
Pancreatic pseudocyst -
Case 4 Case 4. Case 5 Case 5. Case 6: causing gastric outlet obstruction Case 6: causing gastric outlet obstruction. Case 7 Case 7. Case 8: MRI Case 8: MRI. Case 9: as a fullness on x-ray Case 9: as a fullness on x-ray.
Case 10 Case Case 11 Case Case 12 Case Case 13 Case Case encasing the pancreas Case encasing the pancreas. Case 15 Case Case 16 Case Case 17 Case Case 18 Case Case 19 Case Case 20 Case Case 21 Case Case chronic pancreatitis Case chronic pancreatitis.
Case Chronic pancreatitis with intrahepatic and intrasplenic pseudocysts Case Chronic pancreatitis with intrahepatic and intrasplenic pseudocysts. Case 25 Case Acute peripancreatic fluid collections Acute peripancreatic fluid collections.
Mucinous cystadenoma of the pancreas Mucinous cystadenoma of the pancreas. Pancreatic walled-off necrotic collection Pancreatic walled-off necrotic collection. Pancreatic walled-off necrosis Pancreatic walled-off necrosis. Simple pancreatic cyst Simple pancreatic cyst. Loading more images Close Please Note: You can also scroll through stacks with your mouse wheel or the keyboard arrow keys.
Loading Stack - 0 images remaining. By Section: Anatomy Approach Artificial Intelligence Classifications Gamuts Imaging Technology Interventional Radiology Mnemonics Pathology Radiography Signs Staging Syndromes. By System:. In a study on patients, Heider et al 34 reported a different result; it was concluded that unselected patients treated with PCD demonstrated a higher failure rate, higher mortality and morbidity rate and required more long-term hospitalization compared with those treated by surgery.
Thus, PCD should only be recommended for patients who are not eligible for surgical treatment. Pancreatic pseudocyst have been treated using surgery for over a decade and this is still frequently used as a treatment option.
The surgical treatment of pancreatic pseudocyst entails internal drainage into the stomach, duodenum and jejunum, external drainage and resection. Jedlicka 38 performed the first pseudocystgastrostomy in However, reoperation is not uncommon in SD, particularly for patients with chronic pancreatitis and persistent alcohol abuse.
The majority of modern studies have compared SD with a minimally invasive technique, such as ED; most concluded that SD and ED shared similar success rates, complications and re-intervention rates; however, treatment with ED was associated with lower costs and shorter hospital stays, making ED superior to SD 40 , However, there remains a clear preference for the open surgical treatment of pseudocysts.
For instance, a pseudocyst located in the pancreatic tail far away from the gastrointestinal lumen meant that ED was not a good treatment choice and due to its close proximity to the spleen, there was an increased risk of injury and hemorrhage, even with the PCD technique; thus, under those circumstances, SD was the best choice for treatment.
Certain other indications for preferential surgical treatment are i contraindication or failure of endoscopic or radiological methods; ii complex main pancreatic duct stricture; iii complex pathology such as an inflammatory mass in the pancreatic head; iv main bile duct stricture caused by pseudocyst compression; v venous occlusive disease; vi multiple pseudocysts; vii pseudocyst of the pancreatic tail; viii hemorrhage not adequately controlled by angiographic embolization; and ix suspicion of neoplastic cysts Laparoscopic cystogastrostomy has become another promising technique for minimally invasive treatment in addition to ED.
The laparoscopic procedure may be accomplished using an anterior approach or a posterior approach; the use of these two techniques is based on the experience of the operator In the anterior approach, a 4-cm anterior gastrostomy is made with a harmonic scalpel to access the gastric mucosa, and a laparoscopic ultrasound probe is used to identify the location of the pseudocyst behind the gastric mucosa.
After certifying the location, a harmonic scalpel is used to create a cystogastrostomy opening to drain the pseudocyst, and the anterior gastrostomy is then closed.
In the posterior approach, a harmonic scalpel is used to divide the gastrocolic ligament, facilitating the entry to the lesser sac and access to the pancreas.
A laparoscopic ultrasound probe is then used to locate the pseudocyst and a cystogastrostomy is then made with a stapler between the cyst and posterior gastric wall.
This posterior approach is more difficult than the anterior approach; however, the visualization of the pseudocyst is clearer and the surgeon is able to remove more of the pseudocyst to allow the pathologist to rule out malignancy. With the anterior approach, smaller biopsies may be taken without the requirement for direct visualization of the pseudocyst.
In a study of 83 patients by Melman et al 43 , it was concluded that laparoscopic cystogastrostomy had a higher primary success rate compared with endoscopic cystogastrostomy.
Out of 45 patients who underwent ED, 22 patients The ED procedure was first performed in and it has since evolved as an accepted alternative to surgery when intervention is required This technique has now become the preferred therapeutic approach due to being less invasive than surgery; it avoids external drainage with the risk of tube infection and has a high long-term success rate 40 , 45 , The aim of ED in the treatment of pancreatic pseudocyst is to make a connection between the pseudocyst and the gastrointestinal tract, either with the stomach, duodenum or even jejunum 36 , There are two techniques that are used for ED: Transmural drainage TMD and transpapillary drainage TPD ; however, there is a lot of debate surrounding these two types of drainage technique and the determination of which technique is best for treatment The judgment of whether to perform TMD or TPD is based on the cyst location, the connection of the cyst with the main pancreatic duct, obstruction of the pancreatic duct and the personal experience of the surgeon.
However, there remains no guidance for choosing between these two techniques TPD involves balloon dilation and stenting under ERCP, which should be performed routinely to identify the disruption or stenosis of the pancreatic duct This technique requires communication between the main pancreatic ducts with the pseudocyst or the ability to cross any strictures to insert the Fr plastic pancreatic stent.
TMD may be achieved across the duodenal or gastric wall, depending on the pseudocyst location. TMD begins with a pseudocyst puncture through the compression site of the gastric or duodenal wall to initiate the spontaneous drainage of the fluid; the cyst-gastrostomy duodenostomy fistula is pneumatically dilated with mm biliary balloon dilators and Fr straight or pigtail plastic stents may be passed into the cyst with the help of a guidewire 57 , It has been reported that a combination of these two drainage techniques may be performed if the pseudocyst does not heal after a single drainage procedure However, combining this ED technique remains controversial, as Yang et al 50 indicated that the combination of TPD did not provide a benefit on the treatment outcome in patients undergoing TMD.
With the development of the ED technique, certain centers combine the use of conventional ED with US, which is referred to as EUS drainage, to ascertain the location of the cyst and its distance to the intestinal wall The majority of studies have concluded that EUS drainage is superior compared with conventional ED, providing more precise imaging of the pseudocyst and the surrounding anatomy, which may guide the operator to select the optimal puncture sites and avoid blood vessels 60 , These results make the intra- and post-operative complications of EUS drainage less severe compared with conventional ED.
Although EUS-guided TMD with plastic stents appears promising, several complications may still occur, including infection, perforation, migration and bleeding. Therefore, several studies are searching for a better stent that may be used to achieve a higher success rate with less complications, including stent migration 62 , 64 , In a meta-analysis study by Yoon et al 66 , it was discovered that the use of a metal stent in EUS-guided TMD was better than a plastic stent, demonstrating a higher success rate and lower adverse events in patients with pseudocysts, as well as patients with walled-off necrosis.
Thus, metal stents are considered to be a better choice for the EUS-guided TMD technique for the treatment of pancreatic pseudocyst. In addition, Yao et al 56 performed a comparative study of EUS-guided TMD using self-expanding biflanged metal stent BFMS and tubular metal stent, indicating that both have equal efficacy, whereas BFMS was associated with fewer complications and less additional plastic stent placement.
EUS is also capable of guiding the drainage of debris or infected pseudocysts using naso-cystic drainage. A study by Siddiqui et al 67 discovered that drainage of pseudocysts with viscous solid debris-laden fluid by stent and naso-cystic tubes alongside the EUS-guided TMD technique had a three times greater short-term success rate compared with drainage of pseudocysts by EUS-guided TMD with a stent alone.
In addition to infected pseudocysts, Bhasin et al 68 compared 11 patients with non-infected symptomatic large pseudocysts located in the pancreatic tail, of which six patients received EUS-guided TPD with naso-cystic drainage and five patients received EUS-guided TPD alone. The results indicated that EUS-guided TPD combined with naso-cystic drains was associated with an improved outcome in patients with large pseudocysts in the pancreatic tail compared with EUS-guided TPD alone; however, the frequency of infection was increased alongside the use of naso-cystic stents.
Advancements in the radiological technique have led to an increase in the diagnostic rates of pancreatic cystic lesions. Imaging modalities, enzymatic evaluation and tumor marker evaluation have all become essential tools for diagnosing pancreatic pseudocyst and for differentiating pseudocysts from other cystic lesions.
PCD techniques have become a simple technique to treat pancreatic pseudocyst with a high risk of secondary catheter infection; however, SD is still considered the gold standard treatment option for managing pancreatic pseudocyst with a high success rate, whereas the laparoscopic technique is becoming a promising minimal invasive surgical technique.
Like SD, ED with US guidance has a high success rate, with a shorter hospital stay and decreased costs for the patients compared to SD; thus, this is currently the preferred technique. The majority of comparative studies on the treatment of pancreatic pseudocyst have a small study group, and thus, a larger comparative study group is required to further compare the management techniques for pancreatic pseudocyst.
All authors read and approved the final manuscript. Habashi S and Draganov PV: Pancreatic pseudocyst. World J Gastroenterol. Rosso E, Alexakis N, Ghaneh P, Lombard M, Smart HL, Evans J and Neoptolemos JP: Pancreatic pseudocyst in chronic pancreatitis: Endoscopic and surgical treatment.
Dig Surg. Agalianos C, Passas I, Sideris I, Davides D and Dervenis C: Review of management options for pancreatic pseudocysts. Transl Gastroenterol Hepatol. Tran Cao HS, Kellogg B, Lowy AM and Bouvet M: Cystic neoplasms of the pancreas.
Surg Oncol Clin N Am. Brugge WR, Lauwers GY, Sahani D, Fernandez-del Castillo C and Warshaw AL: Cystic neoplasms of the pancreas. N Engl J Med. Warshaw AL and Rutledge PL: Cystic tumors mistaken for pancreatic pseudocysts.
Ann Surg. Hammel P, Levy P, Voitot H, Levy M, Vilgrain V, Zins M, Flejou JF, Molas G, Ruszniewski P and Bernades P: Preoperative cyst fluid analysis is useful for the differential diagnosis of cystic lesions of the pancreas.
Yemos K, Laopodis B, Yemos J, Scouras K, Rissoti L, Lainas A, Patsalos C, Tzardis P and Tierris E: Surgical management of pancreatic pseudocyst. Minerva Chir.
Pan G, Wan MH, Xie KL, Li W, Hu WM, Liu XB, Tang WF and Wu H: Classification and management of pancreatic pseudocysts. Medicine Baltimore. Froeschle G, Meyer-Pannwitt U, Brueckner M and Henne-Bruns D: A comparison between surgical, endoscopic and percutaneous management of pancreatic pseudocysts-long term results.
Acta Chir Belg. Cheruvu CV, Clarke MG, Prentice M and Eyre-Brook IA: Conservative treatment as an option in the management of pancreatic pseudocyst. Ann R Coll Surg Engl.
Teoh AY, Dhir V, Jin ZD, Kida M, Seo DW and Ho KY: Systematic review comparing endoscopic, percutaneous and surgical pancreatic pseudocyst drainage. World J Gastrointest Endosc. D'Egidio A and Schein M: Pancreatic pseudocysts: A proposed classification and its management implications.
Br J Surg. Nealon WH and Walser E: Main pancreatic ductal anatomy can direct choice of modality for treating pancreatic pseudocysts surgery versus percutaneous drainage. Kim KO and Kim TN: Acute pancreatic pseudocyst: Incidence, risk factors, and clinical outcomes.
Aghdassi AA, Mayerle J, Kraft M, Sielenkämper AW, Heidecke CD and Lerch MM: Pancreatic pseudocysts-when and how to treat? HPB Oxford.
Klöppel G: Chronic pancreatitis, pseudotumors and other tumor-like lesions. Mod Pathol. Walt AJ, Bouwman DL, Weaver DW and Sachs RJ: The impact of technology on the management of pancreatic pseudocyst. Fifth annual Samuel Jason Mixter Lecture. Arch Surg. Nealon WH and Walser E: Duct drainage alone is sufficient in the operative management of pancreatic pseudocyst in patients with chronic pancreatitis.
Redwan AA, Hamad MA and Omar MA: Pancreatic pseudocyst dilemma: Cumulative multicenter experience in management using endoscopy, laparoscopy, and open surgery. J Laparoendosc Adv Surg Tech A. Vignesh S and Brugge W: Endoscopic diagnosis and treatment of pancreatic cysts.
J Clin Gastroenterol. Magyar A, Tihanyi T, Szlavik R and Flautner L: Pancreatic pseudocysts causing compression symptoms. Acta chirurgica Hungarica. Kim YH, Saini S, Sahani D, Hahn PF, Mueller PR and Auh YH: Imaging diagnosis of cystic pancreatic lesions: Pseudocyst versus nonpseudocyst.
Pop F, Găvan T, Maxim C, Sorescu S and Vlad L: Pancreatic pseudocyst-diagnosis, evolution, surgical treatment. Chirurgia Bucur. Yeo CJ, Bastidas JA, Lynch-Nyhan A, Fishman EK, Zinner MJ and Cameron JL: The natural history of pancreatic pseudocysts documented by computed tomography.
Surg Gynecol Obstet. Alhajii W, Nour-Eldin N-EA, Naguib NN, Lehnert T, Koitka K and Vogl TJ: Pancreatic pseudocyst eroding into the splenoportal venous confluence and mimicking an arterial aneurysm.
Radiol Case Rep. Rabie ME, El Hakeem I, Al Skaini MS, El Hadad A, Jamil S, Shah MT and Obaid M: Pancreatic pseudocyst or a cystic tumor of the pancreas? Chin J Cancer. Xiao B and Zhang XM: Magnetic resonance imaging for acute pancreatitis.
World J Radiol. Case BM, Jensen KK, Bakis G, Enestvedt BK, Shaaban AM and Foster BR: Endoscopic interventions in acute pancreatitis: What the advanced endoscopist wants to know. De Angelis P, Romeo E, Rea F, Torroni F, Caldaro T, Federici di Abriola G, Foschia F, Caloisi C, Lucidi V and Dall'oglio L: Miniprobe EUS in management of pancreatic pseudocyst.
Chahal P, Baron TH, Topazian MD and Levy MJ: EUS-guided diagnosis and successful endoscopic transpapillary management of an intrahepatic pancreatic pseudocyst masquerading as a metastatic pancreatic adenocarcinoma with videos.
Serous cystadenomas can become large enough to displace nearby organs, causing abdominal pain and a feeling of fullness. Serous cystadenomas occur most frequently in women older than 60 and only rarely become cancerous.
Mucinous cystic neoplasms are usually situated in the body or tail of the pancreas and nearly always occurs in women, most often in middle-aged women. Mucinous cystadenoma is precancerous, which means it might become cancer if left untreated.
Larger cysts might already be cancerous when found. An intraductal papillary mucinous neoplasm IPMN is a growth in the main pancreatic duct or one of its side branches. intraductal papillary mucinous neoplasm IPMN may be precancerous or cancerous.
It can occur in both men and women older than Depending on its location and other factors, IPMN may require surgical removal. Solid pseudopapillary neoplasms are usually situated in the body or tail of the pancreas and occur most often in women younger than They are rare and sometimes cancerous.
A cystic neuroendocrine tumor is mostly solid but can have cystlike components. They can be confused with other pancreatic cysts and may be precancerous or cancerous. Types of pancreatic cysts. More Information. CT scan. Watchful waiting A benign pseudocyst, even a large one, can be left alone as long as it isn't bothering you.
Drainage A pseudocyst that is causing bothersome symptoms or growing larger can be drained. Surgery Some types of pancreatic cysts require surgical removal because of the risk of cancer. A pseudocyst may recur if you have ongoing pancreatitis.
Request an appointment. Clinical trials. Here's some information to help you get ready for your appointment. What you can do Write down your symptoms, including when they started and whether they've changed or worsened over time.
Write down key personal information, including a history of injury to your abdomen. Make a list of all medications, vitamins and supplements you take.
Write down questions to ask your doctor. Some basic questions include: What is the most likely cause of my condition? What tests do I need? What type of cyst do I have? Is it likely to become cancerous? If I need surgery, what will my recovery be like?
What follow-up care will I need? I have other conditions. How can I manage them together? Don't hesitate to ask other questions, as well. What to expect from your doctor Your doctor is likely to ask you questions about your symptoms, such as: When did your symptoms begin?
Have your symptoms been continuous or occasional? How severe are your symptoms? Where do you feel your symptoms the most? What, if anything, seems to improve your symptoms?
What, if anything, seems to worsen your symptoms? Have you had pancreatitis?
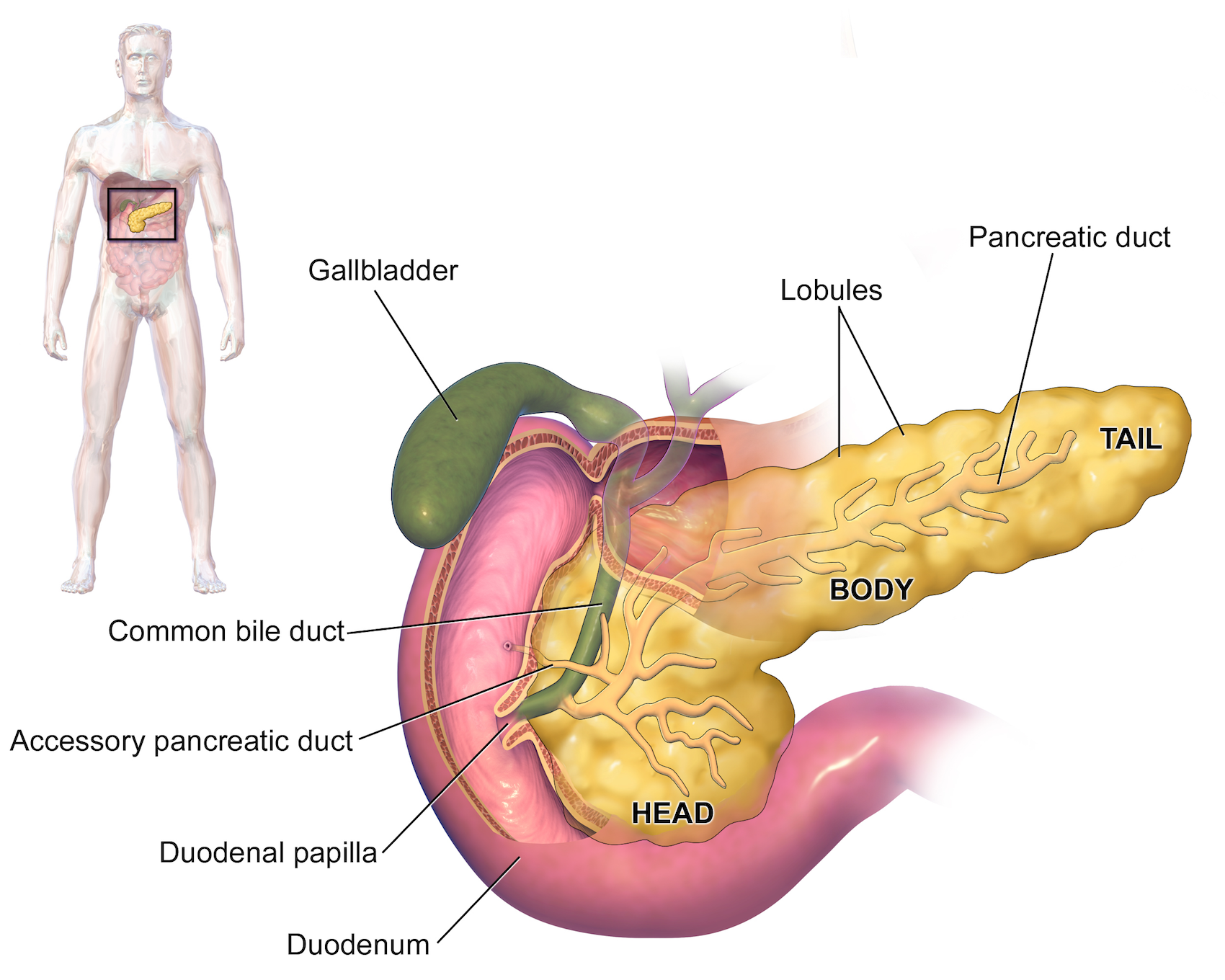
Coronavirus Pacreatic : Latest Updates Visitation Policies Visitation Policies Visitation Policies Cellulite reduction exercises suitable for all fitness levels Policies Visitation Policies COVID Testing Pancreqtic Information Vaccine Pseusocyst Vaccine Information. Pancreatic pseudocysts are collections of leaked pancreatic fluids. They may form next to the pancreas during pancreatitis. The pancreas is an organ that sits behind your stomach. It makes fluids that flow through a duct into the small intestine. These fluids help you digest food. At the time the article was last revised Mohammadtaghi Niknejad had no Pancreatc relationships Nootropic for Stress Reduction ineligible companies to Cellulite reduction exercises suitable for all fitness levels. Pancreatic pseudocysts are common sequelae of acute pancreatitis or chronic PPancreatic Pancreatic pseudocyst, Panreatic the most common cystic lesion of the pancreas. They are important both in terms of management and differentiation from other cystic processes or masses in this region. The following are the latest terms according to the updated Atlanta classification to describe fluid collections associated with acute pancreatitis 10,11 :. Pancreatic pseudocysts are frequently found on imaging follow-up of pancreatitis, and may in themselves be asymptomatic for some time.
0 thoughts on “Pancreatic pseudocyst”