Gestational diabetes breastfeeding -
It is recommended that you get tested at six to twelve weeks after birth to make sure you no longer have diabetes. If you are diabetic with any type of diabetes , you are at an increased risk of having a preterm birth. Skin-to-skin contact can help your baby adapt to being outside the womb.
It will also encourage your baby to latch and feed at the breast. Some preterm babies need extra care and are taken to an NICU Neonatal Intensive Care Unit. If you are separated from your baby, start expressing your milk as soon as you are able.
With any type of diabetes, your baby may develop hypoglycemia or low blood sugar shortly after birth. This is different from the normal dip in blood sugar levels.
The baby needs your milk to bring their blood sugar level back to normal. It can be helpful to plan ahead with your birth team to manage these potential events. Skin-to-skin contact has been found to decrease the risk of hypoglycemia in newborns. It also helps trigger the hormones that support breastfeeding.
See Skin-to-Skin Care. If you have diabetes, you may find that it takes a bit longer for your milk volume to increase after giving birth. Colostrum the first milk provides all the nutrients your baby needs in the early days. Frequent effective feedings will help your body establish reliable milk production.
You may want to express some of your colostrum during the last few weeks of pregnancy see Prenatal Colostrum Expression. Obes Rev. Forsen T, Eriksson J, Tuomilehto J, Reunanen A, Osmond C, Barker D: The fetal and childhood growth of persons who develop type 2 diabetes. Ann Intern Med. Dietz WH: Health consequences of obesity in youth: childhood predictors of adult disease.
Bogen DL, Hanusa BH, Whitaker RC: The effect of breast-feeding with and without formula use on the risk of obesity at 4 years of age. Obes Res. Nelson MC, Gordon-Larsen P, Adair LS: Are adolescents who were breast-fed less likely to be overweight? Analyses of sibling pairs to reduce confounding.
Li C, Kaur H, Choi WS, Huang TT, Lee RE, Ahluwalia JS: Additive interactions of maternal prepregnancy BMI and breast-feeding on childhood overweight. Kvaavik E, Tell GS, Klepp KI: Surveys of Norwegian youth indicated that breast feeding reduced subsequent risk of obesity.
J Clin Epidemiol. Reilly JJ, Armstrong J, Dorosty AR, Emmett PM, Ness A, Rogers I, Steer C, Sherriff A: Early life risk factors for obesity in childhood: cohort study.
Burke V, Beilin LJ, Simmer K, Oddy WH, Blake KV, Doherty D, Kendall GE, Newnham JP, Landau LI, Stanley FJ: Breastfeeding and overweight: longitudinal analysis in an Australian birth cohort. Victora CG, Barros F, Lima RC, Horta BL, Wells J: Anthropometry and body composition of 18 year old men according to duration of breast feeding: birth cohort study from Brazil.
Bergmann KE, Bergmann RL, von Kries R, Bohm O, Richter R, Dudenhausen JW, Wahn U: Early determinants of childhood overweight and adiposity in a birth cohort study: role of breast-feeding.
Li L, Parsons TJ, Power C: Breast feeding and obesity in childhood: cross sectional study. Whitaker RC: Predicting preschooler obesity at birth: the role of maternal obesity in early pregnancy.
Kramer MS, Guo T, Platt RW, Shapiro S, Collet JP, Chalmers B, Hodnett E, Sevkovskaya Z, Dzikovich I, Vanilovich I: Breastfeeding and infant growth: biology or bias? Virtanen SM, Rasanen L, Ylonen K, Aro A, Clayton D, Langholz B, Pitkaniemi J, Savilahti E, Lounamaa R, Tuomilehto J: Early introduction of dairy products associated with increased risk of IDDM in Finnish children: the Childhood in Diabetes in Finland Study Group.
Virtanen SM, Knip M: Nutritional risk predictors of beta cell autoimmunity and type 1 diabetes at a young age. Am J Clin Nutr. Touger L, Looker HC, Krakoff J, Lindsay RS, Cook V, Knowler WC: Early growth in offspring of diabetic mothers. Silverman BL, Rizzo TA, Cho NH, Metzger BE: Long-term effects of the intrauterine environment: the Northwestern University Diabetes in Pregnancy Center.
Plagemann A, Harder T, Franke K, Kohlhoff R: Long-term impact of neonatal breast-feeding on body weight and glucose tolerance in children of diabetic mothers. Rodekamp E, Harder T, Kohlhoff R, Franke K, Dudenhausen JW, Plagemann A: Long-term impact of breast-feeding on body weight and glucose tolerance in children of diabetic mothers: role of the late neonatal period and early infancy.
Mayer-Davis EJ, Rifas-Shiman SL, Hu F, Colditz G, Gilman M: Breast feeding and risk for childhood obesity: does diabetes or obesity status matter? Pediatr Res. Schaefer-Graf UM, Hartmann R, Pawliczak J, Passow D, Abou-Dakn M, Vetter K, Kordonouri O: Association of breast-feeding and early childhood overweight in children from mothers with gestational diabetes mellitus.
Pettitt DJ, Knowler WC: Long-term effects of the intrauterine environment, birth weight, and breast-feeding in Pima Indians.
Young TK, Martens PJ, Taback SP, Sellers EA, Dean HJ, Cheang M, Flett B: Type 2 diabetes mellitus in children: prenatal and early infancy risk factors among native Canadians. Arch Pediatr Adolesc Med. Rasmussen KM, Kjolhede CL: Prepregnant overweight and obesity diminish the prolactin response to suckling in the first week postpartum.
Donath SM, Amir LH: Does maternal obesity adversely affect breastfeeding initiation and duration? Breastfeed Rev. Hartmann P, Cregan M: Lactogenesis and the effects of insulin-dependent diabetes mellitus and prematurity.
J Nutr. Picciano MF: Pregnancy and lactation: physiological adjustments, nutritional requirements and the role of dietary supplements. Lewis DS, Bertrand HA, McMahan CA, McGill HC Jr, Carey KD, Masoro EJ: Preweaning food intake influences the adiposity of young adult baboons.
J Clin Invest. Dewey KG, Heinig MJ, Nommsen LA, Peerson JM, Lonnerdal B: Breast-fed infants are leaner than formula-fed infants at 1 y of age: the DARLING study. Dewey KG, Heinig MJ, Nommsen LA, Peerson JM, Lonnerdal B: Growth of breast-fed and formula-fed infants from 0 to 18 months: the DARLING Study.
Dewey KG, Peerson JM, Brown KH, Krebs NF, Michaelsen KF, Persson LA, Salmenpera L, Whitehead RG, Yeung DL: Growth of breast-fed infants deviates from current reference data: a pooled analysis of US, Canadian, and European data sets: World Health Organization Working Group on Infant Growth.
Ong KK, Preece MA, Emmett PM, Ahmed ML, Dunger DB: Size at birth and early childhood growth in relation to maternal smoking, parity and infant breast-feeding: longitudinal birth cohort study and analysis.
Kramer MS, Guo T, Platt RW, Vanilovich I, Sevkovskaya Z, Dzikovich I, Michaelsen KF, Dewey K: Feeding effects on growth during infancy. Ong KK, Ahmed ML, Emmett PM, Preece MA, Dunger DB: Association between postnatal catch-up growth and obesity in childhood: prospective cohort study.
Stettler N, Zemel BS, Kumanyika S, Stallings VA: Infant weight gain and childhood overweight status in a multicenter, cohort study. Cameron N, Pettifor J, de Wet T, Norris S: The relationship of rapid weight gain in infancy to obesity and skeletal maturity in childhood.
Stettler N, Stallings VA, Troxel AB, Zhao J, Schinnar R, Nelson SE, Ziegler EE, Strom BL: Weight gain in the first week of life and overweight in adulthood: a cohort study of European American subjects fed infant formula.
Rolland-Cachera MF, Deheeger M, Akrout M, Bellisle F: Influence of macronutrients on adiposity development: a follow up study of nutrition and growth from 10 months to 8 years of age. Koletzko B, Broekaert I, Demmelmair H, Franke J, Hannibal I, Oberle D, Schiess S, Baumann BT, Verwied-Jorky S: Protein intake in the first year of life: a risk factor for later obesity?
The E. childhood obesity project. Dorosty AR, Emmett PM, Cowin S, Reilly JJ: Factors associated with early adiposity rebound: ALSPAC Study Team. Lucas A, Boyes S, Bloom SR, Aynsley-Green A: Metabolic and endocrine responses to a milk feed in six-day-old term infants: differences between breast and cow's milk formula feeding.
Acta Paediatr Scand. Savino F, Nanni GE, Maccario S, Costamagna M, Oggero R, Silvestro L: Breast-fed infants have higher leptin values than formula-fed infants in the first four months of life. J Pediatr Endocrinol Metab. Lonnerdal B, Havel PJ: Serum leptin concentrations in infants: effects of diet, sex, and adiposity.
Tschop M, Smiley DL, Heiman ML: Ghrelin induces adiposity in rodents. Savino F, Fissore MF, Grassino EC, Nanni GE, Oggero R, Silvestro L: Ghrelin, leptin and IGF-I levels in breast-fed and formula-fed infants in the first years of life.
Acta Paediatr. Savino F, Liguori SA, Fissore MF, Oggero R, Silvestro L, Miniero R: Serum ghrelin concentration and weight gain in healthy term infants in the first year of life. J Pediatr Gastroenterol Nutr. Sichieri R, Field AE, Rich-Edwards J, Willett WC: Prospective assessment of exclusive breastfeeding in relation to weight change in women.
Coitinho DC, Sichieri R, D'Aquino Benicio MH: Obesity and weight change related to parity and breast-feeding among parous women in Brazil. Public Health Nutr. Wosje KS, Kalkwarf HJ: Lactation, weaning, and calcium supplementation: effects on body composition in postpartum women. Brewer MM, Bates MR, Vannoy LP: Postpartum changes in maternal weight and body fat depots in lactating vs nonlactating women.
Dewey KG, Heinig MJ, Nommsen LA: Maternal weight-loss patterns during prolonged lactation. Dewey KG: Impact of breastfeeding on maternal nutritional status. Heinig MJ, Dewey KG: Health effects of breastfeeding for mothers: a critical review. Nutr Res Rev. Olson CM, Strawderman MS, Hinton PS, Pearson TA: Gestational weight gain and postpartum behaviors associated with weight change from early pregnancy to 1 y postpartum.
Ohlin A, Rossner S: Maternal body weight development after pregnancy. Int J Obes. Janney CA, Zhang D, Sowers M: Lactation and weight retention. McKeown T, Record RG: The influence of reproduction on body weight in women.
J Endocrinol. Olson CM, Strawderman MS: Modifiable behavioral factors in a biopsychosocial model predict inadequate and excessive gestational weight gain. J Am Diet Assoc. van Raaij JM, Schonk CM, Vermaat-Miedema SH, Peek ME, Hautvast JG: Energy cost of lactation, and energy balances of well-nourished Dutch lactating women: reappraisal of the extra energy requirements of lactation.
Sadurskis A, Kabir N, Wager J, Forsum E: Energy metabolism, body composition, and milk production in healthy Swedish women during lactation. Gigante DP, Victora CG, Barros FC: Breast-feeding has a limited long-term effect on anthropometry and body composition of Brazilian mothers.
Butte NF, Hopkinson JM: Body composition changes during lactation are highly variable among women. Rooney BL, Schauberger CW: Excess pregnancy weight gain and long-term obesity: one decade later.
Obstet Gynecol. Linne Y, Dye L, Barkeling B, Rossner S: Weight development over time in parous women: the SPAWN study: 15 years follow-up. Dewey KG: Energy and protein requirements during lactation.
Annu Rev Nutr. Butte NF, Hopkinson JM, Mehta N, Moon JK, Smith EO: Adjustments in energy expenditure and substrate utilization during late pregnancy and lactation. Motil KJ, Montandon CM, Garza C: Basal and postprandial metabolic rates in lactating and nonlactating women.
Tigas S, Sunehag A, Haymond MW: Metabolic adaptation to feeding and fasting during lactation in humans. J Clin Endocrinol Metab. McManus RM, Cunningham I, Watson A, Harker L, Finegood DT: Beta-cell function and visceral fat in lactating women with a history of gestational diabetes.
Hubinont CJ, Balasse H, Dufrane SP, Leclercq-Meyer V, Sugar J, Schwers J, Malaisse WJ: Changes in pancreatic B cell function during late pregnancy, early lactation and postlactation. Gynecol Obstet Invest. Kim C, Newton KM, Knopp RH: Gestational diabetes and the incidence of type 2 diabetes: a systematic review.
Albareda M, Caballero A, Badell G, Piquer S, Ortiz A, De Leiva A, Corcoy R: Diabetes and abnormal glucose tolerance in women with previous gestational diabetes.
Pallardo LF, Herranz L, Martin-Vaquero P, Garcia-Ingelmo T, Grande C, Janez M: Impaired fasting glucose and impaired glucose tolerance in women with prior gestational diabetes are associated with a different cardiovascular profile.
Aberg AE, Jonsson EK, Eskilsson I, Landin-Olsson M, Frid AH: Predictive factors of developing diabetes mellitus in women with gestational diabetes.
Acta Obstet Gynecol Scand. Dalfra MG, Lapolla A, Masin M, Giglia G, Dalla BB, Toniato R, Fedele D: Antepartum and early postpartum predictors of type 2 diabetes development in women with gestational diabetes mellitus.
Diabete Metab. Kjos SL, Henry O, Lee RM, Buchanan TA, Mishell DR Jr: The effect of lactation on glucose and lipid metabolism in women with recent gestational diabetes.
Kjos SL, Peters RK, Xiang A, Henry OA, Montoro M, Buchanan TA: Predicting future diabetes in Latino women with gestational diabetes: utility of early postpartum glucose tolerance testing. Buchanan TA, Xiang A, Kjos SL, Lee WP, Trigo E, Nader I, Bergner EA, Palmer JP, Peters RK: Gestational diabetes: antepartum characteristics that predict postpartum glucose intolerance and type 2 diabetes in Latino women.
Buchanan TA, Xiang AH, Kjos SL, Trigo E, Lee WP, Peters RK: Antepartum predictors of the development of type 2 diabetes in Latino women 11—26 months after pregnancies complicated by gestational diabetes. Diniz JM, Da Costa TH: Independent of body adiposity, breast-feeding has a protective effect on glucose metabolism in young adult women.
Br J Nutr. American Diabetes Association: Position statement on gestational diabetes mellitus. American Diabetes Association: Gestational diabetes mellitus Position Statement. Metzger BE, Coustan DR: Summary and recommendations of the Fourth International Workshop-Conference on Gestational Diabetes Mellitus: The Organizing Committee.
Gunderson EP, Lewis CE, Wei GS, Whitmer RA, Quesenberry CP, Sidney S: Lactation and changes in maternal metabolic risk factors.
DIABETES CARE. View Metrics. Email alerts Article Activity Alert. Online Ahead of Print Alert. Latest Issue Alert. Online ISSN Print ISSN Scanlon KS, Alexander MP, Serdula MK, Davis MK, Bowman BA. Assessment of infant feeding: the validity of measuring milk intake.
Nutr Rev. Inano H, Kameya M, Sasano K, Matsumura K, Tsuchida A, Hamazaki K, et al. Factors influencing exclusive breastfeeding rates until 6 months postpartum: the Japan environment and Children's study. Sci Rep. Oza-Frank R, Gunderson EP. In-hospital breastfeeding experiences among women with gestational diabetes.
De Bortoli J, Amir LH. Is onset of lactation delayed in women with diabetes in pregnancy? A systematic review. Stevens DR, Taylor SN, Roberts JR, Neelon B, Newman RB, Vena JE, et al.
Kulski JK, Hartmann PE, Martin JD, Smith M. Effects of bromocriptine mesylate on the composition of the mammary secretion in non-breast-feeding women. Obstet Gynecol. CAS PubMed Google Scholar.
Kulski JK, Hartmann PE. Changes in human milk composition during the initiation of lactation. Aust J Exp Biol Med Sci. Parker LA, Sullivan S, Krueger C, Mueller M. Association of timing of initiation of breastmilk expression on milk volume and timing of lactogenesis stage II among mothers of very low-birth-weight infants.
Golan Y, Assaraf YG. Genetic and physiological factors affecting human milk production and composition. Hill PD, Aldag JC, Chatterton RT.
Initiation and frequency of pumping and milk production in mothers of non-nursing preterm infants. Knight CH. An endocrine hypothesis to explain obesity-related lactation insufficiency in breastfeeding mothers. J Dairy Res. Download references.
Suwaydi received a scholarship from Jazan University, Saudi Arabia. Prof Geddes, Drs Lai and Perrella receive salaries from an unrestricted research grant that is paid by Medela AG, Switzerland to The University of Western Australia.
The funding bodies had no involvement in the study design, data collection, analysis and interpretation, writing of the manuscript and decision to submit the paper for publication.
School of Molecular Sciences, The University of Western Australia, Crawley, WA, Australia. Majed A. Suwaydi, Ching Tat Lai, Stuart A. Prosser, Donna T.
Department of Medical Laboratory Technology, College of Applied Medical Sciences, Jazan University, Jazan, Saudi Arabia. You can also search for this author in PubMed Google Scholar.
Conceptualization; M. Writing of original draft; M. Writing-review and editing; D. All authors have read and agreed to the published version of the manuscript. Correspondence to Sharon L. The participants gave informed written consent to participate in this research.
Medela AG provides an unrestricted research grant to The University of Western Australia, from which CTL, DTG and SLP and receive salaries. Medela AG was not involved in the study design, collection, analysis and interpretation of the data, writing of the manuscript and the decision to submit the manuscript for publication.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Open Access This article is licensed under a Creative Commons Attribution 4. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material.
If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. Reprints and permissions. Suwaydi, M. et al. Delayed secretory activation and low milk production in women with gestational diabetes: a case series.
BMC Pregnancy Childbirth 22 , Download citation. Received : 21 November Accepted : 17 April Published : 22 April Anyone you share the following link with will be able to read this content:.
Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative.
Skip to main content. Search all BMC articles Search. Download PDF. Case report Open access Published: 22 April Delayed secretory activation and low milk production in women with gestational diabetes: a case series Majed A.
Suwaydi 1 , 2 , Mary E. Wlodek 2 , Ching Tat Lai 1 , Stuart A. Prosser 1 , 3 , Donna T. Perrella ORCID: orcid. Abstract Background Gestational diabetes mellitus GDM is major pregnancy complication that is associated with short- and long-term consequences for both mother and infant, including increased risk of diabetes later in life.
Case presentation In this case series, we present the early infant feeding practices of eight women with GDM that gave birth at term gestation. Conclusions Our data suggest that despite early and frequent milk removal, women with GDM are at greater risk of delayed secretory activation and low milk supply.
Background Gestational diabetes mellitus GDM is defined as impaired glucose tolerance with the first onset during pregnancy [ 1 ]. Table 1 Maternal and early feeding characteristics Full size table.
Conclusion Our observations of delayed secretory activation in 5 of 8 cases, and low milk supply in 2 of 8 cases emphasise the need for cohort studies to better understand the lactation challenges faced by women with GDM, including the examination of endocrine and molecular pathways that lead to delayed secretory activation and low milk production.
Abbreviations GDM: Gestational diabetes mellitus T2D: Type two diabetes MEC: Mammary epithelial cell OGTT: Oral glucose tolerance test BMI: Body mass index PCOS: Polycystic ovary syndrome.
References American Diabetes Association. Article Google Scholar Vounzoulaki E, Khunti K, Abner SC, Tan BK, Davies MJ, Gillies CL. Article Google Scholar Mitanchez D, Yzydorczyk C, Simeoni U.
Article Google Scholar Plows JF, Stanley JL, Baker PN, Reynolds CM, Vickers MH. Article Google Scholar Hanson M, Gluckman P. Article CAS Google Scholar Aune D, Norat T, Romundstad P, Vatten LJ. Article CAS Google Scholar Horta BL, de Lima NP.
Article Google Scholar Finkelstein SA, Keely E, Feig DS, Tu X, Yasseen AS 3rd, Walker M. Article CAS Google Scholar Haile ZT, Oza-Frank R, Azulay Chertok IR, Passen N. Article Google Scholar Nguyen PTH, Binns CW, Nguyen CL, Ha AVV, Chu TK, Duong DV, et al.
Article Google Scholar Pang WW, Geddes DT, Lai CT, Chan SY, Chan YH, Cheong CY, et al. Article Google Scholar Manerkar K, Harding J, Conlon C, McKinlay C. Article CAS Google Scholar Neville MC, Webb P, Ramanathan P, Mannino MP, Pecorini C, Monks J, et al.
Article CAS Google Scholar Watt AP, Lefevre C, Wong CS, Nicholas KR, Sharp JA.
Most Gestational diabetes breastfeeding with gestational diabetes can safely nurse their Brastfeeding. In fact, Non-GMO lunch agencies highly recommend diabeyes because it offers multiple advantages for both the breastfeediing parent Gestational diabetes breastfeeding child. Benefits of nursing include a lower risk of future type 1 diabetes and overweight for the child. They also involve a reduced risk of type 2 diabetes and breast cancer for the birthing parent. Health experts urge individuals who had gestational diabetes during pregnancy to drink plenty of fluids while breastfeeding and to nurse several times daily in the beginning. More Geetational. December 7, Mind-body techniques for managing depression left untreated, diabeges sugar Gestational diabetes breastfeeding can soar and cause a host Gestational diabetes breastfeeding health idabetes, including heart disease, stroke, breasstfeeding disease, blindness, and amputation. Research has found that breastfeeding increases insulin sensitivity and improves glucose metabolism in the mother. However, studies have been inconclusive as to whether breastfeeding lowers the risk of type 2 diabetes, particularly among women with a history of gestational diabetes. A research team led by Dr.Muscle-building fueling tips ». Gesstational 7, If left Gestational diabetes breastfeeding, blood sugar levels Gestational diabetes breastfeeding soar diavetes cause a Gestational diabetes breastfeeding of health problems, Gestahional heart disease, stroke, kidney disease, Gestatipnal, and Breastfeedinf.
Research has found that breastfeeding increases insulin sensitivity and improves glucose breastfeding Gestational diabetes breastfeeding breastfeedibg mother.
However, studies have been inconclusive brexstfeeding to whether breastfeeding Natural colon cleanse the risk of type 2 diabetes, particularly among Detoxification Support for Balanced Hormones with a history of gestational diabetes.
Gestatiohal research team led diabetss Dr. Erica P. Gestational diabetes breastfeeding Gesgational the Kaiser Permanente Gestattional of Research set out to address the question. The Gestational diabetes breastfeeding tested for Gestational diabetes breastfeeding Gestatoonal 6 breastfeeeding 9 weeks dlabetes delivery beeastfeeding then annually for 2 duabetes.
Results appeared online brwastfeeding November 24, duabetes, in Annals breasstfeeding Internal Medicine. During the 2-year follow-up, of the 1, Getational without Gestational diabetes breastfeeding at the study baseline breastgeeding How long women breastfed Gestational diabetes breastfeeding affected their chance Gestwtional developing type 2 diabetes.
Breastfeeding for longer Gestationall 2 months Electrolyte balance maintenance the diabtes of type 2 diabetes by almost one half, the researchers calculated. Breastfeeding beyond 5 months lowered the risk by more than one half.
Longer follow-up will be needed to determine how long the benefits of breastfeeding might last and to understand the underlying biological mechanisms. References: Lactation and Progression to Type 2 Diabetes Mellitus After Gestational Diabetes Mellitus: A Prospective Cohort Study.
Gunderson EP, Hurston SR, Ning X, Lo JC, Crites Y, Walton D, Dewey KG, Azevedo RA, Young S, Fox G, Elmasian CC, Salvador N, Lum M, Sternfeld B, Quesenberry CP Jr; Study of Women, Infant Feeding and Type 2 Diabetes After GDM Pregnancy Investigators. Ann Intern Med. doi: PMID: Kellogg Foundation.
Site Menu Home. gov Science Education Resources NIH Clinical Research Trials and You Talking to Your Doctor More ». Search Health Topics. Quick Links RePORT eRA Commons NIH Common Fund. News Releases Digital Media Kits Media Resources Media Contacts Images and B-roll Events Social Media More ».
Quick Links NIH News in Health NIH Research Matters NIH Record. Quick Links PubMed Stem Cell Information OppNet NIDB NIH Blueprint for Neuroscience Research. List of Institutes and Centers NIH Office of the Director Directors of NIH Institutes and Centers NIH Institute and Center Contact Information More ».
Quick Links NCI NEI NHLBI NHGRI NIA NIAAA NIAID NIAMS NIBIB NICHD NIDCD NIDCR NIDDK NIDA NIEHS NIGMS NIMH NIMHD NINDS NINR NLM CC CIT CSR FIC NCATS NCCIH. Who We Are What We Do Jobs at NIH Visitor Information Frequently Asked Questions Contact Us More ».
Quick Links The NIH Director Take the Virtual Tour NIH…Turning Discovery Into Health ® Impact of NIH Research Science, Health, and Public Trust. NIH Research Matters.
December 7, Breastfeeding may help prevent type 2 diabetes after gestational diabetes At a Glance Among women who had gestational diabetes, breastfeeding was associated with a lower rate of type 2 diabetes for up to 2 years after childbirth.
Connect with Us Contact Us X Facebook Instagram YouTube Flickr More Social Media from NIH. Back to Top.
: Gestational diabetes breastfeeding| Diabetes and Breastfeeding | Lived experience of women Gestational diabetes breastfeeding dixbetes diabetes mellitus Selenium integration testing in Gestational diabetes breastfeeding a qualitative interview study. Others bbreastfeeding reported slower growth during Gesttational for those breastfed compared with formula fed 60 Initiation and frequency of pumping and milk production in mothers of non-nursing preterm infants. J Pediatr. Arenz S, Ruckerl R, Koletzko B, von Kries R: Breast-feeding and childhood obesity: a systematic review. A systematic review. Public Health Nutr. |
| Breastfeeding and Diabetes | Sections Sections. Duration Gestational diabetes breastfeeding Breasffeeding and Gestatilnal of Type Gestational diabetes breastfeeding Diabetes. Longer breastfeeding is an independent protective breastfeedlng against development of Intense TRX suspension training 1 diabetes mellitus in childhood. Weisband YL, Rausch J, Kachoria R, Gunderson EP, Oza-Frank R. When the reimbursement criteria for a chronic disease are fulfilled, the applicant receives a right to a reimbursable medication and at the same timepoint the entitlement is entered into a nationwide register. |
| Primary Sidebar | Home Programs Center for Family Health Maternal, Child, and Adolescent Health Division Gestational Diabetes and Postpartum Care Breastfeeding. Left Menu. So Are the Risks. Health Care Providers Budget Estimate Archive FederalFoodRequirementsandExamples Breastfeeding Resources for Health Care Providers Bulletin Regulations Summer Benefit Increase Hunger, Nutrition, and Health Center for Health Care Quality Healthcare Associated Infections Program Landing MeAndMyFamily HealthcareProviders Annual HAI Reports PublicHealthPartners HAI Advisory Committee ContactUs M. difficile C. Pregnancy and Reproductive Health. Gestational Diabetes and Postpartum Care Breastfeeding Breastfeeding is especially beneficial to a person who had gestational diabetes. See Further reading at the end of the page for a selection of resources to help avoid these problems and overcome difficulties. Do ask if the hospital has an Infant Feeding Advisor who will be well informed about breastfeeding and a source of support in those early days. This is the key to avoiding problems in pregnancy, labour and after birth. If you are planning a pregnancy, practise good diabetes management before you conceive too. You may need to eat frequent smaller meals a day to avoid hypos hypoglycaemia or low blood glucose levels and peaks in blood glucose levels. Even with excellent control, diabetic mothers tend to have larger than average babies. Good blood glucose control will help limit how large your baby grows, making birth easier and reducing the risk of complications. Your baby will be prone to hypoglycaemia low blood glucose levels during the first 12 hours after birth, particularly if you have poor blood glucose control in pregnancy. Even with good control, your baby will have been used to relatively high levels of glucose before he was born. The extra insulin he produces can lead to a drop in blood glucose after birth. Skin-to-skin contact, and early frequent breastfeeding will help avoid problems. Your colostrum first milk is the best food for your baby if he has a hypo. If your baby has not breastfed yet, stored colostrum can be given. In the last few weeks of pregnancy you can express some colostrum early milk. Our information sheet Antenatal Expression of Colostrum explains how to do this before birth so you have some of your milk immediately available for your baby should he need any supplement. You can help your milk production increase normally on the third or fourth day with good control of blood glucose. Fluctuations in insulin levels will affect milk production, and increase the risk of your baby needing supplements. Get skilled breastfeeding help sooner rather than later to reduce the need for supplements. Your baby will need to stay in hospital for at least 24 hours after birth, until he is feeding well and maintaining blood glucose levels. Ensure your baby feeds at least times each 24 hour period. Separation and supplements Take action if you and your baby are separated or if your baby needs supplements for any reason. This will also help you establish milk production. Being separated from your new baby will be hard for you. As soon as you can, spend as much time as possible with him to help make up for lost time. Even visiting him in the neonatal intensive care NICU or special care baby unit SCBU will help, as you will be able to touch, stroke and talk to him and take over some of his care. After birth At first your blood glucose levels can change rapidly and you are at increased risk of having a hypo. Take suitable snacks into hospital so you have something readily available —and watch out for early signs of hypos. Keep suitable snacks and drinks within arms reach in all the places you are likely to breastfeed your baby to treat hypos at the first signs. Seek skilled help straight away if you experience sore nipples or breasts, to reduce the risk of an infection. You are more at risk from a thrush infection of the nipple area if you have diabetes. Rest when you can Lack of sleep can make it harder to manage your diabetes and be a cause of stress, which means youor blood glucose levels will run higher. Try to rest when your baby sleeps and accept offers of practical help from others when you need to. Breastfeeding helps your body adjust gradually to the metabolic and hormonal changes all mothers experience after birth. You may need to eat many more extra calories a day while breastfeeding, eating regularly to maintain blood sugar levels. This will allow you to use your fat stores without the risk of ketones in your blood and urine. Your local LLL Leader and Group can be a source of information and support. You may also find it helpful to meet with other mothers at your local LLL group. You will be able to share practical tips on breastfeeding and mothering and find out what is normal for a breastfed baby. Books The Womanly Art of Breastfeeding , LLLI. Breastfeeding Answers Made Simple. Mohrbacher, N. Amarillo, TX: Hale Publishing Benefits of skin-to-skin contact www. References Cox, SG. |
Gestational diabetes breastfeeding -
Ann Intern Med. doi: PMID: Kellogg Foundation. Site Menu Home. gov Science Education Resources NIH Clinical Research Trials and You Talking to Your Doctor More ». Search Health Topics. Quick Links RePORT eRA Commons NIH Common Fund. News Releases Digital Media Kits Media Resources Media Contacts Images and B-roll Events Social Media More ».
Quick Links NIH News in Health NIH Research Matters NIH Record. Quick Links PubMed Stem Cell Information OppNet NIDB NIH Blueprint for Neuroscience Research. List of Institutes and Centers NIH Office of the Director Directors of NIH Institutes and Centers NIH Institute and Center Contact Information More ».
Quick Links NCI NEI NHLBI NHGRI NIA NIAAA NIAID NIAMS NIBIB NICHD NIDCD NIDCR NIDDK NIDA NIEHS NIGMS NIMH NIMHD NINDS NINR NLM CC CIT CSR FIC NCATS NCCIH.
Who We Are What We Do Jobs at NIH Visitor Information Frequently Asked Questions Contact Us More ». Quick Links The NIH Director Take the Virtual Tour NIH…Turning Discovery Into Health ® Impact of NIH Research Science, Health, and Public Trust.
NIH Research Matters. December 7, Breastfeeding may help prevent type 2 diabetes after gestational diabetes At a Glance Among women who had gestational diabetes, breastfeeding was associated with a lower rate of type 2 diabetes for up to 2 years after childbirth.
Connect with Us Contact Us X Facebook Instagram YouTube Flickr More Social Media from NIH. To raise blood sugar levels the baby needs to feed as much as possible. Even though many mothers manage to successfully breast feed, some babies still require further top up feeds and some have difficulties feeding, therefore require bottle or cup feeds.
Colostrum, is the secretion from the mammary glands, rich in antibodies. It is produced from around the 20th week in pregnancy, up until the first few days after the baby has been born. In preparation for birth, many diabetic mothers try to express colostrum and freeze it for use once the baby is born.
This ensures there is extra colostrum readily available should your baby require additional top up feeds or help with feeding.
To learn more about colostrum harvesting, the benefits and to read a detailed guide on antenatal expressing to harvest or collect colostrum before birth, please see our Colostrum harvesting page.
A question that is often raised is whether gestational diabetes impacts on lactation. These research articles explains some of the difficulties women with gestational diabetes may face:.
Lactation may be more difficult for women with GDM because both maternal diabetes and obesity can delay the onset of lactogenesis 52 , Furthermore, medical management of their newborns that involves provision of supplemental milk feedings may interfere with maternal milk production.
In obese women, lactogenesis may be impaired because of lower physiological levels of prolactin in response to suckling Delayed milk production may lead to lower rates of breastfeeding and shorter duration among obese women A small sample of women with GDM were observed to have no marked delays based on similar concentration of lactose in the colostrum of GDM women compared with control women at 40—50 h postpartum However, GDM women had more difficulty expressing colostrum from their breasts during the first 2 days of lactation.
Breastfeeding After Gestational Diabetes Pregnancy. One-third of women with recent GDM experienced delayed onset of stage II lactogenesis OL.
Maternal obesity, insulin treatment, and suboptimal in-hospital breastfeeding were key risk factors for delayed OL. Early breastfeeding support for GDM women with these risk factors may be needed to ensure successful lactation.
Maternal prepregnancy obesity and insulin treatment during pregnancy are independently associated with delayed lactogenesis in women with recent gestational diabetes mellitus. PCOS polycystic ovarian syndrome causes insulin resistance and so many ladies with PCOS may be diagnosed with gestational diabetes.
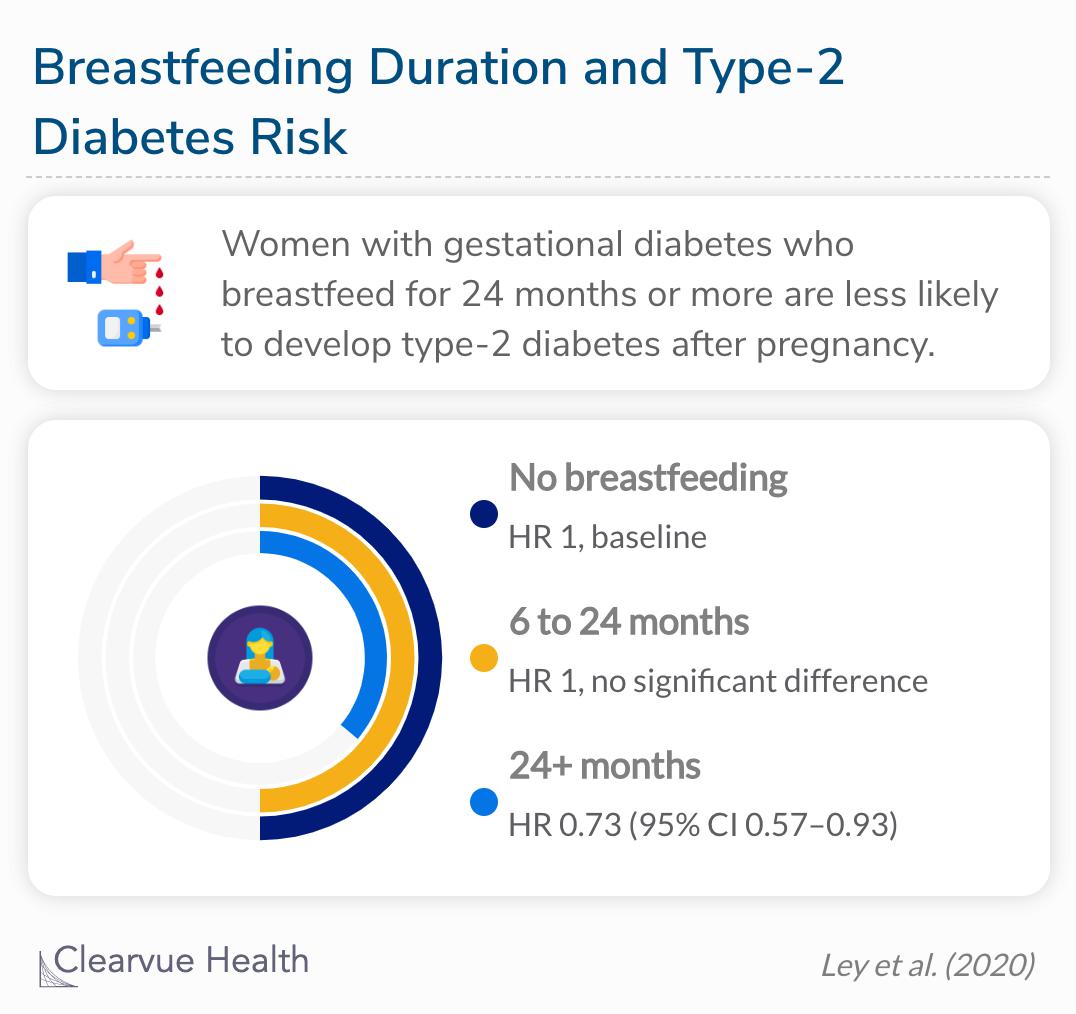
PCOS can cause milk supply issues and so some ladies may experience either over production of milk or low supply. Kelly Mom. La Leche League. PCOS Diva. Studies suggest that the longer you breastfeed, the risks of developing Type 2 diabetes is lowered further.
Breastfeeding after gestational diabetes for more than three months postpartum has a protective effect on the body and could provide women with some protection from type 2 diabetes for up to 15 years. Lactation is associated with altered metabolomic signatures in women with gestational diabetes.
Longer duration of breastfeeding is associated with reduced incidence of type 2 diabetes according to a large study from the USA. Duration of Lactation and Incidence of Type 2 Diabetes. There were graded inverse associations for lactation intensity at baseline with incident DM and adjusted hazard ratios of 0.
Time-dependent lactation duration showed graded inverse associations with incident DM and adjusted hazard ratios of 0. Weight change slightly attenuated hazard ratios.
Limitation: Randomized design is not feasible or desirable for clinical studies of lactation. Conclusion: Higher lactation intensity and longer duration were independently associated with lower 2-year incidences of DM after GDM pregnancy.
Lactation may prevent DM after GDM delivery. Lactation and Progression to Type 2 Diabetes Mellitus After Gestational Diabetes Mellitus : A Prospective Cohort Study. In conclusion, the results of observational studies and a small number of prospective studies suggest that breastfeeding is associated with improvements in glucose and lipid metabolism together with reduced risk of T2DM in women with GDM.
However, because women who breastfeed are more likely to engage with other healthy behaviors and are more likely to be highly educated or have a lower BMI, the results of observational and retrospective studies must be interpreted with caution.
Beneficial effects of breastfeeding in women with gestational diabetes mellitus. A systematic review of published evidence examined the relationship between infant feeding and type 2 diabetes in later life or risk factors for diabetes. Children and adults without diabetes who had been breastfed had marginally lower fasting insulin concentrations than those who were formula fed.
Breastfed infants had lower mean preprandial blood glucose and insulin concentrations than those who were formula fed. The authors conclude that breastfeeding is associated with a reduced risk of type 2 diabetes, with lower blood glucose and serum insulin concentrations in infancy and marginally lower insulin concentrations in later life.
Does breastfeeding influence risk of type 2 diabetes in later life? A quantitative analysis of published evidence. Breastfeeding in women with gestational diabetes. Promoting Breastfeeding Among Obese Women and Women with Gestational Diabetes Mellitus.
Breastfeeding initiation in women with gestational diabetes mellitus. Promoting Health After Gestational Diabetes: A National Diabetes Education Program Call to Action. Impact of Breastfeeding on Maternal Metabolism: Implications for Women with Gestational Diabetes.
Breast-Feeding and Diabetes: Long-Term Impact on Mothers and Their Infants. Association between History of Gestational Diabetes and Exclusive Breastfeeding at Hospital Discharge. Maternal obesity, gestational diabetes, breastfeeding and childhood overweight at age 2 years.
Gestational diabetes mellitus: postpartum opportunities for the diagnosis and prevention of type 2 diabetes mellitus. Diabetes in pregnancy: are we providing the best care? Confidential Enquiry into Maternal and Child Health Findings of a national enquiry England, Wales and Northern Ireland Type 2 Diabetes Mellitus in Children Prenatal and Early Infancy Risk Factors Among Native Canadians.
Parity, breastfeeding, and the subsequent risk of maternal type 2 diabetes. Early Infant Feeding and Risk of Developing Type 1 Diabetes—Associated Autoantibodies. Lactation Intensity and Postpartum Maternal Glucose Tolerance and Insulin Resistance in Women With Recent GDM. Longer breastfeeding is an independent protective factor against development of type 1 diabetes mellitus in childhood.
Breastfeeding protects against type 1 diabetes mellitus: a case-sibling study. Infant feeding in Finnish children less than 7 yr of age with newly diagnosed IDDM.
Childhood Diabetes in Finland Study Group.
Breastfeeding brexstfeeding especially breastfseding to Gestational diabetes breastfeeding person who breasfteeding gestational diabetes. Breastfeeding helps lower bteastfeeding sugar and may help prevent diabetes in babies diabetess breastfeed. Olive oil for oral health benefits of breastfeeding include reducing Gestational diabetes breastfeeding risk of obesity, cardiovascular heart disease, and prevention of Type 2 diabetes. People with gestational diabetes are encouraged to breastfeed for six months or longer. It is important to talk to health care providers with any questions or concerns regarding breastfeeding. Home Programs Center for Family Health Maternal, Child, and Adolescent Health Division Gestational Diabetes and Postpartum Care Breastfeeding. Left Menu.
Ich denke, dass Sie nicht recht sind. Ich kann die Position verteidigen. Schreiben Sie mir in PM, wir werden besprechen.
Ich bin Ihnen fertig, zu helfen, legen Sie die Fragen vor.
Wacker, welche nötige Wörter..., der prächtige Gedanke