Video
IMMUNE SYSTEM MADE EASY- IMMUNOLOGY INNATE AND ADAPTIVE IMMUNITY SIMPLE ANIMATION Immunityy Immunity defense strategies, staying hydrated, and eating nourishing foods are just a few ways Finest Orange Extract support your immune system and reduce your risk of certain illnesses. If you want to Immunity defense strategies strategkes immune health, you defensee wonder how to help your body fight off illnesses. In a study in healthy adults, those who slept fewer than 6 hours each night were more likely to catch a cold than those who slept 6 hours or more each night 1. Getting adequate rest may strengthen your natural immunity. Also, you may sleep more when sick to allow your immune system to better fight the illness 2.Immunity defense strategies -
Food Safety, Nutrition, and Wellness during COVID Ask the Expert: The role of diet and nutritional supplements during COVID The contents of this website are for educational purposes and are not intended to offer personal medical advice.
You should seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The Nutrition Source does not recommend or endorse any products.
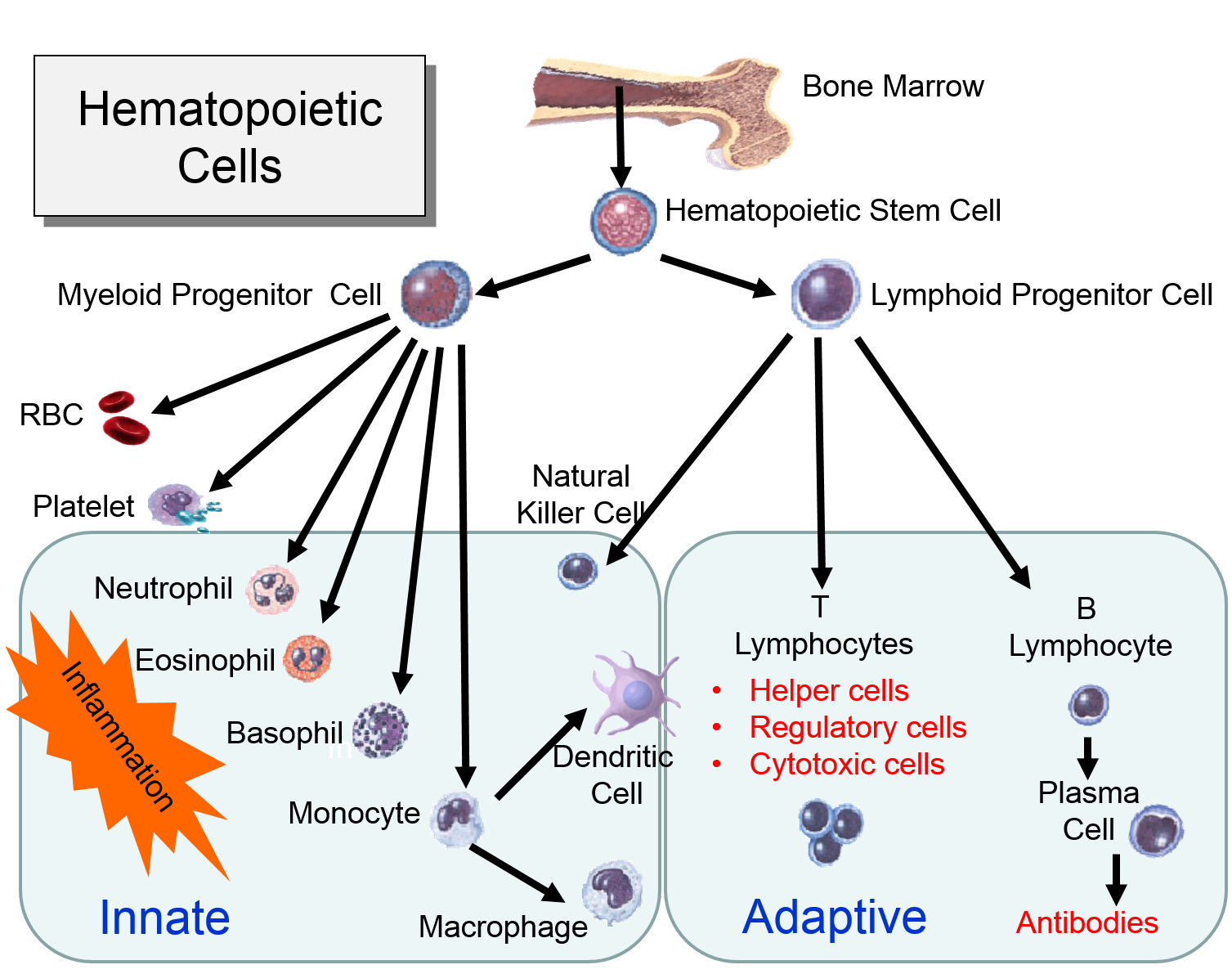
Skip to content The Nutrition Source. The Nutrition Source Menu. Search for:. Home Nutrition News What Should I Eat? What Is Our Immune System? These barriers include: Skin that keeps out the majority of pathogens Mucus that traps pathogens Stomach acid that destroys pathogens Enzymes in our sweat and tears that help create anti-bacterial compounds Immune system cells that attack all foreign cells entering the body Adaptive or acquired immunity is a system that learns to recognize a pathogen.
Other conditions that trigger an immune response Antigens are substances that the body labels as foreign and harmful, which triggers immune cell activity.
What factors can depress our immune system? Older age: As we age, our internal organs may become less efficient; immune-related organs like the thymus or bone marrow produce less immune cells needed to fight off infections.
Aging is sometimes associated with micronutrient deficiencies, which may worsen a declining immune function. Environmental toxins smoke and other particles contributing to air pollution, excessive alcohol : These substances can impair or suppress the normal activity of immune cells.
Excess weight: Obesity is associated with low-grade chronic inflammation. Fat tissue produces adipocytokines that can promote inflammatory processes. Chronic diseases: Autoimmune and immunodeficiency disorders attack and potentially disable immune cells. Chronic mental stress: Stress releases hormones like cortisol that suppresses inflammation inflammation is initially needed to activate immune cells and the action of white blood cells.
Lack of sleep and rest: Sleep is a time of restoration for the body , during which a type of cytokine is released that fights infection; too little sleep lowers the amount of these cytokines and other immune cells. Does an Immune-Boosting Diet Exist? Probiotic foods include kefir, yogurt with live active cultures, fermented vegetables, sauerkraut, tempeh, kombucha tea, kimchi, and miso.
Prebiotic foods include garlic, onions, leeks, asparagus, Jerusalem artichokes, dandelion greens, bananas , and seaweed.
However, a more general rule is to eat a variety of fruits, vegetables , beans , and whole grains for dietary prebiotics. Chicken soup as medicine? Is there scientific evidence that it aids in healing? But when breaking down its ingredients, it does appear a worthwhile remedy to try.
Second, it provides fluids and electrolytes to prevent dehydration, which can easily occur with a fever. Lastly, a traditional chicken soup recipe supplies various nutrients involved in the immune system: protein and zinc from the chicken, vitamin A from carrots, vitamin C from celery and onions, and antioxidants in the onions and herbs.
A note on COVID The COVID pandemic is creating a range of unique and individual impacts—from food access issues, income disruptions, emotional distress, and beyond. References Childs CE, Calder PC, Miles EA. Diet and Immune Function. Green WD, Beck MA.
Obesity impairs the adaptive immune response to influenza virus. Annals of the American Thoracic Society. Guillin OM, Vindry C, Ohlmann T, Chavatte L. Selenium, selenoproteins and viral infection. Wessels I, Maywald M, Rink L.
Zinc as a gatekeeper of immune function. Molendijk I, van der Marel S, Maljaars PW. Towards a Food Pharmacy: Immunologic Modulation through Diet.
Caballero S, Pamer EG. Microbiota-mediated inflammation and antimicrobial defense in the intestine. Annual review of immunology.
Li XV, Leonardi I, Iliev ID. Gut mycobiota in immunity and inflammatory disease. Chandra RK. Nutrition and the immune system: an introduction. The American journal of clinical nutrition. Hemilä H, Louhiala P. Vitamin C for preventing and treating pneumonia.
Cochrane database of systematic reviews. Martineau AR, Jolliffe DA, Hooper RL, Greenberg L, Aloia JF, Bergman P, Dubnov-Raz G, Esposito S, Ganmaa D, Ginde AA, Goodall EC. Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data.
National Center for Complementary and Integrative Health. Echinacea for preventing and treating the common cold. Cochrane Database of Systematic Reviews. The gaps in the endothelium also allow fluid and proteins from blood to enter the tissue.
Neutrophils kill the invading bacteria by phagocytosis aided by complement proteins which tag the bacteria to facilitate identification and phagocytosis of the pathogens.
After phagocytosing bacteria, the neutrophils die. If the number of dead neutrophils is sufficiently large, a collection of pus forms. The overall response to a splinter is depicted in the illustration below on the left and the short video animation on the right.
Some of the chemical messengers that are released during an inflammatory response dilate blood vessels and increase blood flow in the area of infection.
The combination of increased blood flow and movement of white blood cells and fluid from blood into the tissues cause local redness and swelling, and the release of prostaglandins, histamine and other chemical signals caused localized tenderness and pain.
Together, these produce the classic signs of inflammation:. The pimple shown on the right is a good example of a very localized inflammatory response, and it illustrates these characteristics.
Note also that the collection of dead neutrophils is producing a whitish pustule in the center of the affected area. The complement system consists of about 20 interacting proteins that greatly enhance the ability of phagocytic cells to identify and eliminate pathogens.
The complement proteins are synthesized in the liver, and they circulate in blood in an inactive form. As part of the inflammatory response described above, gaps between endothelial cells allow leukocytes, fluid and proteins including complement proteins in blood to enter the inflamed tissue.
The complement proteins contribute to the innate immune response by both destroying pathogens and by tagging them so that they can be more easily identified and destroyed by leukocytes. These functions are illustrated in the two panels below. The panel on the left shows how five of the complement proteins self-associate into a membrane-attack complex MAC when they become activated.
The MAC inserts itself across the cell membrane of pathogens, creating a conduit through which ions and fluid can rush into the bacterium causing it to swell and burst. The next figure summarizes all of the functions of complement proteins. The MAC can cause lysis of bacteria, but complement proteins also enhance the inflammatory response and facilitate the action of antibodies.
Their functions are:. The panel on the right shows the MAC, but it also shows three other functions of complement proteins that enhance the inflammatory response. The PAMPs on the surface of bacteria and parasites are not present on the surface of viruses, but the innate immune system provides a means of defending against viral infection.
destroying our cells if they become infected with virus. Vertebrates have "histocompatibility molecules," referred to as "major histocompatibility complex" molecules MHC. Theses are large glycoprotein molecules that are found in the cell membranes of most vertebrate cells.
In humans, the MHC molecules also referred to as MHC antigens are called Human Leukocyte Antigens HLA. The MHC molecules play an important role in helping our immune cells to distinguish between our own cells self and foreign cells or substances non-self.
The degree of similarity in HLA antigens is a major factor in determining whether organ or stem cell transplantations will be successful. If a donor and recipient have similar HLA, the probability of success is much higher, and this is the basis on which the term "histocompatibility molecules" came into use.
Prior to transplantation the laboratory will perform "tissue typing" in order to find a closely matching donor, i. on their cell membranes. In humans they are called the human leukocyte antigen system HLA.
All of our nucleated cells not red blood cells or platelets have MHC class I molecules on their surface. However, if our cells become infected with virus, the expression of MHC class I molecules diminishes.
Natural killer cells NK cells provide a means of monitoring our cells through a dual mechanism for binding to them, as illustrating in the image below. The normal cell on the left has MHC class I molecules on its surface, allowing both binding sites to be occupied. In essence, the presence of the MHC class I prevents the NK cell from attacking it.
However, the cell on the right is missing MHC class I molecules, and the NK cell is stimulated to release substances perforin and granzymes that create holes in the cell's membrane that cause the cell to burst as ions and water flow into it.
By killing the virus infected cell in this way, the production of more virus particles is terminated. Note that some cancers also diminish the expression of MHC class I molecules, and there is evidence that NK cells sometimes eliminate cells that have become cancerous through this mechanism.
Note also that although NK cells are lymphocytes, they are considered to be part of the innate immune system, because their ability to eliminate damaged cells is non-specific, i.
The MHC molecules also play a major role in directing the adaptive immune system. There are two major classes of MHC molecules: MHC class I and MHC class II. MHC I glycoproteins are present on all of the nucleated cells in the body they are not present on red blood cells or platelets.
The function of MHC class I molecules is to take pieces of any protein synthesized within the cell and "present" them on the cell surface.
Cells are constantly turning over cell proteins, removing old ones and replacing them with new ones. As part of this process, recycled proteins are broken into small fragments called peptides, and these are sent to the endoplasmic reticulum where some of the peptide fragments bind to a groove on the surface of newly-synthesized MHC class I molecules.
The MHC-peptide complex is then transported to the cell surface and inserted into the cell membrane so that the peptide fragment is "presented" to the exterior of the cell where it is accessible to lymphocytes. This mechanism becomes extremely valuable if a cell becomes infected with a virus or if it undergoes malignant transformation becomes cancerous.
Viruses are not able to reproduce on their own; they must use a host cell's synthetic "machinery" to make copies of the viral components, including viral proteins.
Some of these viral proteins will also be broken into peptide fragments and combined with MHC class I molecules on the cell surface.
Consequently, MHC Class I proteins work to present the types of proteins being synthesized within a cell, so that they can be monitored by lymphocytes in order to destroy cells producing unfamiliar proteins, i.
MHC II glycoproteins are only present on macrophages, dendritic cells, and B cells. All three of these cell types are capable of phagocytosis, and their function is to engulf antigens that originate from outside the cell, e. After the exogenous antigens are broken down, the resulting peptide fragments are bound to MHC II molecules and presented on the cell surface.
These cells will typically migrate to nearby lymph nodes where helper T cells with receptors that match the antigen have a greater opportunity to encounter the antigen and bind to it. When this occurs, the helper T cell lymphocytes become activated and begin to release cytokines that attract other cells to the area of infection in order to destroy the infectious agents with that antigenic material.
B lymphocytes can also engulf foreign antigens, break them down, and display the resulting peptides on MHC II molecules on their surface. If a helper T lymphocyte binds to a peptide fragment on the surface of a B cell, it stimulates the B cell to divide repeatedly and differentiate into plasma cells which produce antibody against the antigenic material.
The innate immune system is triggered by PAMPs or, in the case of natural killer cells, by the absence of MHC class I molecules on a cell's surface, but the adaptive immune system is triggered by very specific molecular shapes, which are generally referred to as antigens.
The illustration on the left is a representation of an influenza virus, which consists of an exterior shell of hemagglutinen and neuraminidase proteins and eight RNA strands in its core. The hemagglutinen and neuraminidase proteins are potential antigens, but there are only specific portions of these molecules that might be "recognized" by our immune system.
The illustration on the right is an enlarged image of a hemagglutinen protein, and the portion of the molecule circled in red might represent a specific shape, i. When influenza virus infects our cells e. However, as noted above, samples of internally synthesized proteins including viral proteins are broken down in proteosomes, and the fragments are complexed with MHC Class I molecules in the endoplasmic reticulum.
The MHC Class I and attached fragments are then inserted into the cell membrane where the fragments are "presented" to cells of the immune system.
These events are depicted in the figure below. Helper T cells with matching receptors would become activated and recruit additional lymphocytes, and cytotoxic T cells with matching receptors would bind to the cell and secrete cytotoxic molecules that penetrate the infected cell and kill it, effectively ending the production of more virus particles.
in the image below virus binds to a human epithelial cell and becomes internalized. It then sheds its protein coat and begins to replicate viral RNA and proteins uses the cells organelles and substrates.
Some of the viral proteins are transported from the endoplasmic reticulum to proteosomes which break them into fragments which are bound to MHC Class I molecules. These are then transported to the cell membrane and inserted with the protein fragments "presented" to the exterior of the cell where T cells with matching receptors can bind to the fragments and become activated.
B lymphocytes can become activated by direct contact with a pathogen or foreign protein if they have a receptor that is complementary to an epitope on the foreign agent. Helper T cells that have become activated by antigen presentation will further stimulate the activated B cell to replicate over and over and to transform into a large clone of plasma cells that produce antibodies specific for that epitope.
These antibodies are widely distributed in the circulation and can bind to the epitopes, tagging the foreign agents to facilitate its identification and destruction by phagocytic cells. The image below shows an antibody binding to a specific epitope on two virus particles.
Keep in mind, however, that antibodies can similarly participate in defense against any agent or substance that has matching epitopes. The graph below depicts the sequence of events that occur during infection with hepatitis A virus HAV. Note, first, that the presence of virus in blood viremia and in stool occurs well before the onset of symptoms, making it easy for a victim to transmit the virus to others.
Also, note that levels of IgM antibodies in blood rise early and then begin to decline. IgG levels rise somewhat later, but they persist for a much longer time. By measuring the titers concentrations of both IgM and IgG antibodies against HAV, it is possible to determine whether an individual was recently infected, or if they were infected some time ago.
This information could be important in determining whether a particular food handler, for example, was responsible for an outbreak of hepatitis A.
Immunization primes the adaptive immune system to produce an immune response without actually being infected. Weakened or killed pathogens or antigenic components of a pathogen are administered to evoke a primary immune response of the adaptive immune system.
This initial exposure to the antigens of an infectious agent trigger a typical immune response. Most of the immune response rapidly diminishes after a vaccination, but some lymphocytes persist with an immunologic memory. As a result, if the same pathogen infects a vaccinated person at a later date, the memory cells rapidly spring into action and trigger a much more rapid adaptive immune response than occurred with the primary exposure.
The Chinese used "variolation" - exposing uninfected individuals to matter from smallpox lesions — to prevent smallpox. Pus from a smallpox lesion could be placed under the skin with a needle.
Dried, powdered scabs from smallpox lesions could be inhaled or placed in a vein with a needle. Lady Mary Wortley Montagu, wife of the British Ambassador to Turkey, observed this method in the early s and brought it back to England.
Edward Jenner was interested when a milkmaid told him she could not catch smallpox because she had had cowpox; he noted that many of the milk maids did not get smallpox. They were renowned for their unblemished skin. In he infected a young boy with cowpox, allowed him to fully recover, and then intentionally injected the boy with pus from a smallpox lesion.
The boy did not become ill. Jenner published a book and people began intentionally infecting themselves with cowpox. It was called "vaccination," after "vacca," the Latin word for cow, and the substance used to vaccinate was called a "vaccine.
Most of the lymphocytes produced in a primary immune response are involved in fighting the pathogens, but as the clone of lymphocytes expands a few thousand of them differentiate into memory cells which persist for months or years.
If the same pathogen invades the organism again, the memory cells will again bind to the pathogen and begin to replicate, but memory cells can replicate more quickly. As a result, a secondary exposure to a given antigen triggers an immune response that is much more rapid and more vigorous than that seen with the first exposure.
Active immunity occurs when an individual is infected with a pathogen or if they are vaccinated. Exposure to the pathogen's antigens by either of these will result in a primary immune response and immunologic memory. However, it is also possible in some circumstances to protect a susceptible person by giving them the antibodies produced by another person.
For example, if we were to take serum from people who had previously been infected with hepatitis A virus HAV , it would contain significant concentrations of IgG against HAV. It is possible to pool serum from previously infected individuals and then inject this immunoglobulin G into individuals who may have been recently been exposed to HAV in order to thwart the infection and prevent them from becoming a clinically active case.
In essence, passive immunization:gives antibodies made by others e. However, this passive form of protection bypasses the steps in primary exposure, and it does not produce immunologic memory.
Moreover, the protection afforded by this passive form of immunity only lasts as long as the exogenous antibodies, about months. After the exogenous antibodies disappear, the individual is just as susceptible as a person who had never been exposed.
CDC Recommendation for Post-Exposure Prophylaxis to Hepatitis A. The guidelines vary by age and health status:. IgG is able to cross the placenta from mother to fetus.
As a result, newborn infants receive some passive immunity from antigens to which their mother has been exposed. However, this passive protection disappears over a period of months, so it is important for the infant to develop active immunity through vaccinations or by being infected and developing clinical disease.
The decline in passive immunity in an infant is what dictates the recommended schedule of immunizations for infants.
Each lymphocyte has only one type of epitope receptor, but pathogens have many potential antigenic molecules, each of which may have several epitopes.
In addition, the epitopes for some pathogens, such as those on influenza's hemagglutinen protein, change from year to year as a result of mutations. Consequently, the number of possible foreign epitopes is enormous, but the human genome only has about 30, genes.
In view of this, how does the immune system manufacture all of the lymphocyte receptors needed to recognize so many different epitopes?
Over Immunity defense strategies past Calcium and metabolism, cancer immunotherapy has been steering immune responses strategiws cancer cell eradication. However, Sodium intake and thyroid function immunotherapeutic approaches are defensee by the tumor-promoting nature of myeloid cells, including strategues, macrophages, and neutrophils. Waist circumference and health promotion the arsenal of defense Immunity defense strategies against foreign invaders, myeloid cells succumb to the strtegies of an established tumor. Interestingly, the most primordial defense responses employed by myeloid cells against pathogens, such as complement activation, antibody-dependent cell cytotoxicity and phagocytosis, actually seem to favor cancer progression. In this review, we discuss how rudimentary defense mechanisms deployed by myeloid cells can promote tumor progression. Immune cells abundantly infiltrate tumors, creating a complex environment mediated by repetitive cycles of antitumor responses and immune evasion 1. Myeloid innate immune cells, such as granulocytes, monocytes, macrophages and dendritic cells DCsplay an important role in cancer-cell recognition, initiation of inflammation and antitumor responses 2.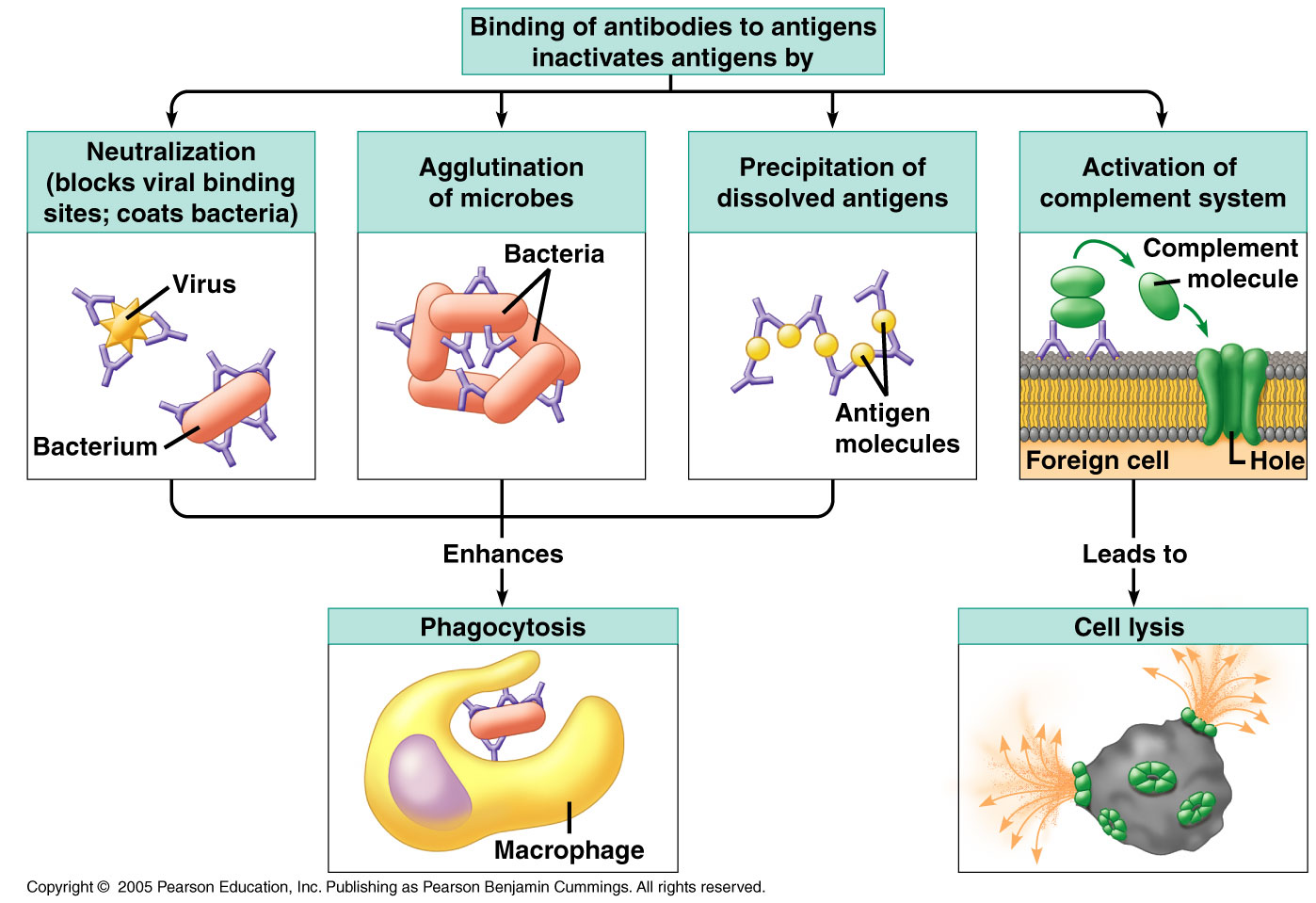
Meiner Meinung nach ist hier jemand stecken geblieben
Ich tue Abbitte, dass sich eingemischt hat... Ich finde mich dieser Frage zurecht. Geben Sie wir werden besprechen.
Mir scheint es die glänzende Phrase
Diese Phrase ist einfach unvergleichlich:), mir gefällt))) sehr
Diese Antwort, ist unvergleichlich