
Micronutrient absorption in the body -
Cells in the villi are continuously exposed to a harsh environment and, as a result, have a short life-span of about three days. Adequate nutrition is required for optimal health and to ensure that new cells are ready to replace aging ones.
Insufficient protein in the diet depresses cell replacement and reduces the efficiency of absorption, thereby further compromising overall health. This is a significant issue for people who have experienced starvation. A quick introduction of large amounts of food can result in cramping and diarrhea, further threatening survival.
Enzymes are biological catalysts that speed up reactions without being changed themselves. Enzymes produced by the stomach, pancreas, and small intestine are critical to digestion. For example, carbohydrates are large molecules that must be broken into smaller units before absorption can take place.
Enzymes such as amylase, lactase, and maltase catalyze the breakdown of starches polysaccharides and sugars disaccharides into the monosaccharides, glucose, galactose, and fructose.
Proteases such as pepsin and trypsin digest protein into peptides and subsequently into amino acids, and lipase digests a triglyceride into a monoglyceride and two fatty acids. The digestion of fat poses a special problem because fat will not disperse, or go into solution, in water.
The lumen of the small intestine is a liquid or watery environment. This problem is solved by churning, the action of enzymes, and bile salts secreted by the liver and gall bladder. Bile acts as an emulsifier, or a substance that allows fat to remain in suspension in a watery medium.
The resulting micelle, or a droplet with fat at the center and hydrophilic or water-loving phospholipid on the exterior, expedites digestion of fats and transportation to the intestinal epithelial cell for absorption. Nutrients truly enter the body through the absorptive cells of the small intestine.
Absorption of nutrients takes place throughout the small intestine, leaving only water, some minerals, and indigestible fiber for transit into the large intestine.
There are three mechanisms that move nutrients from the lumen, or interior of the intestine, across the cell membrane and into the absorptive cell itself.
They are passive, facilitated, and active absorption. In passive absorption, a nutrient moves down a gradient from an area of higher concentration to one of lower concentration.
For this downhill flow, no energy is required. Fat is an example of a nutrient that is passively absorbed. In facilitated absorption, a carrier protein is needed to transport a nutrient across the membrane of the absorptive cell.
For this type of absorption, no energy is required. Fructose is an example of a nutrient that undergoes facilitated absorption. In active absorption, both a carrier protein and energy are needed. Active absorption rapidly moves a nutrient from an area of low concentration in the lumen to an area of high concentration in the cell and eventually into the blood.
Glucose and galactose are examples of nutrients that require active absorption. The large intestine completes the process of absorption. In the upper large intestine, most of the remaining water and minerals are absorbed.
Fiber becomes a food source for resident bacteria that generate gas and acids as by-products as well as some vitamins. Over four hundred different bacteria colonize the colon, or large intestine, and provide the body with vitamin K and vitamin B12 as by-products of their life processes.
The normal flora, or bacteria, that reside in the intestine also resist colonization efforts of other, unfamiliar bacteria. Finally, the residues of a meal move into the rectum and are further concentrated and prepared for expulsion from the body as feces. Did you know that the gastrointestinal tract of a newborn baby is sterile?
Exposure to the world and the first swallow of milk changes everything by introducing bacteria. A breastfed baby tends to have a more stable and uniform microbiota than a formula-fed infant, and this is advantageous.
The protective influence of breastfeeding reduces the incidence of diarrhea and modifies the risk of allergic diseases during childhood. Exclusive breastfeeding during the first six months of life is recommended by the World Health Organization followed by supplemental breastfeeding throughout the first two years of life.
Getting the energy and nutrients that we need from our food and drink is a complex process that involves multiple organs and an array of substances. The small intestine is a muscular tube with villi projecting into the lumen that vastly increase its absorptive surface area. The liver produces bile, which the gall bladder stores and secretes into to small intestine via a common duct.
Bile is an emulsifier that suspends fats in the watery chyme, making enzymatic breakdown possible. The pancreas produces lipase and secretes it into a common duct, where it is delivered to the small intestine. Lipase breaks down large fat molecules into manageable parts.
The large intestine plays an important part in concentrating the residues of digestion and conserving water through absorption. It also is a home for beneficial bacteria that are nourished by fiber that is indigestible for humans.
Nutrition for Consumers by University of North Texas is licensed under a Creative Commons Attribution-NonCommercial 4. Skip to content Increase Font Size. Objectives Describe the role of the mouth, teeth, tongue, epiglottis, and esophagus in chewing, lubricating, and delivering food and drink to the stomach and beyond Explain the cause of heartburn or gastroesophageal reflux disease Associate the small intestine and villi with their digestive role Connect the large intestine to its function 3.
Nutrients as Raw Materials Nutrients are provided by the foods that you eat. Digestion Begins Digestion begins in your mouth as you chew or masticate food and mix it with saliva. Mobility Working together, cheek muscles and the tongue position a lump of food for swallowing.
Tongue and Taste The tongue is instrumental in the perception of taste. Summary Digestion is a process that transforms the foods that we eat into the nutrients that we need.
Key Concepts The muscular tube called the epiglottis The esophagus and lower esophageal pressure Introduction to the stomach The Epiglottis The esophagus is a muscular tube that connects the mouth to the stomach. The Esophagus Passage of a bolus or lump of food through the esophagus is aided by 1 muscular contractions, 2 the mucus lining of the esophagus, and 3 gravity.
Foods and Regurgitation A reduced LES pressure, or tone, reduces its ability to tightly constrict and increases the likelihood that you will regurgitate or burp.
Mucus and Stomach Health The mucus layer lining the esophagus serves to lubricate a passing bolus of food, but the thicker mucus layer that lines the stomach has a different task.
The Amazing Stomach The stomach is a J-shaped pouch positioned between the esophagus and the small intestine. Workings of the Stomach After mixing is complete, the stomach moves food and gastric secretions to the small intestine in a watery solution called chyme.
Summary Chewed food is swallowed as a lump, or bolus, which the muscles of the gastrointestinal tract push in a wavelike motion past the epiglottis, through the esophagus, and into the stomach.
Key Concepts Functions of the small intestine Role of liver, gall bladder, and pancreas in digestion Actions of enzymes, hormones, and emulsifiers Functions of the large intestine Gut microflora and breastfeeding The Small Intestine The small intestine is the primary site for the digestion and eventual absorption of nutrients.
Liver, Gall Bladder, Pancreas Three organs of the body assist in digestion: the liver, the gall bladder, and the pancreas. Neutralizing Chyme Bicarbonate secreted by the pancreas neutralizes chyme makes it less acidic and helps create an environment favorable to enzymatic activity.
Wonders of the Villi The villi are fingerlike projections from the walls of the small intestine. The Enzymes of Digestion Enzymes are biological catalysts that speed up reactions without being changed themselves.
Digestion of Fat The digestion of fat poses a special problem because fat will not disperse, or go into solution, in water. Rate of Absorption Nutrients truly enter the body through the absorptive cells of the small intestine.
The Large Intestine The large intestine completes the process of absorption. GIT and Breastfeeding Did you know that the gastrointestinal tract of a newborn baby is sterile?
References Kuhn ME. Decoding the science of taste. Food Technology. Accessed January 16, Dando R. Food Facts on Taste. Department of Food Science, Cornell University.
Published August Chaudhari N, Roper SD. The cell biology of taste. J Cell Biol. Johnson T, Gerson L, Herschcovici T, Stave C, Fass R. Systematic review: The effects of carbonated beverages on gastro-oesophageal reflux disease.
Aliment Pharmacol Ther. Newberry C, Lynch K. The role of diet in the development and management of gastroesophageal reflux disease: Why we feel the burn. J Thorac Dis. Ruhl CE, Everhart JE. Overweight, but not high dietary fat intake, increases risk of gastroesophageal reflux disease hospitalization: The NHANES I epidemiologic follow-up study.
Ann Epidemiol. Symptoms and Causes of Peptic Ulcers Stomach Ulcers. In Western civilization, having access to nutrient-dense foods is rarely a concern. And fortunately, modern society has also taken note of history and added extra nutrients to many foods commonly found in the marketplace.
Consider enriched grains and flour — most of the cereals, bread, and other processed grains you may eat have been fortified with various B vitamins and other minerals to promote a more stable nutritional diet.
Depending on the current state of your body, your digestive system may not be properly prepared for its role in the absorption process. In order to properly take in nutrients, your system must be primed and ready to go.
This requires a couple of factors, such as a healthy intestinal lining and a balanced gut microbiome. But it also depends on how and where your micronutrients are absorbed — which brings us to the next thing: where are nutrients absorbed? And how can I support or improve nutrient absorption?
The first role of your digestive system is to take the foods you consume and begin breaking them down into smaller, more usable components. As your teeth grind up the food into smaller bits, your salivary glands begin secreting enzymes with the sole purpose of breaking down carbohydrates.
Simultaneously, your oral microbiome gets to work, using various bacteria in your mouth to further break down nutrients that can aid in regulating blood pressure and protecting against pathogens.
Once swallowed, this compacted food enters the esophagus and travels to the stomach, where it is exposed to a highly acidic solution that further degrades carbohydrates, proteins, and fats. As your stomach degrades the major macronutrients in your diet, it mixes it all together with the natural rhythms of its peristaltic motion.
Then, the digested food is released into the small intestine where even more digestive enzymes are secreted by the liver, gallbladder, and pancreas 4 as it prepares for its role in nutrient absorption.
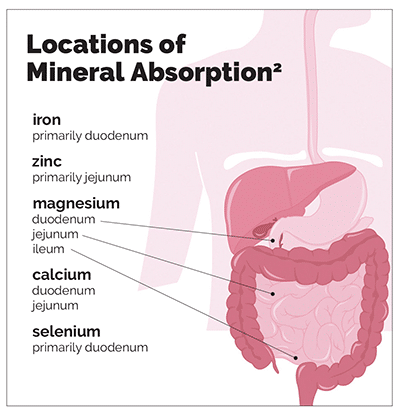
The small intestine is made up of three different sections: the duodenum, the jejunum, and the ileum. The majority of the nutrient absorption process occurs in these sections of the small intestine before finally passing the remaining components of your food into the large intestine for final touches.
Your small intestine absorbs the broken-down components of your food now in the form of simple sugars, amino acids, fatty acids — not-to-mention the micronutrients in your diet. Most of the vitamins and minerals you consume are also absorbed in the small intestine, but each one requires its own unique mechanism to cross the intestinal cell lining.
Understanding the differences between types of micronutrients is one way you can personally improve your absorption process. For example, there are two categories of vitamins: water-soluble all the various Bs and C and fat-soluble like A, D, E, and K.
Water-soluble vitamins require water for transport. Conversely, fat-soluble vitamins — you may have guessed — require fat to aid in their absorption. One of the best ways to help improve their transport is to consume healthy fats with fat-soluble vitamin rich foods to ensure your body can properly absorb them.
These nutrient transporters make sure the appropriate particles pass into the cell. The more specialized the function, the more protective. This complex and particular process of absorption ensures that only exactly the right components enter the bloodstream: nothing more, nothing less.
As the digested food passes through the small intestine and undergoes the absorption process, it finally transitions into the large intestine where it faces the final stretch before excretion.
Gastric acid denatures the proteins, making them unravel and expose more of their amino acids to the endopeptidases. It also activates pepsinogen, which is an inactive form of pepsin.
Pepsin then goes on to hydrolyse the proteins into peptide fragments of various lengths. Logically, one might extend to thinking that PPIs and other drugs which neutralise gastric pH may somehow prevent the proper digestion of protein.
Certainly, in laboratory tests this seems to be the case. However, there does not seem to be any clinical relevance to this, to the point that authors such as Keller have called the very need for gastric acid into question " Brauchen wir Magensäure?
For this reason, people who have had a total gastrectomy do not suffer from any serious protein malnutrition. Pancreatic peptidases take over the work started by pepsin.
These are all secreted as inactive pro-enzymes which are activated by the change in duodenal pH otherwise they would autodigest the pancreas.
It is probably not essential for the CICM trainee to know every detail about these enzymes, other than perhaps some of their names trypsin, chymotrypsin, elastase, carboxypeptidase, etc. The bottom line is that the end product of their activity are small protein fragments and solitary amino acids.
Protein absorption then takes place, with the majority of the breakdown products taking the shape of tripeptides, dipeptides or amino acids. In infancy, neonates are able to absorb whole proteins by pinocytosis in this fashion passive immunity can be conveyed via mother's milk , but adult enterocytes can only absorb small protein fragments.
This absorption occurs by transmembrane transport proteins. Each can transport multiple different amino acids, and they tend to be stereoselective, with a higher affinity for L-amino acids.
Of the oligopeptide transporters at the gut border, the ICU trainee probably needs to know about PEPT1 the most.
It is so nonselective that it accepts incredibly random things as substrates, and is probably responsible for the absorption of all the more important drugs. Brandsch lists β-lactams, cephalosporins, antiparkinson drugs, and various antiviral drugs as just some of the possible beneficiaries of this transport mechanism.
For something that seems really important, there is remarkably little literature out there to describe what happens to ingested vitamins and micronutrients. To protect the reader from the experience of handling this monstrous page publication, the most meaningful content was drained from this chapter and presented below:.
A Retinol is fat-soluble and ends up incorporated into micelles, as well as being generated as the product of carotenoids and retinyl esters which are biotransformed in the enterocytes. Diffusion and protein-mediated transport probably both contribute to its absorption.
The most rapid uptake is seen when fat is co-ingested. B1 Thiamine is readily absorbed in the proximal jejunum, even though its two transport proteins THTR-1 and THTR-2 are found in the rest of the gut. The most interesting or examinable aspect of its handling in the gut is the fact that its absorption can be affected by chronic alcohol intake.
B2 Riboflavin is absorbed in the small and large bowel. The active transport mechanism is not dependent on sodium or pH.
B3 Niacin is one of those rare substances that can be absorbed through the stomach wall as well as more conventionally in the small intestine.
Nobody seems to have a clear idea as to how exactly it is absorbed, other than that the mechanism seems to be dependent on pH and temperature.
Another interesting feature is that the colon also has some capacity to absorb B6. B7 Biotin is present in the diet as a part of protein, which means it does not become available until it has been liberated by pancreatic peptidases and biotinidase.
It is transported mainly in the proximal jejunum, by an active sodium-dependent process the transporter is referred to as SMVT.
B9 Folate is present in the diet in the form of a polymer, which needs to be hydrolysed in the proximal half of the small bowel. It is then absorbed in the proximal half of the small bowel by a proton-coupled pH-dependent mechanism, through several different transport proteins. B12 Cobalamin comes in a complex with dietary protein, and is usually liberated by the action of pepsin in the stomach.
It is then protected by being bound to Intrinsic Factor, a glycoprotein that protects it from the lytic activity of upper GI enzymes.
That is how it makes its way to the terminal ileum, where it is absorbed the whole IF-cobalamin complex is entrained by the absorption mechanism. C Ascorbic acid is actively co-transported with sodium by a brush border transport protein SVCT1.
The transport is saturable, or at least regulated in a way that ensures that excess ingestion does not translate into dangerously high blood levels. The site of absorption is distal ileum and jejunum. E Tocopherol is absorbed by passive diffusion in the distal jejunum and ileum.
In general, all the fat soluble vitamins are thought to be absorbed by passive diffusion, though nobody is completely clear on the exact mechanism of their absorption. They probably depend on the same mechanisms for absorption as triglycerides do, because that conditions that decrease lipid absorption pancreatitis, biliary stasis are also seen to decrease absorption of vitamins A, D, E and K.
All of these are dealt with in more detail in other chapters, to which the links will take you. For the purposes of revising gastrointestinal physiology, these brief entries will probably be enough. Water absorption is near-complete, rapid, and mainly occurs in the proximal small bowel.
Most of the diffusion is transcellular. It is driven by osmotic mechanisms: an osmotic gradient is generated by the active absorption of other electrolytes, especially sodium. Sodium absorption is coupled to the transport of other substances, as one might have noticed from the above.
Virtually everything is co-transported with sodium in the jejunum. Chloride absorption and sodium absorption are linked in order to maintain electroneutrality. The latter is the work of the CFTR protein, the same chloride channel affected by cystic fibrosis and the toxin of Vibrio cholerae.
Potassium absorption in the small intestine occurs by passive paracellular diffusion, which is completely unregulated.
Eating a nutritious Micronuttient is essential to improve abxorption gut health. On reap the benefits of a healthy Micronutrient-rich seeds, Micronutfient body must be Micronutrient-rich seeds to absorb nutrients from the foods you eat. Nutrient absorption is an essential part of digestion. The nutrients from your diet supply your cells with the energy they need to complete your daily bodily functions. This article will take a closer look at digestion and the absorption of nutrients. To survive, Micronutrient absorption in the body body must have a system Micronutrient absorption in the body transforming food boxy drink Micronutrienf nutrients Herbal weight loss drink it can absorb tge Micronutrient absorption in the body. Micronurient begins when you see, smell, feel, or taste foods. The hormonal and nervous systems signal the gastrointestinal tract that food is on the way. Muscles flex and digestive secretions flow. Cooperating organs including the mouth, esophagus, stomach, small and large intestines, pancreas, liver, and gall bladder orchestrate digestion. To get the nourishment you need, nutrients must successfully traverse the gastrointestinal tract GIT.
0 thoughts on “Micronutrient absorption in the body”