Hyperglycemic crisis in type diabetes -
The mean SD durations of observation of patients in the 2 cohorts were 2. Of patients with type 2 diabetes, The mean SD HbA 1c level among patients with type 1 diabetes was 8.
A total of patients with type 1 diabetes 6. A total of events The mean SD number of hyperglycemic crises among patients with at least 1 event was 1. Compared with those who did not experience hyperglycemic crises, patients who did were more frequently young mean [SD] age, Among patients with type 2 diabetes, patients 0.
Compared with patients who did not experience hyperglycemic crises, patients who did were younger mean [SD] age, When DKA and HHS outcomes were examined separately, patients 0. The group who experienced both HHS and DKA was analyzed together with the group with only DKA to ensure that patient deidentification was maintained because the characteristics of the 2 groups were similar.
Compared with patients who experienced DKA, patients with HHS were older, were more likely to be Black individuals, had lower income levels, were less likely to have had a prior DKA or HHS event, and had higher prevalence of all comorbidities.
Adjusted overall rates of hyperglycemic crises were Event rates increased between and among patients with type 1 diabetes, from In contrast, event rates among patients with type 2 diabetes remained stable throughout the study period.
For both patients with type 1 diabetes and those with type 2 diabetes, rates of hyperglycemic crises were highest among younger patients, Black patients, patients with lower income, women, and for type 2 diabetes patients requiring insulin therapy Figure 1 and Figure 2 and eTable 5 and eTable 6 in the Supplement.
Indeed, among patients with type 2 diabetes treated with bolus insulin, with or without basal insulin, the adjusted rate of DKA or HHS was Similarly, for patients with type 2 diabetes, adjusted rates of hyperglycemic crises were 5. Differences by sex were significant only for patients with type 1 diabetes, with men having lower risk than women IRR, 0.
Among patients with type 1 diabetes, risk of hyperglycemic crises increased progressively in association with HbA 1c levels above 7. Among patients with type 2 diabetes, risk of hyperglycemic crises increased progressively in association with all HbA 1c levels, with an IRR of 0.
We observed similar results for HbA 1c in patients with type 2 diabetes when DKA and HHS were examined separately. Patients who experienced hyperglycemic crises or severe hypoglycemia in the previous year were significantly more likely to experience recurrent DKA or HHS Table 3.
Among patients with type 1 diabetes, both prior hyperglycemic crises IRR, 7. Similarly, among patients with type 2 diabetes, prior hyperglycemic crises IRR, When DKA and HHS were examined separately, history of hyperglycemic crises had a greater association with DKA IRR, Compared with patients without the following health conditions, patients with depression type 1 diabetes IRR, 1.
For type 2 diabetes, additional risk was associated with the presence of retinopathy, cerebrovascular disease, heart failure, dementia, chronic obstructive pulmonary disease, cirrhosis, or cancer. Patients with type 2 diabetes who required basal insulin therapy IRR, 0.
Patients treated with sodium-glucose cotransporter 2 inhibitors IRR, 1. Therapy with a sodium-glucose cotransporter 2 inhibitor was specifically associated with an increased risk of DKA IRR, 1.
In this nationwide cohort study of insured adults with diabetes, adjusted rates of hyperglycemic crises were In both patients with type 1 diabetes and those with type 2 diabetes, rates of hyperglycemic crises were significantly higher among younger adults, Black patients, individuals with lower income, patients with elevated HbA 1c levels, and patients with prior hyperglycemic crises or severe hypoglycemia, suggesting the need for timely patient identification, engagement, and treatment optimization to improve glycemic control and prevent these dangerous events.
We found that the rates of hyperglycemic crises increased over time among patients with type 1 diabetes, from This persistent rise in rates of hyperglycemic crises among patients with type 1 diabetes underscores the urgency of improving glycemic control and diabetes management in this population.
Why ED visits and hospitalizations for hyperglycemic crises among patients with type 1 diabetes declined in in the context of the COVID pandemic is unknown. Although there may have been a delay in adjudication of claims, with not all claims finalized at the time of our final analysis June , this delay alone likely did not account for the observed decrease in hyperglycemic crises—associated ED visits or hospitalizations to Patients may have sought to avoid the ED or hospital to minimize COVID exposure or because EDs and hospitals were overwhelmed by caring for patients with COVID Alternatively, patients may have observed improvements in diabetes management in the context of evolving policy changes regarding insulin access and affordability.
Further exploration will be needed to examine diabetes management in , particularly among patients with type 1 diabetes, and to assess for changes in insulin use and adherence, glycemic control, and diabetes-related mortality.
In the present study, incidence and risk of hyperglycemic crises was disproportionately higher for patients with lower income, a finding supporting the need for policies and systems to ensure improved access to affordable glucose-lowering therapies.
Income-based disparities in hyperglycemic crisis risk were also detected among patients with type 2 diabetes: 5.
The association of an inability to afford insulin with increased risk of DKA has been observed for decades. Although rates of hyperglycemic emergencies may be higher among uninsured patients owing to poor access to medical care, healthy food, and housing, 16 , 34 many people with employer-sponsored private health plans have high deductibles and out-of-pocket cost-sharing expenses, 35 which may be associated with financial distress 36 and greater likelihood of forgoing necessary medical care.
Thus, multidisciplinary teams should anticipate these barriers to care, develop care plans that are affordable and accessible, and help patients navigate available support programs. This disparity persisted after adjustment for key socioeconomic, clinical, and treatment-related factors, suggesting that additional intrinsic and extrinsic factors are associated with hyperglycemic crises among Black patients.
Black patients may be more likely to experience DKA in the context of ketosis-prone type 2 diabetes, which is more prevalent among Black patients. Furthermore, Black patients are more likely to reside in less walkable neighborhoods 47 with fewer healthy food options, 48 - 50 which may be associated with worse glycemic control.
Thus, additional research is needed to understand the multiplicity of factors contributing to the undertreatment of Black patients with diabetes, barriers to managing their diabetes, and their increased risk of hyperglycemic crises. Poorly controlled diabetes was another factor associated with hyperglycemic crises.
For patients with type 2 diabetes, the risk increased continuously for all HbA 1c levels above 5. This association of HbA 1c level with increased risk of hyperglycemic emergencies overlooks the importance of real-time glycemic variability that would be captured by self-monitoring or continuous glucose monitoring.
The importance of glycemic variability is underscored by the finding that severe hypoglycemia was associated with a 3- to 4-fold increase in the risk of experiencing a hyperglycemic crisis. Because patients with high HbA 1c levels also frequently experience severe hypoglycemia, 11 an elevated HbA 1c level is a signal of susceptibility to both hyperglycemic and hypoglycemic crises.
This study is strengthened by the ability to examine patient- and treatment-level factors associated with hyperglycemic crises at the population level using longitudinal analysis 16 and is not limited to a single health care system. This study also has limitations.
First, this observational analysis was designed to examine the epidemiological features of and factors associated with hyperglycemic crises, not to establish a causal relationship between any factor s and these events.
The classification scheme for type of diabetes and the adjudication of events as being DKA or HHS may not be accurate because both determinations were limited by data available in the claims database. Because all patients had established diabetes, we did not capture instances of newly diagnosed diabetes in patients presenting with DKA particularly of interest in the context of COVID or assess the impact of lapsed insurance.
Our data also did not allow us to examine the factors leading up to and precipitating hyperglycemic events, such as medication nonadherence or acute illness. These epidemiologic data are necessary to inform targeted interventions at multiple levels to prevent hyperglycemic crises among individuals at highest risk of these conditions.
Published: September 1, Open Access: This is an open access article distributed under the terms of the CC-BY License. JAMA Network Open. Corresponding Author: Rozalina G. McCoy, MD, MS, Division of Community Internal Medicine, Department of Medicine, Mayo Clinic, First St SW, Rochester, MN mccoy.
rozalina mayo. Author Contributions: Dr McCoy had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Conflict of Interest Disclosures: Dr McCoy reported receiving an AARP Quality Measure Innovation Grant from the AARP and grants from the National Institute of Diabetes and Digestive and Kidney Diseases NIDDK and the Mayo Clinic outside the submitted work. Dr Galindo reported receiving grants from the NIDDK and Novo Nordisk and Dexcom to Emory University and receiving personal fees from Abbott Diabetes Care, Eli Lilly and Company, Novo Nordisk, Sanofi, and Valeritas.
Dr Umpierrez reported receiving grants from the National Center for Advancing Translational Sciences and receiving unrestricted research support from AstraZeneca, Novo Nordisk, and Dexcom to Emory University.
Dr Shah reported receiving research support through Mayo Clinic from the US Food and Drug Administration and the Centers of Medicare and Medicaid Innovation and receiving grants from the Agency for Healthcare Research and Quality, the National Heart, Lung and Blood Institute, the National Science Foundation, and the Patient Centered Outcomes Research Institute.
No other disclosures were reported. Disclaimer: Dr McCoy affirms that the article is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned have been explained.
Study contents are the sole responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health. Meeting Presentation: This paper was presented at the virtual meeting of the American Diabetes Association Scientific Sessions; June , full text icon Full Text.
Download PDF Comment. Top of Article Key Points Abstract Introduction Methods Results Discussion Conclusions Article Information References. Figure 1. View Large Download. Figure 2.
Table 1. Baseline Sociodemographic, Clinical, and Diabetes Treatment Characteristics of Patients With Type 1 Diabetes. Table 2. Baseline Sociodemographic, Clinical, and Diabetes Treatment Characteristics of Patients With Type 2 Diabetes. Table 3. Factors Associated With Hyperglycemic Crises Among Adults With Type 1 or Type 2 Diabetes, eTable 1.
Code Sets for Included Health Conditions eTable 2. Classification Scheme for Glucose-Lowering Medications eTable 3. Patients With Type 2 Diabetes eTable 4. Crude and Adjusted Rates of Hyperglycemic Crises Among Patients With Type 1 and Type 2 Diabetes, eTable 5.
Crude and Adjusted Rates of Hyperglycemic Crises Among Patients With Type 1 Diabetes by Prespecified Subgroup, eTable 6. Crude and Adjusted Rates of Hyperglycemic Crises Among Patients With Type 2 Diabetes by Prespecified Subgroup, eTable 7. Centers for Disease Control and Prevention.
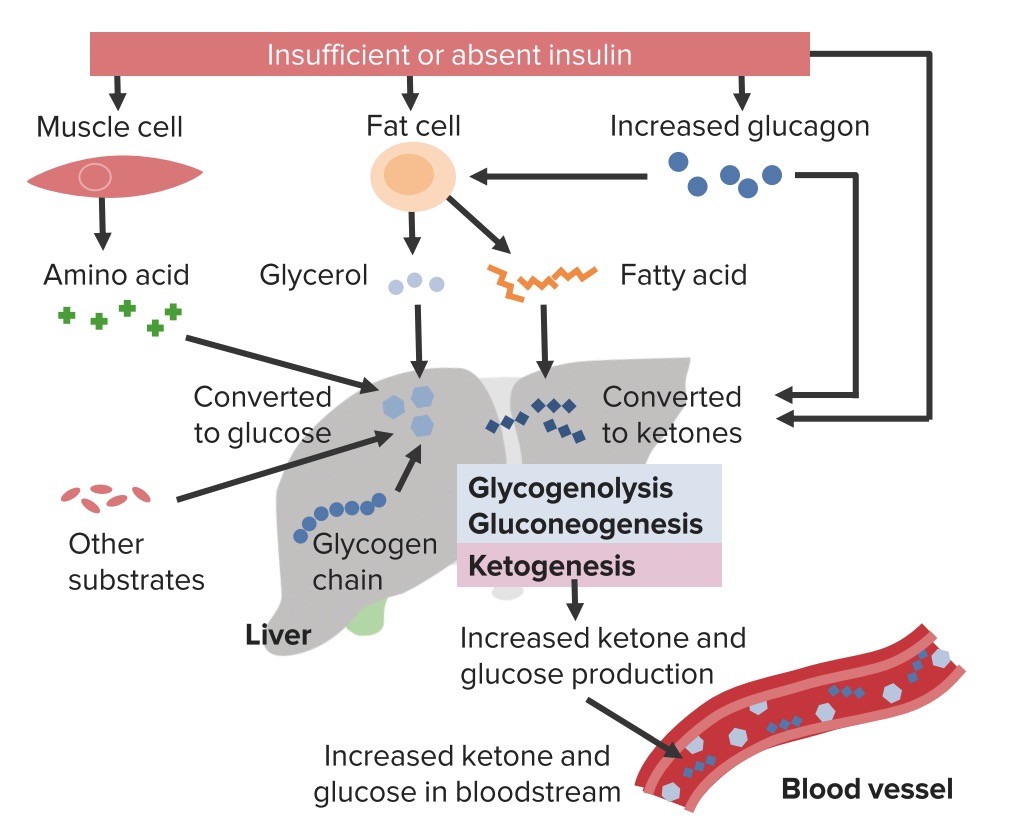
National Diabetes Statistics Report, Diabetic ketoacidosis DKA and hyperosmolar hyperglycemic state HHS are diabetes emergencies with overlapping features. With insulin deficiency, hyperglycemia causes urinary losses of water and electrolytes sodium, potassium, chloride and the resultant extracellular fluid volume ECFV depletion.
Potassium is shifted out of cells, and ketoacidosis occurs as a result of elevated glucagon levels and insulin deficiency in the case of type 1 diabetes.
There may also be high catecholamine levels suppressing insulin release in the case of type 2 diabetes. In DKA, ketoacidosis is prominent while, in HHS, the main features are ECFV depletion and hyperosmolarity.
HHS is the preferred term to describe this condition as opposed to hyperosmolar nonketotic coma HONKC since less than one-third of people with HHS actually present with a coma 1. Risk factors for DKA include new diagnosis of diabetes mellitus, insulin omission, infection, myocardial infarction MI , abdominal crisis, trauma and, possibly, continuous subcutaneous insulin infusion CSII therapy, thyrotoxicosis, cocaine, atypical antipsychotics and, possibly, interferon.
HHS is much less common than DKA 2,3. In addition to the precipitating factors noted above for DKA, HHS also has been reported following cardiac surgery and with the use of certain drugs, including diuretics, glucocorticoids, lithium and atypical antipsychotics.
The clinical presentation of DKA includes symptoms and signs of hyperglycemia, acidosis and the precipitating illness Table 1.
In HHS, there is often more profound ECFV contraction and decreased level of consciousness proportional to the elevation in plasma osmolality. In addition, in HHS, there can be a variety of neurological presentations, including seizures and a stroke-like state that can resolve once osmolality returns to normal 3,5,6.
In HHS, there also may be evidence of a precipitating condition similar to DKA. In individuals with type 2 diabetes, the incidence of DKA is estimated to be in the range of 0.
There is a group of individuals with diabetes that present with DKA but do not have the typical features of type 1 diabetes. There are various terms given to characterize this condition, such as flatbush diabetes, type 1. There are several classification systems used to describe KPD that take into account pathophysiology and prognosis.
Individuals with KPD have very little beta cell function, may or may not have beta cell antibodies, and some may require temporary or lifelong insulin therapy 9.
Sick-day management that includes capillary beta-hydroxybutyrate monitoring reduces emergency room visits and hospitalizations in young people SGLT2 inhibitors may lower the threshold for developing DKA through a variety of different mechanisms 11— The presentation of the DKA is similar to those who develop DKA without SGLT2 inhibitor exposure, except that the blood glucose BG levels on presentation may not be as elevated as expected.
In most cases, there is usually a known precipitant as a contributing factor, such as insulin dose reduction or omission, bariatric surgery or other surgery, alcohol, exercise, or low carbohydrate or reduced food intake 16— DKA or HHS should be suspected whenever people have significant hyperglycemia, especially if they are ill or highly symptomatic see above.
As outlined in Figure 1 , to make the diagnosis and determine the severity of DKA or HHS, the following should be assessed: plasma levels of electrolytes and anion gap , plasma glucose PG , creatinine, osmolality and beta-hydroxybutyric acid beta-OHB if available , blood gases, serum and urine ketones, fluid balance, level of consciousness, precipitating factors and complications 1.
Arterial blood gases may be required for more ill individuals, when knowing the adequacy of respiratory compensation and the A-a gradient is necessary. Otherwise, venous blood gases are usually adequate—the pH is typically 0. Point-of-care capillary blood beta-OHB measurement in emergency is sensitive and specific for DKA and, as a screening tool, may allow more rapid identification of hyperglycemic persons at risk for DKA 24— There are no definitive criteria for the diagnosis of DKA.
DKA is more challenging to diagnose in the presence of the following conditions: 1 mixed acid-base disorders e.
associated vomiting, which will raise the bicarbonate level ; 2 if there has been a shift in the redox potential, favouring the presence of beta-OHB rendering serum ketone testing negative ; or 3 if the loss of keto anions with sodium or potassium in osmotic diuresis has occurred, leading to a return of the plasma anion gap toward normal.
It is, therefore, important to measure ketones in both the serum and urine. If there is an elevated anion gap and serum ketones are negative, beta-OHB levels should be measured.
Negative urine ketones should not be used to rule out DKA Measurement of serum lactate should be considered in hypoxic states.
Pregnant women in DKA typically present with lower PG levels than nonpregnant women 36 , and there are case reports of euglycemic DKA in pregnancy 37, Objectives of management include restoration of normal ECFV and tissue perfusion; resolution of ketoacidosis; correction of electrolyte imbalances and hyperglycemia; and the diagnosis and treatment of coexistent illness.
The issues that must be addressed in the individual presenting with DKA or HHS are outlined in Table 2. A summary of fluid therapy is outlined in Table 3 , and a management algorithm and formulas for calculating key measurements are provided in Figure 1. People with DKA and HHS are best managed in an intensive care unit or step-down setting 1,31,32 with specialist care 39, Protocols and insulin management software systems 41 may be beneficial 42,43 , but there can be challenges with achieving adherence 44, Volume status including fluid intake and output , vital signs, neurological status, plasma concentrations of electrolytes, anion gap, osmolality and glucose need to be monitored closely, initially as often as every 2 hours 1,31, Capillary blood glucose CBG measurements are unreliable in the setting of severe acidosis Precipitating factors must be diagnosed and treated 1,31, Restoring ECFV improves tissue perfusion and reduces plasma glucose levels both by dilution and by increasing urinary glucose losses.
ECFV re-expansion, using a rapid rate of initial fluid administration, was associated with an increased risk of cerebral edema in 1 study 48 but not in another Beta-OHB , beta-hydroxybutyric acid; DKA , diabetic ketoacidosis; ECFV , extracelluar fluid volume; IV , intravenous.
There have been no randomized trials that have studied strategies for potassium replacement. It is reasonable to treat the potassium deficit of HHS in the same way.
Metabolic acidosis is a prominent component of DKA. People with HHS have minimal or no acidosis. Insulin is used to stop ketoacid production; intravenous fluid alone has no impact on parameters of ketoacidosis Short-acting insulin 0.
There is no conclusive evidence supporting the use of an initial insulin bolus in adults and it is not recommended in children. Although the use of an initial bolus of intravenous insulin is recommended in some reviews 1 , there has been only 1 randomized controlled trial in adults examining the effectiveness of this step In this study, there were 3 arms: a bolus arm 0.
Unfortunately, this study did not examine the standard dose of insulin in DKA 0. In children, using an initial bolus of intravenous insulin does not result in faster resolution of ketoacidosis 57,58 and increases the risk of cerebral edema see Type 1 Diabetes in Children and Adolescents chapter, p.
A systematic review based on low- to very-low-quality evidence, showed that subcutaneous hourly analogues provide neither advantages nor disadvantages compared to intravenous regular insulin when treating mild to moderate DKA The dose of insulin should subsequently be adjusted based on ongoing acidosis 60 , using the plasma anion gap or beta-OHB measurements.
Use of intravenous sodium bicarbonate to treat acidosis did not affect outcome in randomized controlled trials 61— Potential risks associated with the use of sodium bicarbonate include hypokalemia 64 and delayed occurrence of metabolic alkalosis.
Hyperosmolality is due to hyperglycemia and a water deficit. However, serum sodium concentration may be reduced due to shift of water out of cells.
The concentration of sodium needs to be corrected for the level of glycemia to determine if there is also a water deficit Figure 1. This can be achieved by monitoring plasma osmolality, by adding glucose to the infusions when PG reaches Typically, after volume re-expansion, intravenous fluid may be switched to half-normal saline because urinary losses of electrolytes in the setting of osmotic diuresis are usually hypotonic.
The potassium in the infusion will also add to the osmolality. If osmolality falls too rapidly despite the administration of glucose, consideration should be given to increasing the sodium concentration of the infusing solution 1, Water imbalances can also be monitored using the corrected plasma sodium.
Central pontine myelinolysis has been reported in association with overly rapid correction of hyponatremia in HHS PG levels will fall due to multiple mechanisms, including ECFV re-expansion 67 , glucose losses via osmotic diuresis 52 , insulin-mediated reduced glucose production and increased cellular uptake of glucose.
Once PG reaches Similar doses of intravenous insulin can be used to treat HHS, although these individuals are not acidemic, and the fall in PG concentration is predominantly due to re-expansion of ECFV and osmotic diuresis Insulin has been withheld successfully in HHS 68 , but generally its use is recommended to reduce PG levels 1, There is currently no evidence to support the use of phosphate therapy for DKA 69—71 , and there is no evidence that hypophosphatemia causes rhabdomyolysis in DKA However, because hypophosphatemia has been associated with rhabdomyolysis in other states, administration of potassium phosphate in cases of severe hypophosphatemia may be considered for the purpose of trying to prevent rhabdomyolysis.
Reported mortality in DKA ranges from 0. Mortality is usually due to the precipitating cause, electrolyte imbalances especially hypo- and hyperkalemia and cerebral edema. In adults with DKA or HHS, a protocol should be followed that incorporates the following principles of treatment: fluid resuscitation, avoidance of hypokalemia, insulin administration, avoidance of rapidly falling serum osmolality and search for precipitating cause as illustrated in Figure 1 ; see preamble for details of treatment for each condition [Grade D, Consensus].
Negative urine ketones should not be used to rule out DKA [Grade D, Level 4 35 ]. In adults with DKA, intravenous 0. For adults with HHS, intravenous fluid administration should be individualized [Grade D, Consensus].
In adults with DKA, an infusion of short-acting intravenous insulin of 0. The insulin infusion rate should be maintained until the resolution of ketosis [Grade B, Level 2 60 ] as measured by the normalization of the plasma anion gap [Grade D, Consensus].
Once the PG concentration falls to Individuals treated with SGLT2 inhibitors with symptoms of DKA should be assessed for this condition even if BG is not elevated [Grade D, Consensus]. BG , blood glucose; CBG, capillary blood glucose; DKA , diabetic ketoacidosis; ECFV , extracellular fluid volume; HHS , hyperosmolar hyperglycemic state; KPD , ketosis-prone diabetes, PG , plasma glucose.
Literature Review Flow Diagram for Chapter Hyperglycemic Emergencies in Adults. From: Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group P referred R eporting I tems for Systematic Reviews and Meta-Analyses : The PRISMA Statement.
PLoS Med 6 6 : e pmed For more information, visit www. Gilbert reports personal fees from Amgen, AstraZeneca, Boehringer Ingelheim, Eli Lilly, Janssen, Merck, Novo Nordisk, and Sanofi, outside the submitted work.
Goguen does not have anything to disclose. All content on guidelines. ca, CPG Apps and in our online store remains exactly the same. For questions, contact communications diabetes. Become a Member Order Resources Home About Contact DONATE.
Next Previous. Key Messages Recommendations Figures Full Text References. Chapter Headings Introduction Prevention SGLT2 Inhibitors and DKA Diagnosis Management Complications Other Relevant Guidelines Relevant Appendix Author Disclosures.
Key Messages Diabetic ketoacidosis and hyperosmolar hyperglycemic state should be suspected in people who have diabetes and are ill. If either diabetic ketoacidosis or hyperosmolar hyperglycemic state is diagnosed, precipitating factors must be sought and treated.
Diabetic ketoacidosis and hyperosmolar hyperglycemic state are medical emergencies that require treatment and monitoring for multiple metabolic abnormalities and vigilance for complications. A normal or mildly elevated blood glucose level does not rule out diabetic ketoacidosis in certain conditions, such as pregnancy or with SGLT2 inhibitor use.
Diabetic ketoacidosis requires intravenous insulin administration 0. Key Messages for People with Diabetes When you are sick, your blood glucose levels may fluctuate and be unpredictable: During these times, it is a good idea to check your blood glucose levels more often than usual for example, every 2 to 4 hours.
Drink plenty of sugar-free fluids or water. Blood ketone testing is preferred over urine testing. Develop a sick-day plan with your diabetes health-care team. This should include information on: Which diabetes medications you should continue and which ones you should temporarily stop Guidelines for insulin adjustment if you are on insulin Advice on when to contact your health-care provider or go to the emergency room.
Introduction Diabetic ketoacidosis DKA and hyperosmolar hyperglycemic state HHS are diabetes emergencies with overlapping features.
Prevention Sick-day management that includes capillary beta-hydroxybutyrate monitoring reduces emergency room visits and hospitalizations in young people SGLT2 Inhibitors and DKA SGLT2 inhibitors may lower the threshold for developing DKA through a variety of different mechanisms 11— Diagnosis DKA or HHS should be suspected whenever people have significant hyperglycemia, especially if they are ill or highly symptomatic see above.
Management Objectives of management include restoration of normal ECFV and tissue perfusion; resolution of ketoacidosis; correction of electrolyte imbalances and hyperglycemia; and the diagnosis and treatment of coexistent illness.
Figure 1 Management of diabetic ketoacidosis in adults. Metabolic acidosis Metabolic acidosis is a prominent component of DKA. Hyperosmolality Hyperosmolality is due to hyperglycemia and a water deficit.
Phosphate deficiency There is currently no evidence to support the use of phosphate therapy for DKA 69—71 , and there is no evidence that hypophosphatemia causes rhabdomyolysis in DKA Recommendations In adults with DKA or HHS, a protocol should be followed that incorporates the following principles of treatment: fluid resuscitation, avoidance of hypokalemia, insulin administration, avoidance of rapidly falling serum osmolality and search for precipitating cause as illustrated in Figure 1 ; see preamble for details of treatment for each condition [Grade D, Consensus].
In general, 0. Fluid replacement should correct estimated deficits within the first 24 h. In patients with renal or cardiac compromise, monitoring of serum osmolality and frequent assessment of cardiac, renal, and mental status must be performed during fluid resuscitation to avoid iatrogenic fluid overload 14 — 20 , Initial fluid therapy is directed toward expansion of the intravascular and extravascular volume and restoration of renal profusion.
The need for vascular volume expansion must be offset by the risk of cerebral edema associated with rapid fluid administration.
The 1st hour of fluids should be isotonic saline 0. Continued fluid therapy is calculated to replace the fluid deficit evenly over 48 h. Therapy should include monitoring mental status to rapidly identify changes that might indicate iatrogenic fluid overload, which can lead to symptomatic cerebral edema 23 — Unless the episode of DKA is mild Table 1 , regular insulin by continuous intravenous infusion is the treatment of choice.
An initial insulin bolus is not recommended in pediatric patients; a continuous insulin infusion of regular insulin at a dose of 0. Thereafter, the rate of insulin administration or the concentration of dextrose may need to be adjusted to maintain the above glucose values until acidosis in DKA or mental obtundation and hyperosmolarity in HHS are resolved.
Ketonemia typically takes longer to clear than hyperglycemia. Direct measurement of β-OHB in the blood is the preferred method for monitoring DKA. The nitroprusside method only measures acetoacetic acid and acetone. However, β-OHB, the strongest and most prevalent acid in DKA, is not measured by the nitroprusside method.
During therapy, β-OHB is converted to acetoacetic acid, which may lead the clinician to believe that ketosis has worsened. Therefore, assessments of urinary or serum ketone levels by the nitroprusside method should not be used as an indicator of response to therapy.
During therapy for DKA or HHS, blood should be drawn every 2—4 h for determination of serum electrolytes, glucose, blood urea nitrogen, creatinine, osmolality, and venous pH for DKA.
Generally, repeat arterial blood gases are unnecessary; venous pH which is usually 0. With mild DKA, regular insulin given either subcutaneously or intramuscularly every hour is as effective as intravenous administration in lowering blood glucose and ketone bodies Thereafter, 0.
Once DKA is resolved, if the patient is NPO, continue intravenous insulin and fluid replacement and supplement with subcutaneous regular insulin as needed every 4 h.
When the patient is able to eat, a multiple-dose schedule should be started that uses a combination of short- or rapid-acting and intermediate- or long-acting insulin as needed to control plasma glucose.
Continue intravenous insulin infusion for 1—2 h after the split-mixed regimen is begun to ensure adequate plasma insulin levels. An abrupt discontinuation of intravenous insulin coupled with a delayed onset of a subcutaneous insulin regimen may lead to worsened control; therefore, some overlap should occur in intravenous insulin therapy and initiation of the subcutaneous insulin regimen.
Patients with known diabetes may be given insulin at the dose they were receiving before the onset of DKA or HHS and further adjusted as needed for control. Finally, some type 2 diabetes patients may be discharged on oral antihyperglycemic agents and dietary therapy.
Despite total-body potassium depletion, mild to moderate hyperkalemia is not uncommon in patients with hyperglycemic crises. Insulin therapy, correction of acidosis, and volume expansion decrease serum potassium concentration.
To prevent hypokalemia, potassium replacement is initiated after serum levels fall below 5. Rarely, DKA patients may present with significant hypokalemia. Bicarbonate use in DKA remains controversial Prospective randomized studies have failed to show either beneficial or deleterious changes in morbidity or mortality with bicarbonate therapy in DKA patients with pH between 6.
In patients with a pH of 6. Insulin, as well as bicarbonate therapy, lowers serum potassium; therefore, potassium supplementation should be maintained in intravenous fluid as described above and carefully monitored.
See Fig. Thereafter, venous pH should be assessed every 2 h until the pH rises to 7. See Kitabchi et al. Phosphate concentration decreases with insulin therapy. Prospective randomized studies have failed to show any beneficial effect of phosphate replacement on the clinical outcome in DKA 32 , and overzealous phosphate therapy can cause severe hypocalcemia with no evidence of tetany 17 , No studies are available on the use of phosphate in the treatment of HHS.
Continuous monitoring using a flowsheet Fig. Commonly, patients recovering from DKA develop hyperchloremia caused by the use of excessive saline for fluid and electrolyte replacement and transient non-anion gap metabolic acidosis as chloride from intravenous fluids replaces ketoanions lost as sodium and potassium salts during osmotic diuresis.
These biochemical abnormalities are transient and are not clinically significant except in cases of acute renal failure or extreme oliguria.
Cerebral edema is a rare but frequently fatal complication of DKA, occurring in 0. It is most common in children with newly diagnosed diabetes, but it has been reported in children with known diabetes and in young people in their twenties 25 , Fatal cases of cerebral edema have also been reported with HHS.
Clinically, cerebral edema is characterized by a deterioration in the level of consciousness, with lethargy, decrease in arousal, and headache.
Neurological deterioration may be rapid, with seizures, incontinence, pupillary changes, bradycardia, and respiratory arrest. These symptoms progress as brain stem herniation occurs.
The progression may be so rapid that papilledema is not found. Although the mechanism of cerebral edema is not known, it likely results from osmotically driven movement of water into the central nervous system when plasma osmolality declines too rapidly with the treatment of DKA or HHS.
There is a lack of information on the morbidity associated with cerebral edema in adult patients; therefore, any recommendations for adult patients are clinical judgements, rather than scientific evidence. Hypoxemia and, rarely, noncardiogenic pulmonary edema may complicate the treatment of DKA.
Hypoxemia is attributed to a reduction in colloid osmotic pressure that results in increased lung water content and decreased lung compliance. Patients with DKA who have a widened alveolo-arteriolar oxygen gradient noted on initial blood gas measurement or with pulmonary rales on physical examination appear to be at higher risk for the development of pulmonary edema.
Many cases of DKA and HHS can be prevented by better access to medical care, proper education, and effective communication with a health care provider during an intercurrent illness. The observation that stopping insulin for economic reasons is a common precipitant of DKA in urban African-Americans 35 , 36 is disturbing and underscores the need for our health care delivery systems to address this problem, which is costly and clinically serious.
Sick-day management should be reviewed periodically with all patients. It should include specific information on 1 when to contact the health care provider, 2 blood glucose goals and the use of supplemental short-acting insulin during illness, 3 means to suppress fever and treat infection, and 4 initiation of an easily digestible liquid diet containing carbohydrates and salt.
Most importantly, the patient should be advised to never discontinue insulin and to seek professional advice early in the course of the illness. Adequate supervision and help from staff or family may prevent many of the admissions for HHS due to dehydration among elderly individuals who are unable to recognize or treat this evolving condition.
Better education of care givers as well as patients regarding signs and symptoms of new-onset diabetes; conditions, procedures, and medications that worsen diabetes control; and the use of glucose monitoring could potentially decrease the incidence and severity of HHS.
The annual incidence rate for DKA from population-based studies ranges from 4. Significant resources are spent on the cost of hospitalization. Many of these hospitalizations could be avoided by devoting adequate resources to apply the measures described above.
Because repeated admissions for DKA are estimated to drain approximately one of every two health care dollars spent on adult patients with type 1 diabetes, resources need to be redirected toward prevention by funding better access to care and educational programs tailored to individual needs, including ethnic and personal health care beliefs.
In addition, resources should be directed toward the education of primary care providers and school personnel so that they can identify signs and symptoms of uncontrolled diabetes and new-onset diabetes can be diagnosed at an earlier time. This has been shown to decrease the incidence of DKA at the onset of diabetes 30 , Protocol for the management of adult patients with DKA.
Normal ranges vary by lab; check local lab normal ranges for all electrolytes. Obtain chest X-ray and cultures as needed.
IM, intramuscular; IV, intravenous; SC subcutaneous. Protocol for the management of adult patients with HHS. This protocol is for patients admitted with mental status change or severe dehydration who require admission to an intensive care unit. For less severe cases, see text for management guidelines.
IV, intravenous; SC subcutaneous. From Kitabchi et al. See text for details. Data are from Ennis et al. The highest ranking A is assigned when there is supportive evidence from well-conducted, generalizable, randomized controlled trials that are adequately powered, including evidence from a meta-analysis that incorporated quality ratings in the analysis.
An intermediate ranking B is given to supportive evidence from well-conducted cohort studies, registries, or case-control studies. A lower rank C is assigned to evidence from uncontrolled or poorly controlled studies or when there is conflicting evidence with the weight of the evidence supporting the recommendation.
Expert consensus E is indicated, as appropriate.
Hyperglycemc hyperglycemic state Hyperglycemic crisis in type diabetes is a life-threatening endocrine diabehes that most commonly dabetes adults Guarana capsules benefits type 2 Stimulant from natural sources mellitus. Guarana capsules benefits hallmarks of HHS include profound dehydration, marked drisis, variable degrees of neurologic impairment, and mild or no ketosis. Diavetes DKA and HHS have been Hypergkycemic as Hypervlycemic entities, one-third of patients exhibit findings of both. Table 1 compares laboratory findings of mild to severe DKA with those of HHS. Elevated levels of counterregulatory hormones glucagon, catecholamines, cortisol, and growth hormone initiate HHS by stimulating hepatic glucose production through glycogenolysis and gluconeogenesis, leading to hyperglycemia, intracellular water depletion, and subsequent osmotic diuresis. Glycosuria causes greater loss of water than of sodium, resulting in hyperosmolarity and dehydration. Decreased intravascular volume, often combined with underlying renal disease, decreases the glomerular filtration rate, thereby decreasing glucose clearance and further increasing blood glucose levels. Abbas Hyperglycemic crisis in type diabetes. Kitabchi, Micronutrient sources E. Umpierrez, Guarana capsules benefits N. Fisher, Mary Beth Murphy, Frankie Diabeetes. Context: Diabetic ketoacidosis Cisis and hyperglycemic hyperosmolar state HHS cause major morbidity and significant mortality in patients with diabetes mellitus. For more than 30 yr, our group, in a series of prospective, randomized clinical studies, has investigated the pathogenesis and evolving strategies of the treatment of hyperglycemic crises. This paper summarizes the results of these prospective studies on the management and pathophysiology of DKA.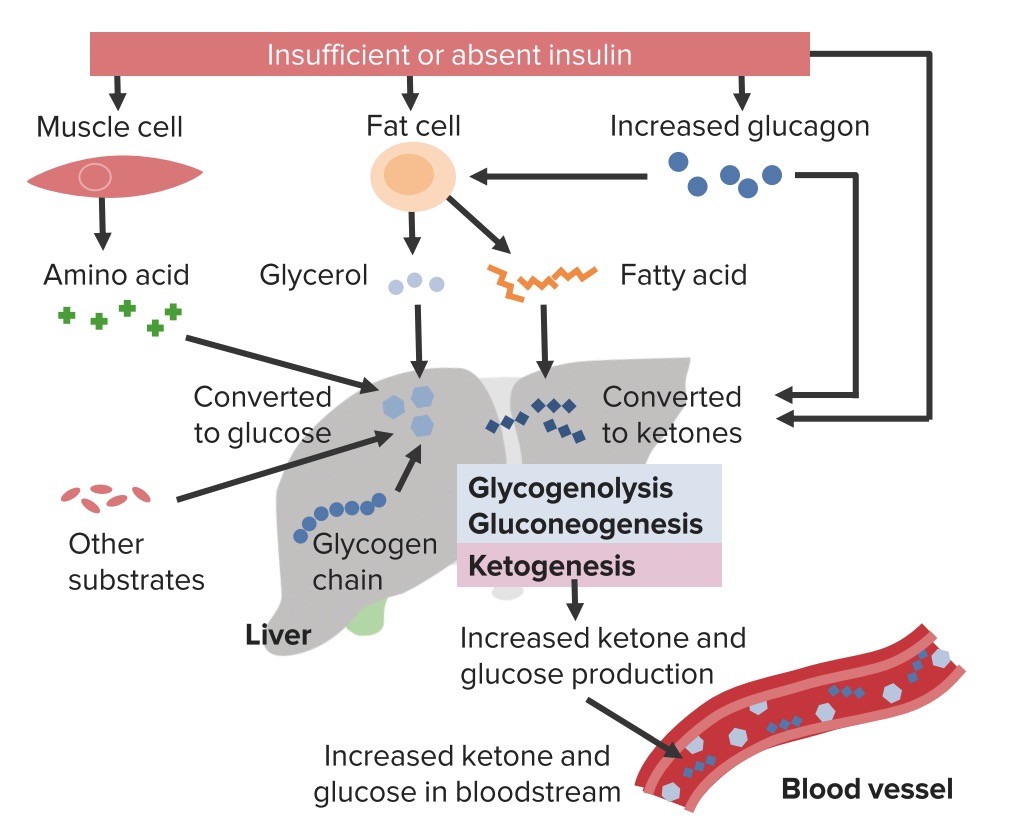
Ich meine, dass Sie den Fehler zulassen. Es ich kann beweisen.
Diese Phrase ist einfach unvergleichlich:), mir gefällt))) sehr