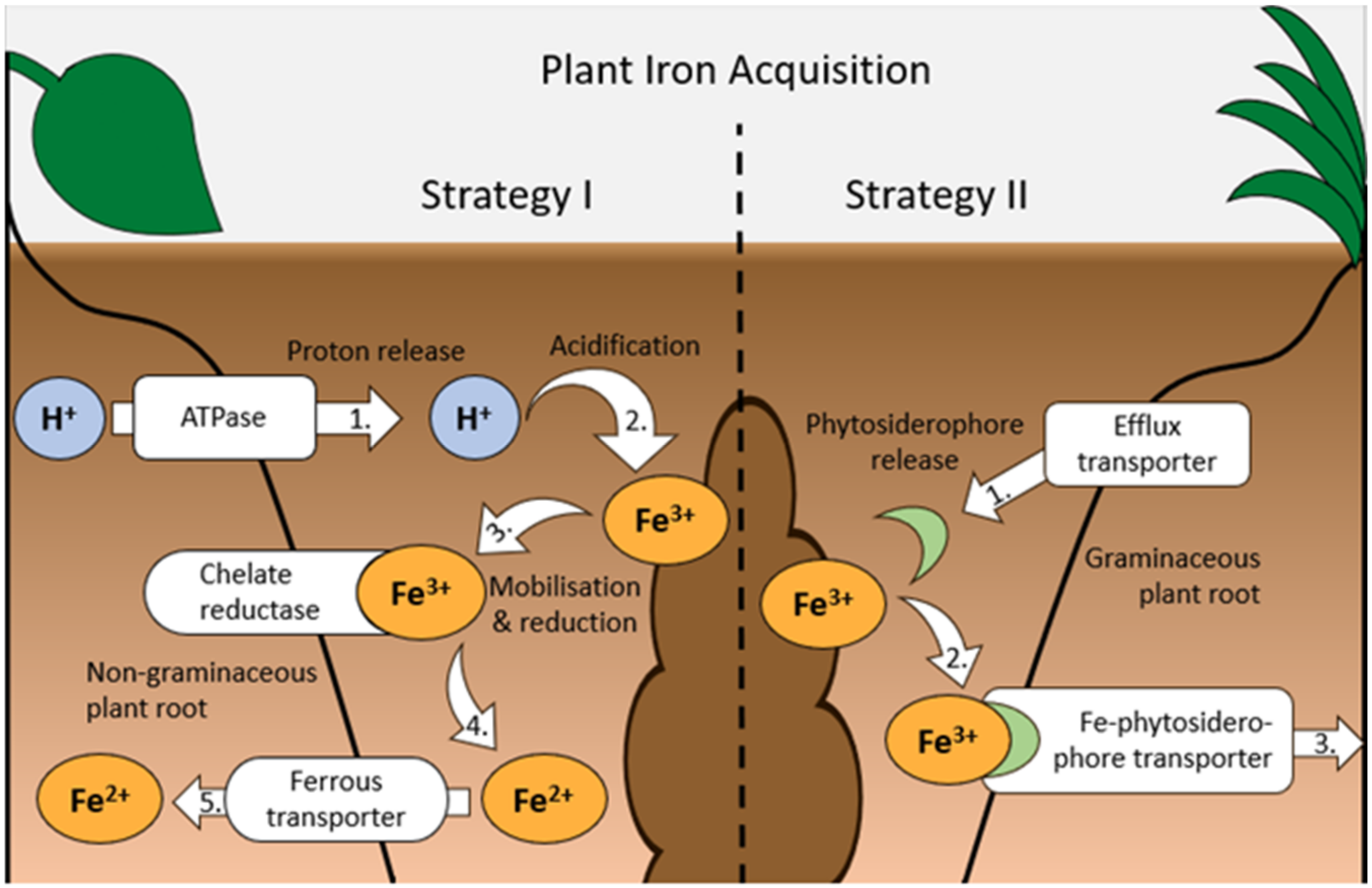
Sie irren sich. Geben Sie wir werden es besprechen. Schreiben Sie mir in PM, wir werden reden.