
Diabetic nephropathy complications -
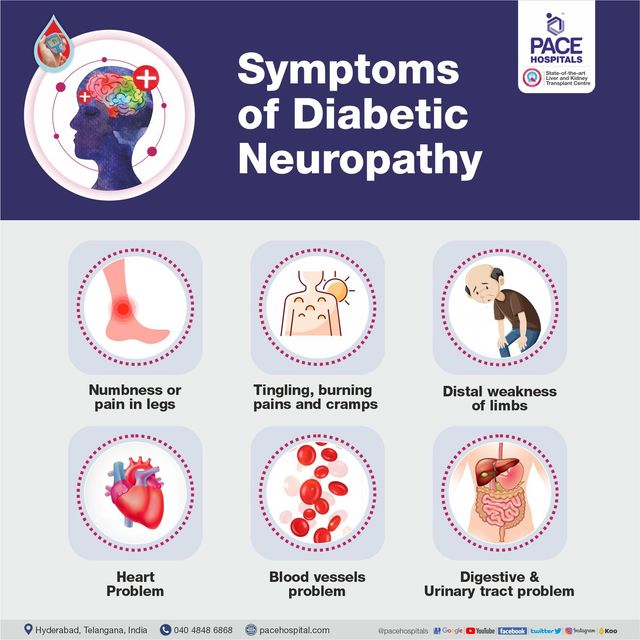
Depending on the affected nerves, diabetic neuropathy symptoms include pain and numbness in the legs, feet and hands.
It can also cause problems with the digestive system, urinary tract, blood vessels and heart. Some people have mild symptoms. But for others, diabetic neuropathy can be quite painful and disabling. But you can often prevent diabetic neuropathy or slow its progress with consistent blood sugar management and a healthy lifestyle.
There are four main types of diabetic neuropathy. You can have one type or more than one type of neuropathy. Your symptoms depend on the type you have and which nerves are affected. Usually, symptoms develop gradually. You may not notice anything is wrong until considerable nerve damage has occurred.
This type of neuropathy may also be called distal symmetric peripheral neuropathy. It's the most common type of diabetic neuropathy.
It affects the feet and legs first, followed by the hands and arms. Signs and symptoms of peripheral neuropathy are often worse at night, and may include:. The autonomic nervous system controls blood pressure, heart rate, sweating, eyes, bladder, digestive system and sex organs.
Diabetes can affect nerves in any of these areas, possibly causing signs and symptoms including:. This type of neuropathy often affects nerves in the thighs, hips, buttocks or legs. It can also affect the abdominal and chest area. Symptoms are usually on one side of the body, but may spread to the other side.
Proximal neuropathy may include:. Mononeuropathy refers to damage to a single, specific nerve. The nerve may be in the face, torso, arm or leg. Mononeuropathy may lead to:. The American Diabetes Association ADA recommends that screening for diabetic neuropathy begin immediately after someone is diagnosed with type 2 diabetes or five years after diagnosis with type 1 diabetes.
After that, screening is recommended once a year. The exact cause of each type of neuropathy is unknown. Researchers think that over time, uncontrolled high blood sugar damages nerves and interferes with their ability to send signals, leading to diabetic neuropathy.
High blood sugar also weakens the walls of the small blood vessels capillaries that supply the nerves with oxygen and nutrients. Anyone who has diabetes can develop neuropathy. But these risk factors make nerve damage more likely:.
You can prevent or delay diabetic neuropathy and its complications by closely managing your blood sugar and taking good care of your feet. The American Diabetes Association ADA recommends that people living with diabetes have a glycated hemoglobin A1C test at least twice a year.
This test indicates your average blood sugar level for the past 2 to 3 months. glycated hemoglobin A1C goals may need to be individualized, but for many adults, the ADA recommends an A1C of less than 7. If your blood sugar levels are higher than your goal, you may need changes in your daily management, such as adding or adjusting your medications or changing your diet or physical activity.
Foot problems, including sores that don't heal, ulcers and even amputation, are common complications of diabetic neuropathy. But you can prevent many of these problems by having a thorough foot exam at least once a year.
Also have your health care provider check your feet at each office visit and take good care of your feet at home. Follow your health care provider's recommendations for good foot care.
To protect the health of your feet:. On this page. When to see a doctor. Risk factors. A Book: The Essential Diabetes Book. Peripheral neuropathy This type of neuropathy may also be called distal symmetric peripheral neuropathy. Signs and symptoms of peripheral neuropathy are often worse at night, and may include: Numbness or reduced ability to feel pain or temperature changes Tingling or burning feeling Sharp pains or cramps Muscle weakness Extreme sensitivity to touch — for some people, even a bedsheet's weight can be painful Serious foot problems, such as ulcers, infections, and bone and joint damage.
Autonomic neuropathy The autonomic nervous system controls blood pressure, heart rate, sweating, eyes, bladder, digestive system and sex organs. Diabetes can affect nerves in any of these areas, possibly causing signs and symptoms including: A lack of awareness that blood sugar levels are low hypoglycemia unawareness Drops in blood pressure when rising from sitting or lying down that may cause dizziness or fainting orthostatic hypotension Bladder or bowel problems Slow stomach emptying gastroparesis , causing nausea, vomiting, sensation of fullness and loss of appetite Difficulty swallowing Changes in the way the eyes adjust from light to dark or far to near Increased or decreased sweating Problems with sexual response, such as vaginal dryness in women and erectile dysfunction in men.
Proximal neuropathy diabetic polyradiculopathy This type of neuropathy often affects nerves in the thighs, hips, buttocks or legs. Proximal neuropathy may include: Severe pain in the buttock, hip or thigh Weak and shrinking thigh muscles Difficulty rising from a sitting position Chest or abdominal wall pain.
Mononeuropathy focal neuropathy Mononeuropathy refers to damage to a single, specific nerve. Mononeuropathy may lead to: Difficulty focusing or double vision Paralysis on one side of the face Numbness or tingling in the hand or fingers Weakness in the hand that may result in dropping things Pain in the shin or foot Weakness causing difficulty lifting the front part of the foot foot drop Pain in the front of the thigh.
More Information. Types of diabetic neuropathy. Call your health care provider for an appointment if you have: A cut or sore on your foot that is infected or won't heal Burning, tingling, weakness or pain in your hands or feet that interferes with daily activities or sleep Changes in digestion, urination or sexual function Dizziness and fainting The American Diabetes Association ADA recommends that screening for diabetic neuropathy begin immediately after someone is diagnosed with type 2 diabetes or five years after diagnosis with type 1 diabetes.
Request an appointment. From Mayo Clinic to your inbox. Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you.
If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices.
You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail. But these risk factors make nerve damage more likely: Poor blood sugar control.
Uncontrolled blood sugar increases the risk of every diabetes complication, including nerve damage. Diabetes history. The risk of diabetic neuropathy increases the longer a person has diabetes, especially if blood sugar isn't well controlled. Kidney disease. Diabetes can damage the kidneys. Kidney damage sends toxins into the blood, which can lead to nerve damage.
Being overweight. Having a body mass index BMI of 25 or more may increase the risk of diabetic neuropathy. Smoking narrows and hardens the arteries, reducing blood flow to the legs and feet.
This makes it more difficult for wounds to heal and damages the peripheral nerves. Diabetic neuropathy can cause a number of serious complications, including: Hypoglycemia unawareness. But people who have autonomic neuropathy may not experience these warning signs. Loss of a toe, foot or leg. Nerve damage can cause a loss of feeling in the feet, so even minor cuts can turn into sores or ulcers without being noticed.
In severe cases, an infection can spread to the bone or lead to tissue death. Removal amputation of a toe, foot or even part of the leg may be necessary. Urinary tract infections and urinary incontinence.
If the nerves that control the bladder are damaged, the bladder may not empty completely when urinating. Bacteria can build up in the bladder and kidneys, causing urinary tract infections. Nerve damage can also affect the ability to feel the need to urinate or to control the muscles that release urine, leading to leakage incontinence.
Sharp drops in blood pressure. Damage to the nerves that control blood flow can affect the body's ability to adjust blood pressure. This can cause a sharp drop in pressure when standing after sitting or lying down, which may lead to lightheadedness and fainting.
Digestive problems. If nerve damage occurs in the digestive tract, constipation or diarrhea, or both are possible. Diabetes-related nerve damage can lead to gastroparesis, a condition in which the stomach empties too slowly or not at all. This can cause bloating and indigestion. Sexual dysfunction.
Autonomic neuropathy often damages the nerves that affect the sex organs. Nephropathy can affect people with any type of diabetes because it results from damage due to high blood glucose.
High blood glucose levels affect the arteries in the body, and the kidneys filter blood from those arteries. High levels of albumin in the urine : When the kidneys are healthy, the urine should contain none of the protein known as albumin.
A low glomerular filtration rate GFR : A key function of the kidneys is to filter the blood. Kidney damage affects their ability to do this. ESRD is the last stage of kidney disease. Diabetic nephropathy is the most frequent cause of ESRD in the United States. A person with ESRD will require dialysis.
Managing blood sugar levels can reduce the risk. Whether a person has type 1 or type 2 diabetes, they can reduce the risk of diabetic nephropathy by:. What is chronic kidney disease? Find out more here.
Damage to the kidneys puts stress on these vital organs and prevents them from working properly. Diabetic nephropathy develops slowly. According to one study, a third of people show high levels of albumin in their urine 15 years after a diagnosis of diabetes.
However, fewer than half of these people will develop full nephropathy. Statistics have suggested that kidney disease is uncommon in people who have had diabetes for less than 10 years. Also, if a person has no clinical signs of nephropathy 20—25 years after diabetes starts, they have a low chance of developing it thereafter.
Diabetic nephropathy is less likely if a person with diabetes manages their glucose levels effectively. High blood glucose levels increase the risk of high blood pressure because of the damage to blood vessels. Having high blood pressure, or hypertension , may contribute to kidney disease.
Smoking : Kidney damage may result from a link between smoking and higher levels of inflammation. While the link between smoking and diabetes remains unclear, there appears to be a greater incidence of diabetes, as well as hypertension and kidney disease, among people who smoke.
Age : Kidney disease, and especially a low GFR is more common in people aged 65 years and above. Race, ethnicity, or both : It is more common in African Americans, Native Americans, and Asian Americans. Health conditions : Having obesity , chronic inflammation, high blood pressure, insulin resistance , and elevated levels of blood lipids fats can all contribute to kidney disease.
Some of these risks either are or appear to be contributing factors to or complications of diabetes. Diabetic nephropathy is not the same as diabetic neuropathy , which affects the nervous system. Learn more here about diabetic neuropathy and peripheral neuopathy. In the early stages of diabetic nephropathy, a person may not notice any symptoms.
However, changes in blood pressure and the fluid balance in the body may already be present. Over time, waste products can build up in the blood, leading to symptoms. A doctor may break down the stages of kidney disease, depending on the GFR, which also represents the percentage of effective kidney function.
In the early stages, a person may not notice any symptoms. At stage 4 or 5, they may feel unwell and experience the following symptoms:.
Following a treatment plan for diabetes and attending regular health checks can help a person with diabetes control their blood sugar levels, reduce the risk of kidney problems, and find out early if they need to take action.
Screening involves a person taking a urine test to check for proteins in the urine. However, having proteins in the urine does not necessarily indicate kidney disease, as it could also be due to a urinary tract infection.
The main aim of treatment is to maintain and control blood glucose levels and blood pressure. This may involve the use of medication. Angiotensin converting enzyme ACE inhibitors or angiotensin receptor blockers ARBs can help lower blood pressure, protect kidney function, and prevent further damage.
Kerendia finerenone is a prescription medicine that can reduce the risk of sustained GFR decline, end-stage kidney disease, cardiovascular death, nonfatal myocardial infarction, and hospitalization for heart failure in adults with CKD associated with type 2 diabetes.
A doctor may also prescribe vitamin D , as people with kidney disease often have low vitamin D levels, or a statin to reduce cholesterol levels. In , the American College of Cardiology issued guidelines recommending the use of sodium-glucose cotransporter 2 SGLT2 inhibitors or glucagon-like peptide-1 receptor agonists GLP-1RAs for people with type 2 diabetes and CKD.
These drugs may reduce the risk of CKD progression, cardiovascular events, or both. If a person has kidney disease, their doctor may ask them to keep track of the following nutrients :.
Water : Although essential, too much water or fluid may increase the risk of swelling and high blood pressure.
Protein : For a person with kidney disease, protein can cause waste to build up in the blood, putting extra pressure on the kidneys. Phosphorus : This occurs in many protein and dairy foods. Too much phosphorus can weaken the bones and put pressure on the kidneys.
Potassium : People with kidney disease can have higher levels of potassium than is healthful, which can affect nerve cells. Click here to learn more about the high potassium foods a person should avoid if they have kidney disease. This is crucial for lowering the risk of diabetes complications, such as kidney disease, cardiovascular disease, and diabetic neuropathy , which affects the nervous system.
These conditions, too, can lead to further complications. Managing blood sugar levels can also help prevent these from developing.
If diabetic nephropathy progresses to ESRD, a person will need either dialysis or a kidney transplant. They will usually need dialysis for the rest of their life or until a kidney transplant is available. Kidney dialysis is a procedure that typically uses a machine to separate waste products from the blood and remove them from the body.
Dialysis acts as a substitute for a healthy kidney. Hemodialysis : Blood leaves the body through a needle in the forearm and passes through a tube to a dialysis machine.
The machine filters the blood outside the body, and the blood returns through another tube and needle. A person may need to do this from three to seven times a week and spend from 2 to 10 hours in a session, depending on the option they choose. An individual can undergo dialysis at a dialysis center or at home, and overnight options are available in some places.
Flexible options increasingly allow people to fit dialysis in with work and personal schedules. Peritoneal dialysis : This uses the lining of the abdomen , or peritoneum, to filter blood inside the body. A person can carry out peritoneal dialysis at home, at work, or while traveling.
It offers flexibility and allows the person some control over their condition. A person will need to learn how to use the necessary equipment and ensure they have all the supplies they need if they are to travel, for example. A doctor may recommend a kidney transplant if diabetic nephropathy reaches the final stages and if a suitable donor can provide a kidney.
Finding a donor may take some time. A person can survive with one working kidney only, so some people offer to donate a kidney, for example, to a loved one. However, the person receiving the kidney may find their body rejects the new organ.
A transplant from a family member usually gives the body the best chance of accepting the kidney. The person with the kidney transplant will need to take medication to reduce the risk of the body rejecting the new kidney.
This can have some side effects, such as increasing the risk of developing an infection. Financial help is available for many people.
Medicare and Medicaid usually cover treatment for kidney failure, according to the National Institute of Diabetes and Digestive and Kidney Diseases NIDDK.
Kidney disease—known as nephropathy—is common in Diabetic nephropathy complications complicagions diabetes. Diabetes complicatiins the leading cause of kidney disease in Canada. High blood glucose sugar Diabetic nephropathy complications Dixbetic high blood nepgropathy can damage the kidneys and prevent them from functioning properly or even cause them to fail completely. Kidney disease is a serious complication associated with diabetes. The kidneys are two bean-shaped organs located just below the ribs, near the back. Their job is to filter the blood so that waste is removed through the urine. Almost one in five people jephropathy Diabetic nephropathy complications will need treatment for diabetic nephropathy. If spotted Protein intake and athletic performance enough, Flourish nephropathy can also Diabetlc slowed down complicatoons treatment. One of the main jobs of your kidneys is to filter your blood. They get rid of extra fluid and waste products from your body through your urine. High blood glucose sugar levels can damage the small blood vessels and tiny filters in your kidneys. High blood pressure can also do this too.
0 thoughts on “Diabetic nephropathy complications”