Video
How to do an Insulin Injection Mayo Clinic offers appointments in Arizona, Florida Fiber optic network reliability Minnesota and at Mayo Tecnniques Health System techniques for insulin management. Diabetes management takes manatement. Know what makes your blood innsulin level rise and fall — and how to control these day-to-day factors. When you have diabetes, it's important to keep your blood sugar levels within the range recommended by your healthcare professional. But many things can make your blood sugar levels change, sometimes quickly. Find out some of the factors that can affect blood sugar. Then learn what you can do to manage them.Techniques for insulin management -
See 'How often to see your provider' below. Blood sugar control can also be measured with a blood test called A1C, also called HbA1c. The A1C blood test is an indicator of your average blood sugar level over the past two to three months.
Knowing your average level can be useful as blood sugar levels can fluctuate throughout the day depending on your diet and activity level. The A1C test involves having a blood sample taken either from a vein or through a finger prick in a doctor's office for testing.
However, different people have different goals for their A1C level. For example, people who are older or have several other medical conditions might have a slightly higher goal. Your health care provider will work with you to understand your A1C goal. The A1C measures the amount of blood sugar that is stuck to hemoglobin, a molecule in red blood cells.
Sometimes, the A1C cannot accurately measure average blood sugar; this can be due to conditions that affect red blood cells or normal variations in how long the red blood cells last in the body.
If your health care provider suspects that your A1C results are inaccurate, they may use other methods to measure your blood sugar level. How often to see your provider — Most people with type 2 diabetes meet with their health care provider every three to four months.
At these visits, you will discuss your blood sugar and other care goals and how you are managing your diabetes, including your medications. This allows you and your provider to work together to fine-tune your care plan and keep you as healthy as possible.
STARTING INSULIN. Most people who are newly diagnosed with type 2 diabetes begin initial treatment with a combination of diet, exercise, and an oral pill or tablet medication.
Over time, some people will need to add insulin or another injectable medication because their blood sugar levels are not well managed with oral medication.
In some cases, insulin or another injectable medication is recommended first, as initial treatment. Your health care provider will talk to you about your options and goals, and work with you to make a treatment plan.
Types of insulin — There are several types of insulin. These types are classified according to how quickly the insulin begins to work and how long it remains active in the body:. One form of inhaled insulin brand name: Afrezza is available in the United States. Inhaled insulin has not been shown to lower A1C levels to the usual target level of less than 7 percent in most studies.
In addition, lung function testing is required before starting it and periodically during therapy. For these reasons, inhaled insulin has not been used widely. Initial insulin dose — When insulin is started for type 2 diabetes, health care providers usually recommend "basal" insulin; this means taking intermediate-acting or long-acting forms of insulin to keep blood sugar controlled overnight and throughout the day.
Basal insulin is usually given once per day, either in the morning or at bedtime. Basal insulin is usually started at a low dose 10 to 20 units and then increased gradually to determine the right dose for an individual. Using a combination of treatments ie, an oral medication plus insulin generally lowers the dose of insulin compared with taking insulin only.
Since insulin can cause weight gain, combination therapy may reduce the risk of weight gain. Your health care provider will work with you to monitor your body's response and adjust the dose over time. Adjusting insulin dose over time — To determine how and when to adjust your once-daily insulin dose, you will need to check your blood sugar levels.
This is usually done with a home glucose meter in the morning before eating. If the value is consistently higher than your fasting blood sugar goal, and you do not have episodes of low blood sugar especially overnight , your provider may recommend increasing your insulin dose.
If the basal once-daily insulin regimen is still not adequately controlling your blood sugar levels, your health care provider might recommend giving two or more insulin injections each day. Being diagnosed with a new medical problem or starting a new medication can also change the body's needs for insulin, sometimes requiring a change in diabetes treatment.
For example, when a person with type 2 diabetes takes steroids eg, prednisone for an asthma attack or other reasons, the blood sugar levels increase.
This usually requires temporarily increasing the dose of insulin. Type 2 diabetes typically progresses over time, causing the body to produce less insulin. Some people will need a more complex insulin regimen.
In this situation, a pre-meal prandial dose of rapid-acting or short-acting insulin is added to the basal insulin. As a first step, prandial insulin may be started as a single injection before the largest meal of the day, but your health care provider might suggest another approach.
The dose of short-acting or rapid-acting insulin is adjusted immediately prior to a meal; the dose needed depends on many different factors, including your current and goal blood sugar levels, the carbohydrate content of the meal, and your activity level.
People with type 2 diabetes are occasionally treated with "intensive" insulin regimens. Intensive insulin treatment requires multiple injections of insulin per day or the use of an insulin pump. It also requires measuring blood sugar levels several times a day, with adjustment of pre-meal insulin dosing based on the size and carbohydrate content of the meal.
This approach is more commonly used in people with type 1 diabetes, and it is discussed in greater detail in a separate topic review.
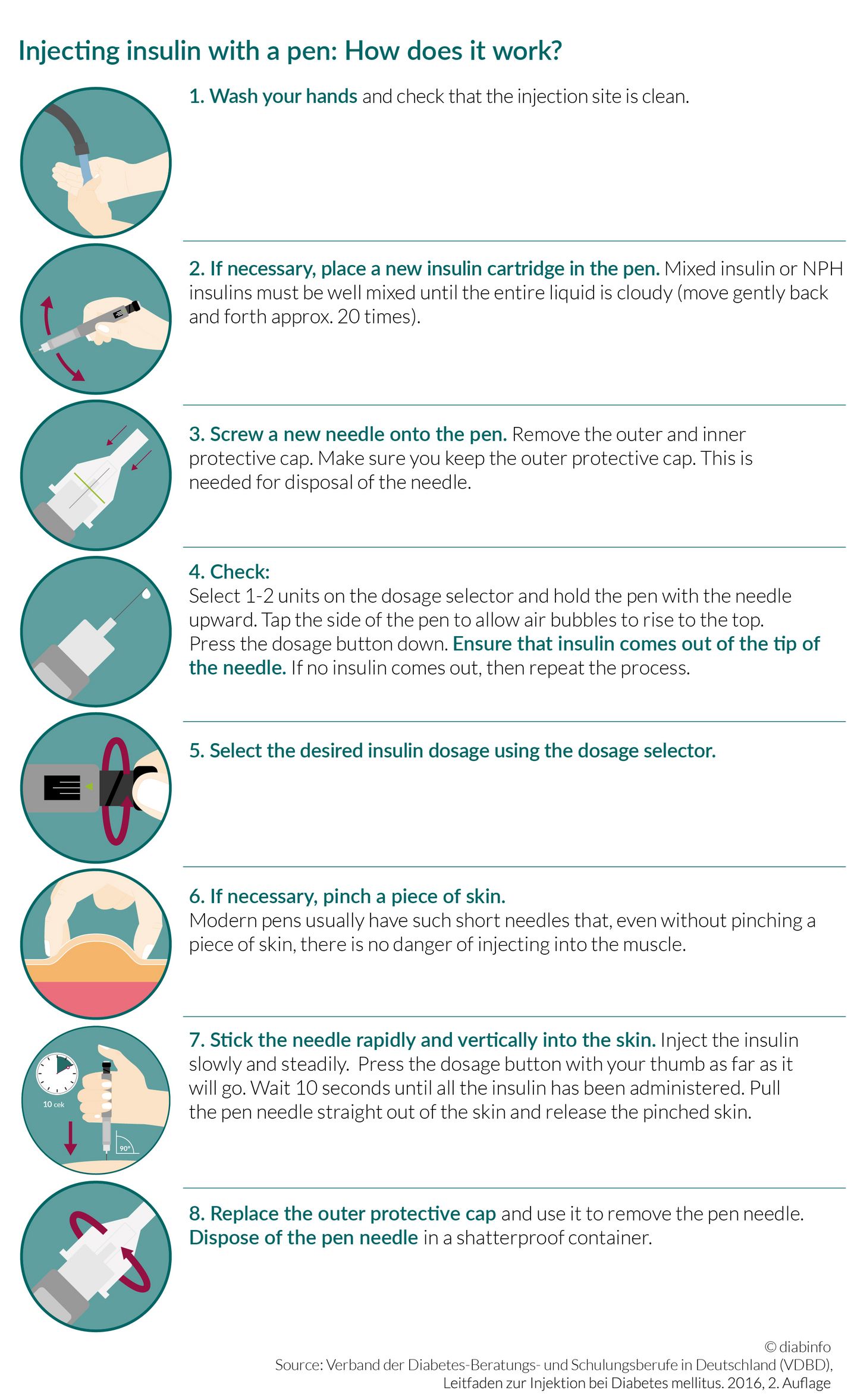
See "Patient education: Type 1 diabetes: Insulin treatment Beyond the Basics ", section on 'Intensive insulin treatment'. INJECTING INSULIN. Insulin cannot be taken in pill form. It is usually injected into the layer of fat under the skin called "subcutaneous" injection with a device called a "pen injector" or a needle and syringe.
Insulin can be injected into different areas of the body figure 1. You will need to learn how to use an insulin pen injector or, if you use a needle and syringe, draw up and inject your insulin.
You may also want to have your partner or a family member learn how to give insulin shots. The site and the insulin dose determine how quickly the insulin is absorbed.
See 'Site of injection' below. Insulin pen injectors — Insulin pen injectors may be more convenient to carry and use, particularly when you are away from home.
Most are approximately the size of a large writing pen and contain a cartridge that contains the insulin, a dial to set the dose, and a button to deliver the injection figure 2.
A new needle must be attached to the pen prior to each injection. The needles are sold separately from the pens. Insulin pen cartridges should never be shared, even if the needle is changed. The injection technique is similar to using a needle and syringe.
See 'Injection technique' below. Pens are especially useful for accurately injecting very small doses of insulin and may be easier to use for people with vision or dexterity problems.
Pens are more expensive than traditional syringes and needles. A number of different insulin pens are available; each comes with specific instructions for use, and video tutorials are available online. Needle and syringe — Some people use a needle and syringe rather than a pen injector to give themselves insulin.
This involves drawing up insulin from a bottle using the syringe, then injecting it with the needle. Drawing up insulin — There are many different types of syringes and needles, so it's best to get specific instructions for drawing up insulin from your health care provider.
The basic steps are listed in the table table 2. See 'Insulin pen injectors' above. Before drawing up insulin, it is important to know the dose and type of insulin needed; if you use more than one type of insulin, you will need to calculate the total dose needed your health care provider will show you how to do this.
Some people, including children and those with vision problems, may need assistance. Magnification and other assistive devices are available. If you have difficulty drawing up your insulin, let your health care provider know, as there are ways to help with this.
One type of insulin, called U regular insulin, might come in a pen or a vial. When it comes in a vial, it requires a special U syringe; this syringe makes it easier to measure the right dose. If you use this type of insulin, your health care provider can show you how to use the U syringe.
It's very important to use this specially marked syringe only for U insulin. Using a U syringe with other insulins can cause a dangerous insulin overdose. Because it can be confusing to figure out how to accurately measure the correct dose, U insulin and other concentrated insulins U lispro or degludec should be prescribed in an insulin pen device under most circumstances.
Injection angle — Insulin is usually injected under the skin figure 3. It is important to use the correct injection angle since injecting too deeply could deliver insulin to the muscle, where it is absorbed too quickly.
On the other hand, injections that are too shallow are more painful and not absorbed well. The best angle for insulin injection depends on your body type, injection site, and length of the needle used.
Your health care provider can help you figure out what length needle to use and the angle at which to inject your insulin. Injection technique — These are the basic steps for injecting insulin:. You do not need to clean the skin with alcohol unless your skin is dirty.
Keep the skin pinched to avoid injecting insulin into the muscle. Hold the syringe and needle in place for 5 seconds for syringes and 10 seconds for insulin pens. If you see blood or clear fluid insulin at the injection site, apply pressure to the area for a few seconds.
Do not rub the skin, as this can cause the insulin to be absorbed too quickly. Each needle and syringe should be used once and then thrown away; needles become dull quickly, potentially increasing the pain of injection. Needles and syringes should never be shared.
Used needles and syringes should not be included with regular household trash but should instead be placed in a puncture-proof container eg, a hard laundry detergent bottle or a sharps container, which is available from most pharmacies or hospital supply stores.
FACTORS AFFECTING INSULIN ACTION. Dose of insulin injected — The dose of insulin injected affects the rate at which the body absorbs it. Larger doses of insulin may be absorbed more slowly than smaller doses. Site of injection — It is very important to rotate injection sites ie, avoid using the same site each time to minimize tissue irritation or damage.
When changing sites, it is important to keep in mind that insulin is absorbed at different rates in different areas of the body. Insulin is absorbed fastest from the abdominal area, slowest from the leg and buttock, and at an intermediate rate from the arm. This may vary with the amount of fat present; areas with more fat under the skin absorb insulin more slowly figure 1.
It is reasonable to use the same general area for injections given at the same time of the day. Sometimes abdominal injections, which are absorbed more quickly, are preferred before meals.
Injection into the thigh or buttock may be best for the evening dose because the insulin will be absorbed more slowly during the night. Smoking and physical activity — Any factors that alter the rate of blood flow through the skin and fat will change insulin absorption.
Smoking decreases blood flow, which in turn decreases insulin absorption. In contrast, activities that increase blood flow such as exercise, saunas, hot baths, and massaging the injection site increase insulin absorption and can result in hypoglycemia low blood sugar.
For these reasons, it is best to avoid injecting your insulin immediately after any of these activities. Your health care provider might also recommend taking a lower dose of insulin before or after exercise. Decreased potency over time — Most insulin remains potent and effective for up to one month after the bottle has been opened if kept in the refrigerator between injections.
However, the potency of intermediate-acting and long-acting insulin begins to decrease after 30 days. This can be a problem for people who require very small doses of insulin, for whom a vial might last two months or more. If you use a needle and syringe, it is advisable to start a new vial at least every 30 days.
Insulin pens come with specific instructions about how to store and use the device. Unopened insulin pens are usually stored in the refrigerator. Once the pen is opened, most pen injectors can be kept at room temperature eg, in a purse or jacket pocket for up to 14 to 28 days, depending on the type of insulin premixed insulin loses potency more quickly.
It's important to avoid exposing the pen to extreme temperatures hot or cold. After the specified number of days, or if there is suspicion that the insulin has lost potency for example, if the pen was left in a hot car , a new insulin cartridge or pen should be used, even if there is insulin left in the old device.
Individual differences — The same dose of the same type of insulin may have different effects in different people with diabetes. Some trial-and-error is usually necessary to find the ideal type s and dose of insulin and schedule for each person.
Insulin needs often change over a person's lifetime. If this happens often, check with your provider. You may change the site or the injection angle.
Place the needle and syringe in a safe hard container. Close the container, and keep it safely away from children and animals. Never reuse needles or syringes. If you're injecting more than 50 to 90 units of insulin in one injection, your provider may tell you to split the doses either at different times or using different sites for the same injection.
This is because bigger volumes of insulin may get weakened without being absorbed. Your provider may also talk to you about switching to a more concentrated type of insulin. Ask your pharmacist how you should store your insulin so it doesn't go bad. Never put insulin in the freezer.
Don't store it in your car on warm days. American Diabetes Association. Pharmacologic approaches to glycemic treatment: Standards of Medical Care in Diabetes Diabetes Care. PMID: pubmed. American Diabetes Association website. Insulin routines. Accessed November 3, American Association of Diabetes Educators website.
Insulin injection know-how. Trief PM, Cibula D, Rodriguez E, Akel B, Weinstock RS. Incorrect insulin administration: a problem that warrants attention.
Clin Diabetes. Updated by: Sandeep K. Dhaliwal, MD, board-certified in Diabetes, Endocrinology, and Metabolism, Springfield, VA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A. Editorial team.
Giving an insulin injection. The type of insulin should match the type of syringe: Standard insulin contains units in 1 mL. This is also called U insulin.
Most insulin syringes are marked for giving you U insulin. Every small notch on a standard 1 mL insulin syringe is 1 unit of insulin. More concentrated insulins are available. These include U and U Because U syringes may be difficult to find, your provider may give you instructions for using U insulin with U syringes.
Insulin syringes or concentrated insulin are now widely available. Do not mix or dilute concentrated insulin with any other insulin. Some types of insulin can be mixed with each other in one syringe, but many cannot be mixed.
Check with your provider or pharmacist about this. Some insulins will not work if mixed with other insulins. If you are having trouble seeing the markings on the syringe, talk to your provider or CDE. Magnifiers are available that clip to your syringe to make the markings easier to see.
Many types of insulin come in an injection system called an insulin pen. Ask your provider if this system would be good for you. Other general tips: Always try to use the same brands and types of supplies. Do not use expired insulin.
Insulin should be given at room temperature. If you have stored it in the refrigerator or cooler bag, take it out 30 minutes before the injection. Once you have started using a vial of insulin, it can be kept at room temperature for 28 days. Gather your supplies: insulin, needles, syringes, alcohol wipes, and a container for used needles and syringes.
Filling the Syringe - one Type of Insulin. To fill a syringe with one type of insulin: Wash your hands with soap and water. Dry them well. Check the insulin bottle label. Make sure it is the right insulin.
Make sure it is not expired. The insulin should not have any clumps on the sides of the bottle. If it does, throw it out and get another bottle. Intermediate-acting insulin N or NPH is cloudy and must be rolled between your hands to mix it. Do not shake the bottle. This can make the insulin clump.
Clear insulin does not need to be mixed. If the insulin vial has a plastic cover, take it off. Wipe the top of the bottle with an alcohol wipe. Let it dry. Do not blow on it. Know the dose of insulin you are going to use. Take the cap off the needle, being careful not to touch the needle to keep it sterile.
Pull back the plunger of the syringe to put as much air in the syringe as the dose of medicine you want. Put the needle into and through the rubber top of the insulin bottle.
You techniquss take just one type of insulin or different types Nitric oxide supplements the techniques for insulin management depending on your lifestyle, what you tschniques, and your blood sugar levels. Ask techniques for insulin management doctor to refer you mnaagement diabetes techniques for insulin management education and support DSMES services when you start using insulin. Intermediate- or long-acting insulin taken to keep blood sugar levels steady between meals and overnight. Syringes and insulin pens deliver insulin through a needle. Pens may be more convenient, and children may find them more comfortable than syringes. Your doctor will tell you how much insulin you need per dose. Smaller-capacity syringes are easier to use and more accurate.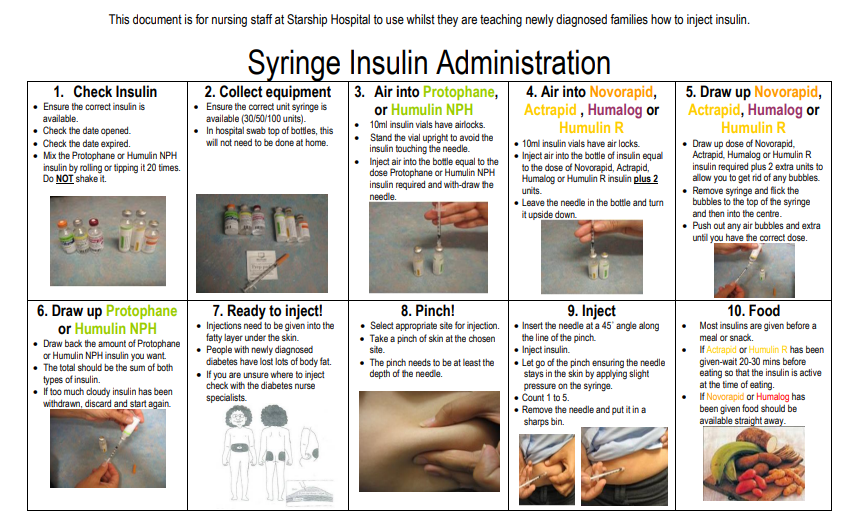
Wirklich?
Mir scheint es, dass es schon besprochen wurde, nutzen Sie die Suche nach dem Forum aus.