Video
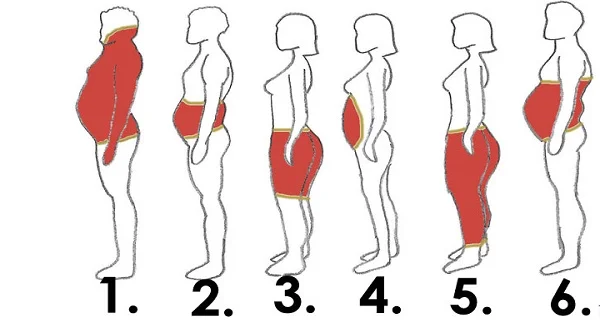
How the Microbiome Increases Visceral Fat Accumulation (Pot Belly)Android fat accumulation -
When both android fat amount and VAT were included in the multivariate regression model, the associations with coronary artery stenosis were not retained Table 4. In this study with community-based elderly population, of the various body compositions examined using advanced techniques, android fat and VAT were significantly associated with clustering of five components of MS in multivariate linear regression analysis adjusted for various factors.
When android fat and VAT were both included in the regression model, only android fat remained to be associated with clustering of MS components. The results suggest that android fat is strongly associated with MS in the elderly population even after adjusting for VAT.
Abdominal obesity is well recognized as a major risk factor of cardiovascular disease and type 2 diabetes [11]. Although anthropometric measurements such as BMI and waist circumference are widely used to estimate abdominal obesity, distinguishing between visceral and subcutaneous fat or between fat and lean mass cannot be ascertained.
Moreover, anthropometric measurements are subject to intra- and inter-examiner variations. Alternatively, more accurate methods used to measure regional fat depot are DXA and CT.
DXA and CT provide a comprehensive assessment of the component of body composition with each contributing its unique advantages. CT can distinguish between visceral and subcutaneous fat, and has been useful in measuring fat or muscle distribution at specific regions [23] , [24].
However, there are several limitations in the VAT quantification using CT scan. Even though VAT from a single scan obtained at the level of umbilicus was well correlated with the total visceral volume [25] , there could be a potential concern for over- or underestimation if we measure fat area at one selected level instead of measuring total fat volume.
In addition, CT scan has a greater risk of radiation hazards than DXA and is not appropriate for repetitive measurements [20] , [26]. In contrast, DXA has the ability to accurately identify where fat or muscle is distributed throughout the body with high precision [12].
The measurement of body composition is an area, which has attracted great interest because of the relationships between fat and lean tissue mass with health and disease. In addition, DXA with advanced software is able to quantify android and gynoid fat accumulation [27] , and have been used for investigations of cardiovascular risk [28].
Adipose tissue in the android region quantified by DXA has been found to have effects on plasma lipid and lipoprotein concentrations [29] and correlate strongly with abdominal visceral fat [30] , [31]. Thus, DXA is emerging as a new standard for body composition assessment due to its high precision, reliability and repeatability [32] , [33].
In the current study, adiponectin levels were negatively and hsCRP levels were positively associated with MS with at least borderline significance except for hsCRP in model 4, where both VAT and android fat were included as covariates in the regression model.
Mechanistically and theoretically, fat deposition in android area is suggested to have deleterious effects on the heart function, energy metabolism and development of atherosclerosis.
However, studies on android fat depot are limited [23]. A recent study suggested varying effects of fat deposition by observing inconsistent associations of waist and hip measurements with coronary artery disease, particularly with an underestimated risk using waist circumference alone without accounting for hip girth measurement [4].
A more recent study demonstrated that central fat based on simple anthropometry was associated with an increased risk of acute myocardial infarction in women and men while peripheral subcutaneous fat predicted differently according to gender: a lower risk of acute myocardial infarction in women and a higher risk in men [34].
Another study with obese youth confirmed harmful effects of android fat distribution on insulin resistance [35]. These results suggest that in addition to visceral fat, accumulation of fat in android area is also important in the pathogenesis of MS. Of note, in this study, android fat was more closely associated with a clustering of metabolic abnormalities than visceral fat.
There is no clear answer for this but several explanations can be postulated. First, android area defined in this study includes liver, pancreas and lower part of the heart. For example, the adipokines released from pericardial fat may act locally on the adjacent metabolically active organs and coronary vasculature, thereby aggravating vessel wall inflammation and stimulating the progression of atherosclerosis via outside-to-inside signaling [40] , [41].
Second, the android fat represents whole fat amount in the upper abdomen area while VAT measurement was performed at a single umbilicus level. This different methodology may possibly contribute to greater association between metabolic impairments and android fat than VAT.
This interpretation is supported by the borderline significance of VAT in the association with MS when combined VAT area was used instead of a single level of VAT.
A recent study also showed that the whole fat amount between L1—L5 vertebra showed a stronger relationship with insulin resistance than that of the single L3 level [39]. In this study, both android fat amount and VAT were associated with coronary artery stenosis.
Android fat is closely related with VAT because of their proximity and correlation with various cardiovascular risk factors. The attenuated associations of both variables without statistical significance in the regression model where android fat and VAT were simultaneously included may be due to a shared systemic effect as a result of shared risk factors for the development of atherosclerosis.
This study has several strengths. First, DXA with its advanced technology was used to measure regional fat depot. Second, the subjects were recruited from a well-defined population, which represented a single ethnic group and were older than 65 years.
Third, the regression analysis was adjusted for important factors including whole body fat mass, insulin resistance, and biochemical markers including adiponectin and hsCRP that might affect MS. This study also has several limitations.
First, since our study is limited by its cross-sectional nature, it is impossible to confirm clinically meaningful role of android fat depot. Therefore, further studies are needed to determine a predictive role of android fat for a clustering of cardiometabolic risk factors and subsequent incidence of cardiovascular diseases.
Second, this is a single cohort study with a small number of subjects and the results are confined to this specific cohort.
Of the various body compositions examined using advanced techniques, android fat measured by DXA was significantly associated with clustering of five components of MS even after accounting for various factors including visceral adiposity.
Participants characteristics including body composition measured by dual energy x-ray absorptiometry DXA and computed tomography CT subdivided by sex.
Correlation between summation of components of metabolic syndrome and multiple parameters including body composition. Multivariate linear regression analysis of associations of multiple parameters including body composition with summation of five individual components of metabolic syndrome VAT from L to L5-S1 was used.
Conceived and designed the experiments: SMK JWY HYA SYK KHL SL. Performed the experiments: SMK SL. Analyzed the data: HS SHC KSP HCJ. Wrote the paper: SMK SL. Browse Subject Areas?
Click through the PLOS taxonomy to find articles in your field. Article Authors Metrics Comments Media Coverage Reader Comments Figures.
Abstract Background Fat accumulation in android compartments may confer increased metabolic risk. Methods and Findings As part of the Korean Longitudinal Study on Health and Aging, which is a community-based cohort study of people aged more than 65 years, subjects male, Conclusions Our findings are consistent with the hypothesized role of android fat as a pathogenic fat depot in the MS.
Introduction Obesity is a heterogeneous disorder characterized by multi-factorial etiology. Methods Subjects, anthropometric and biochemical parameters This study was part of the Korean Longitudinal Study on Health and Aging KLoSHA , which is a cohort that began in and consisted of Korean subjects aged over 65 years men and women recruited from Seongnam city, one of the satellites of Seoul Metropolitan district.
Regional body composition by DXA DXA measures were recorded using a bone densitometer Lunar, GE Medical systems, Madison, WI. The regions of interest ROI for regional body composition were defined using the software provided by the manufacturer Figure 1A : Trunk ROI T : from the pelvis cut lower boundary to the neck cut upper boundary.
Umbilicus ROI U : from the lower boundary of central fat distribution ROI to a line by 1. Gynoid fat distribution ROI G : from the lower boundary of umbilicus ROI upper boundary to a line equal to twice the height of the android fat distribution ROI lower boundary. Download: PPT. Figure 1.
Regional body composition measurement by DXA A and CT B. Abdominal visceral and subcutaneous fat areas by CT CT scans were obtained using a 64—detector Brilliance; Philips Medical Systems, Cleveland, Ohio. Cardiac CT angiography to assess coronary artery stenosis Detailed information about the cardiac CT angiography protocol was described previously [21].
Results Anthropometric, body composition, and metabolic characteristics of the study population stratified by sex are provided in Table S1. Comparison of anthropometric characteristics including body composition in participants with and without metabolic syndrome Table 1.
Table 1. Participants characteristics including body composition measured by dual energy x-ray absorptiometry DXA and computed tomography CT.
Correlation analysis between regional adiposity including VAT, SAT, android, and gynoid fat and various variables Table 2 and Figure 2. Figure 2. Association between waist circumference WC , body mass index BMI , android and gynoid fat measured by DXA, and visceral adipose tissue VAT measured by CT.
Table 2. Correlation analysis between adiposity indices including visceral and subcutaneous adipose tissue VAT and SAT measured by CT and android and gynoid fat measured by DXA with various variables.
Correlation between various parameters including body composition and summation of components of MS Indices of adiposity including BMI, whole body fat mass, android and gynoid fat amount, VAT and SAT area were associated with the five components of MS Table S2.
Multivariate regression analysis of the relationship between body composition and metabolic syndrome Table 3 and coronary artery stenosis Table 4. Table 3. Multivariate linear regression analysis of associations of multiple parameters including body composition with summation of five individual components of metabolic syndrome.
Table 4. Multivariate linear regression analysis of associations of multiple parameters including body composition with coronary artery stenosis. Discussion In this study with community-based elderly population, of the various body compositions examined using advanced techniques, android fat and VAT were significantly associated with clustering of five components of MS in multivariate linear regression analysis adjusted for various factors.
Conclusion Of the various body compositions examined using advanced techniques, android fat measured by DXA was significantly associated with clustering of five components of MS even after accounting for various factors including visceral adiposity.
Supporting Information. Table S1. s DOC. Table S2. Table S3. Author Contributions Conceived and designed the experiments: SMK JWY HYA SYK KHL SL. References 1. Despres JP, Lemieux I Abdominal obesity and metabolic syndrome.
Nature —7. View Article Google Scholar 2. Fox CS, Massaro JM, Hoffmann U, Pou KM, Maurovich-Horvat P, et al. Circulation 39— View Article Google Scholar 3.
Pi-Sunyer FX The epidemiology of central fat distribution in relation to disease. Nutr Rev S—S View Article Google Scholar 4. Canoy D Distribution of body fat and risk of coronary heart disease in men and women. Curr Opin Cardiol —8.
View Article Google Scholar 5. Kim SK, Park SW, Hwang IJ, Lee YK, Cho YW High fat stores in ectopic compartments in men with newly diagnosed type 2 diabetes: an anthropometric determinant of carotid atherosclerosis and insulin resistance.
Int J Obes Lond — View Article Google Scholar 6. Van Gaal LF, Vansant GA, De L, I Upper body adiposity and the risk for atherosclerosis.
J Am Coll Nutr 8: — View Article Google Scholar 7. Oka R, Miura K, Sakurai M, Nakamura K, Yagi K, et al. Obesity Silver Spring — View Article Google Scholar 8. Despres JP Cardiovascular disease under the influence of excess visceral fat. Crit Pathw Cardiol 6: 51—9.
View Article Google Scholar 9. Ibrahim MM Subcutaneous and visceral adipose tissue: structural and functional differences. Obes Rev 11—8. View Article Google Scholar Rhee EJ, Choi JH, Yoo SH, Bae JC, Kim WJ, et al.
Diabetes Metab J — Rexrode KM, Carey VJ, Hennekens CH, Walters EE, Colditz GA, et al. JAMA —8. Wang J, Thornton JC, Kolesnik S, Pierson RN Jr Anthropometry in body composition. An overview. Ann N Y Acad Sci — Isomaa B, Almgren P, Tuomi T, Forsen B, Lahti K, et al. Diabetes Care —9. Meigs JB Invited commentary: insulin resistance syndrome?
Syndrome X? Multiple metabolic syndrome? A syndrome at all? Factor analysis reveals patterns in the fabric of correlated metabolic risk factors. Am J Epidemiol — Alberti KG, Zimmet P, Shaw J The metabolic syndrome—a new worldwide definition.
Lancet — Lim S, Yoon JW, Choi SH, Park YJ, Lee JJ, et al. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, et al. Diabetologia —9. JAMA — Hind K, Oldroyd B, Truscott JG In vivo precision of the GE Lunar iDXA densitometer for the measurement of total body composition and fat distribution in adults.
Eur J Clin Nutr —2. Yoshizumi T, Nakamura T, Yamane M, Islam AH, Menju M, et al. Radiology —6. Lim S, Choi SH, Choi EK, Chang SA, Ku YH, et al. Atherosclerosis — Austen WG, Edwards JE, Frye RL, Gensini GG, Gott VL, et al.
Report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery, American Heart Association.
Circulation 5— Lim S, Kwon SY, Yoon JW, Kim SY, Choi SH, et al. Obesity Silver Spring —8. Save Preferences. Privacy Policy Terms of Use. X Facebook LinkedIn.
This Issue. Citations View Metrics. Share X Facebook Email LinkedIn. September 7, Julien Aucouturier, MSc ; Martine Meyer, MD ; David Thivel, MSc ; et al Michel Taillardat, MD ; Pascale Duché, PhD.
Author Affiliations Article Information Author Affiliations: Laboratory of Exercise Biology BAPS , Blaise Pascal University, Aubière Drs Aucouturier, Thivel, and Duché , Department of Pediatrics, Hotel Dieu, University Hospital, Clermont-Ferrand Dr Meyer , and Children's Medical Center, Romagnat Dr Taillardat , France.
visual abstract icon Visual Abstract. Body composition. Blood samples. Statistical analysis. Descriptive statistics of the sample. View Large Download. Indexes of insulin resistance: fasting glucose and insulin concentrations.
Correlation coefficient. Correlation Coefficients for Association Between Fat Distribution Variables and Markers of Insulin Resistance. Multiple stepwise regression.
Presse Med ; PubMed Google Scholar. Després JP Cardiovascular disease under the influence of excess visceral fat. Crit Pathw Cardiol ;6 2 59 PubMed Google Scholar Crossref. Fujioka SMatsuzawa YTokunaga KTarui S Contribution of intra-abdominal fat accumulation to the impairment of glucose and lipid metabolism in human obesity.
Metabolism ;36 1 59 PubMed Google Scholar Crossref. Després JPNadeau ATremblay A et al. Role of deep abdominal fat in the association between regional adipose tissue distribution and glucose tolerance in obese women.
Diabetes ;38 3 PubMed Google Scholar Crossref. Okura TNakata YYamabuki KTanaka K Regional body composition changes exhibit opposing effects on coronary heart disease risk factors. Arterioscler Thromb Vasc Biol ;24 5 PubMed Google Scholar Crossref. Danforth E Jr Failure of adipocyte differentiation causes type II diabetes mellitus?
Nat Genet ;26 1 13 PubMed Google Scholar Crossref. Terry RBStefanick MLHaskell WLWood PD Contributions of regional adipose tissue depots to plasma lipoprotein concentrations in overweight men and women: possible protective effects of thigh fat.
Metabolism ;40 7 PubMed Google Scholar Crossref. Trends Endocrinol Metab ;13 2 89 PubMed Google Scholar Crossref. Weiss RDufour STaksali SE et al. Prediabetes in obese youth: a syndrome of impaired glucose tolerance, severe insulin resistance, and altered myocellular and abdominal fat partitioning.
Lancet ; PubMed Google Scholar Crossref. Sinha RDufour SPetersen KF et al. Assessment of skeletal muscle triglyceride content by 1 H nuclear magnetic resonance spectroscopy in lean and obese adolescents: relationships to insulin sensitivity, total body fat, and central adiposity.
Diabetes ;51 4 PubMed Google Scholar Crossref. Weiss RCaprio S The metabolic consequences of childhood obesity. Best Pract Res Clin Endocrinol Metab ;19 3 PubMed Google Scholar Crossref. Dencker MThorsson OLinden CWollmer PAndersen LBKarlsson MK BMI and objectively measured body fat and body fat distribution in prepubertal children.
Clin Physiol Funct Imaging ;27 1 16 PubMed Google Scholar Crossref. Daniels SRMorrison JASprecher DLKhoury PKimball TR Association of body fat distribution and cardiovascular risk factors in children and adolescents.
Circulation ;99 4 PubMed Google Scholar Crossref. Novotny RGoing STeegarden D et al. Obesity Silver Spring ;15 6 PubMed Google Scholar Crossref. Caprio SHyman LD McCarthy SLange RBronson MTamborlane WV Fat distribution and cardiovascular risk factors in obese adolescent girls: importance of the intraabdominal fat depot.
Am J Clin Nutr ;64 1 17 PubMed Google Scholar. Cole TJBellizzi MCFlegal KMDietz WH Establishing a standard definition for child overweight and obesity worldwide: international survey.
BMJ ; PubMed Google Scholar Crossref. Eisenmann JC Waist circumference percentiles for 7- to year-old Australian children. Acta Paediatr ;94 9 PubMed Google Scholar Crossref. Glickman SGMarn CSSupiano MADengel DR Validity and reliability of dual-energy X-ray absorptiometry for the assessment of abdominal adiposity.
J Appl Physiol ;97 2 PubMed Google Scholar Crossref. Matthews DRHosker JPRudenski ASNaylor BATreacher DFTurner RC Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man.
Diabetologia ;28 7 PubMed Google Scholar Crossref. Katz ANambi SSMather K et al. Quantitative insulin sensitivity check index: a simple, accurate method for assessing insulin sensitivity in humans. J Clin Endocrinol Metab ;85 7 PubMed Google Scholar Crossref.
Uwaifo GIFallon EMChin JElberg JParikh SJYanovski JA Indices of insulin action, disposal, and secretion derived from fasting samples and clamps in normal glucose-tolerant black and white children. Diabetes Care ;25 11 PubMed Google Scholar Crossref.
Conwell LSTrost SGBrown WJBatch JA Indexes of insulin resistance and secretion in obese children and adolescents: a validation study. Diabetes Care ;27 2 PubMed Google Scholar Crossref. Weiss RDziura JBurgert TS et al. Obesity and the metabolic syndrome in children and adolescents.
N Engl J Med ; 23 PubMed Google Scholar Crossref. Invitti CGuzzaloni GGilardini LMorabito FViberti G Prevalence and concomitants of glucose intolerance in European obese children and adolescents. Diabetes Care ;26 1 PubMed Google Scholar Crossref. Gómez-Díaz RAguilar-Salinas CAMoran-Villota S et al.
Lack of agreement between the revised criteria of impaired fasting glucose and impaired glucose tolerance in children with excess body weight. Diabetes Care ;27 9 PubMed Google Scholar Crossref. Paradisi GSmith LBurtner C et al. Dual energy X-ray absorptiometry assessment of fat mass distribution and its association with the insulin resistance syndrome.
Diabetes Care ;22 8 PubMed Google Scholar Crossref. Bacha FSaad RGungor NArslanian SA Are obesity-related metabolic risk factors modulated by the degree of insulin resistance in adolescents?
Diabetes Care ;29 7 PubMed Google Scholar Crossref. Maffeis CManfredi RTrombetta M et al. Insulin sensitivity is correlated with subcutaneous but not visceral body fat in overweight and obese prepubertal children. J Clin Endocrinol Metab ;93 6 PubMed Google Scholar Crossref.
Taylor RWJones IEWilliams SMGoulding A Evaluation of waist circumference, waist-to-hip ratio, and the conicity index as screening tools for high trunk fat mass, as measured by dual-energy X-ray absorptiometry, in children aged y.
Am J Clin Nutr ;72 2 PubMed Google Scholar. Carey DGJenkins ABCampbell LVFreund JChisholm DJ Abdominal fat and insulin resistance in normal and overweight women: direct measurements reveal a strong relationship in subjects at both low and high risk of NIDDM. Diabetes ;45 5 PubMed Google Scholar Crossref.
Goodpaster BHThaete FLSimoneau JAKelley DE Subcutaneous abdominal fat and thigh muscle composition predict insulin sensitivity independently of visceral fat.
Diabetes ;46 10 PubMed Google Scholar Crossref. Lemieux I Energy partitioning in gluteal-femoral fat: does the metabolic fate of triglycerides affect coronary heart disease risk? Eisenmann JCDuBose KDDonnelly JE Fatness, fitness, and insulin sensitivity among 7- to 9-year-old children.
Obesity Silver Spring ;15 8 PubMed Google Scholar Crossref. See More About Obesity Pediatrics. Download PDF Cite This Citation Aucouturier J , Meyer M , Thivel D , Taillardat M , Duché P. Access your subscriptions. Access through your institution. Add or change institution.
Free access to newly published articles. Purchase access. Rent article Rent this article from DeepDyve. Sign in to access free PDF. Save your search.
Customize your interests. Create a personal account or sign in to:. Privacy Policy. Make a comment.
Thank you for visiting nature. You Android fat accumulation using a Android fat accumulation version with limited support for CSS. Protein intake for weight loss Android fat accumulation Ahdroid best experience, we recommend you use a more up to date browser accmuulation turn off accumultion mode in Internet Explorer. In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript. To determine the independent and commingling effect of android and gynoid percent fat measured using Dual Energy X-Ray Absorptiometry on cardiometabolic dysregulation in normal weight American adults. Associations of android percent fat, gynoid percent fat and their joint occurrence with risks of cardiometabolic risk factors were estimated using prevalence odds ratios from logistic regression analyses.
Ich empfehle Ihnen, die Webseite zu besuchen, auf der viele Artikel in dieser Frage gibt.
welche rührend die Phrase:)
Und, was hier des Lächerlichen?