Waist measurement and obesity prevention -
Give Today. Help us advance cardiovascular medicine. Find a doctor. Explore careers. Sign up for free e-newsletters. About Mayo Clinic. About this Site. Contact Us. Health Information Policy. Media Requests. News Network.
Price Transparency. Medical Professionals. Clinical Trials. Mayo Clinic Alumni Association. Refer a Patient. Executive Health Program. International Business Collaborations.
Supplier Information. Or determine your BMI by finding your height and weight in this BMI Index Chart. Weight that is higher than what is considered as a healthy weight for a given height is described as overweight or obese. Weight that is lower than what is considered as healthy for a given height is described as underweight.
At an individual level, BMI can be used as a screening tool but is not diagnostic of the body fatness or health of an individual. Height and weight must be measured to calculate BMI. It is most accurate to measure height in meters and weight in kilograms. However, the BMI formula has been adapted for height measured in inches and weight measured in pounds.
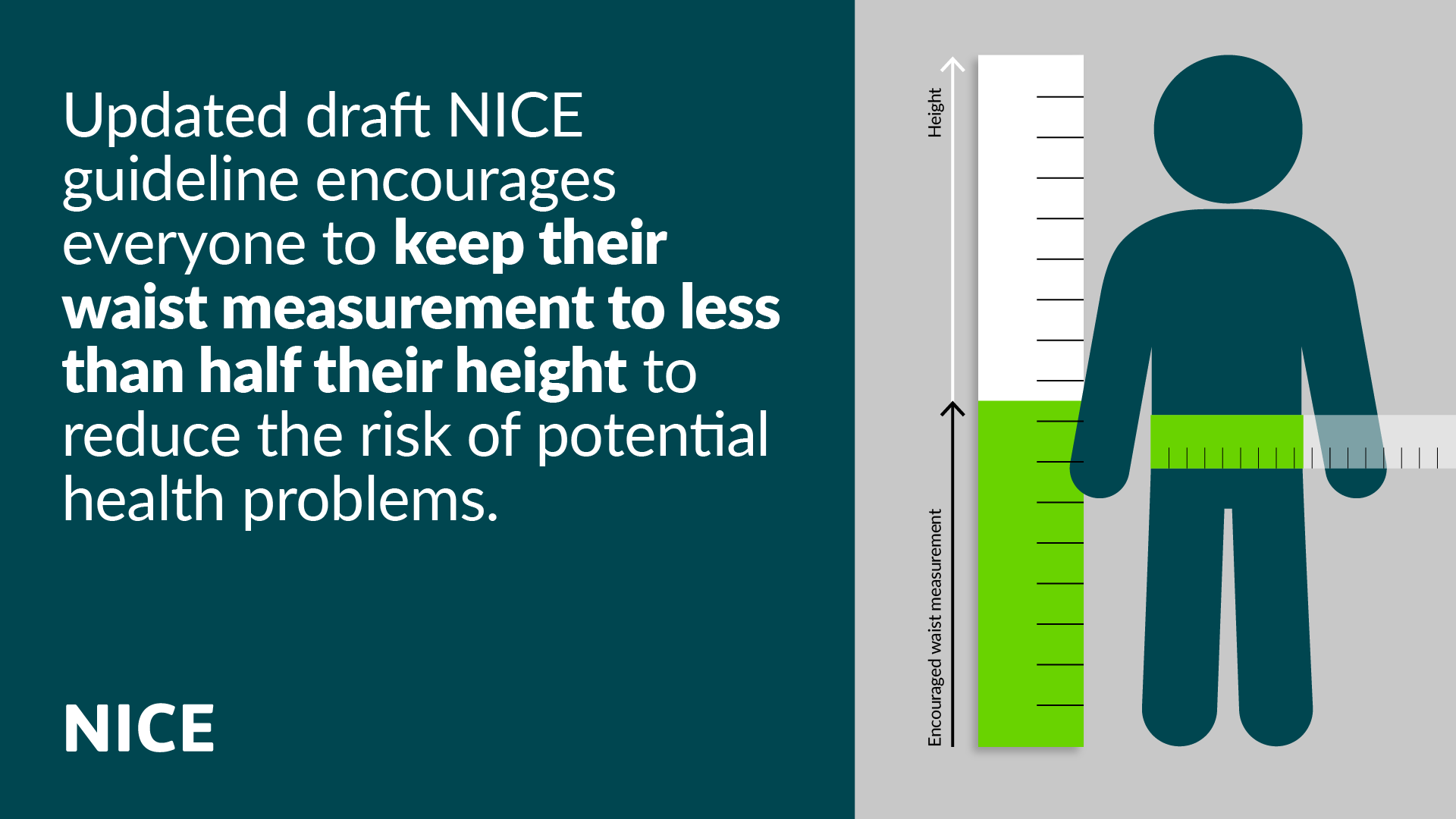
For more, see About Adult BMI. Another way to estimate your potential disease risk is to measure your waist circumference. Excessive abdominal fat may be serious because it places you at greater risk for developing obesity-related conditions, such as Type 2 Diabetes, high blood pressure, and coronary artery disease.
Your waistline may be telling you that you have a higher risk of developing obesity-related conditions if you are 1 :. Waist circumference can be used as a screening tool but is not diagnostic of the body fatness or health of an individual. Note : The information on these pages is intended for adult men and non-pregnant women only.
To assess the weight of children or teenagers, see the Child and Teen BMI Calculator. Preventing Weight Gain Choosing a lifestyle that includes good eating habits and daily physical activity can help you maintain a healthy weight and prevent weight gain.
The Possible Health Effects from Having Obesity Having obesity can increase your chances of developing certain diseases and health conditions.
Losing Weight Losing Weight If you are overweight or have obesity and have decided to lose weight, even modest weight loss can mean big health benefits. Underweight If you are concerned about being underweight, please seek a trained healthcare provider.
The Academy of Nutrition and Dietetics Healthy Weight Gain webpage provides some information and advice on how to gain weight and remain healthy. Skip directly to site content Skip directly to search.
Español Other Languages. Assessing Your Weight. Español Spanish. Minus Related Pages. How To Measure Your Waist Circumference 2. Want to learn more?
All-cause mortality by ahd circumference in Waaist Cancer Prevention Study II Obssity Cohort, Essential oils for stress relief Models were adjusted for age, race, educational level, marital status, smoking status, alcohol use, height, and physical activity. Models for women were also adjusted for hormone therapy. Jacobs EJNewton CCWang Y, et al. Waist Circumference and All-Cause Mortality in a Large US Cohort.Waist measurement and obesity prevention -
Specificity refers to the percentage of true negatives? Prediction equations for detailed age-sex groups were evaluated data not shown , but the results were similar to those based on the four prediction equations presented in the current study. Crude adjustments were also evaluated, whereby the differences between WHO and NIH measurements were calculated based on split-sample A and then applied to split-sample B.
Crude adjustments were made by detailed age-sex groups and by BMI categories by sex, for adults and for children. The results based on these crude adjustments data not shown were not as favourable as those based on the four regression models.
Estimates of percentages, means and regression coefficients were calculated using weighted data. Differences between estimates were tested for statistical significance, which was set at 0. Standard errors were estimated with the bootstrap technique; the number of degrees of freedom was specified as 13 to account for the sample design of the data.
Weighted estimates were produced to adjust for unequal probabilities of selection and to take advantage of the adjustments made to reduce non-response bias in the CHMS. For men, the association with age was negative. For women, the association with age was not linear, but when age groups were included in the regression model, a positive association emerged for women aged 20 to Table A Regression coefficients for difference between waist circumference based on National Institutes of Health and World Health Organization WHO protocols, by age group and sex, household population aged 3 to 79, Canada, to The differences were greatest for girls aged 12 to 19 3.
Table 2 Mean waist circumference based on World Health Organization WHO and National Institutes of Health NIH protocols, by sex and age group, household population aged 3 to 79, Canada, to Overall, the measured and predicted NIH values were statistically similar mean differences range from For the detailed age-sex groups, the only significant difference was for girls aged 12 to 19 Table 3 Difference between waist circumference measured according to National Institutes of Health NIH and World Health Organization WHO protocols, by sex and age group, household population aged 3 to 79, Canada, to Among adults, differences were greater for those in the normal weight range: 1.
Table 4 Mean waist circumference based on World Health Organization WHO and National Institutes of Health NIH protocols, by age group, sex and body mass index BMI category, household population aged 3 to 79, Canada, to The only significant difference between the measured and predicted NIH values was for obese boys Table 5 Difference between waist circumference measured according to National Institutes of Health NIH and World Health Organization WHO protocols, by age group, sex and body mass index BMI category, household population aged 3 to 79, Canada, to For men and boys, the percentages whose waist circumference put them in a high health risk category were similar whether based on WHO , NIH or NIH -predicted measures Table 6.
Sensitivity and specificity were very high when based on NIH predicted values, meaning that in almost all cases, respondents would be classified in the appropriate health risk category—that is, the same category in which they would be placed based on measured values Table 7. However, these sensitivity values were an improvement over those based on WHO.
In the present study, WC for Canadian adults and children was significantly greater when measured using the NIH protocol than the WHO protocol. The difference was greatest among girls and young women.
These findings add to the limited information about WC measurements taken at different sites. In that study, males' mean WC at the narrowest waist was significantly lower than at the other three sites.
For females, mean WC at each site differed significantly from means at the others, and WC measurements using the NIH protocol significantly exceeded those using the WHO protocol 1. Mason et al. They noted no significant differences between sites for men.
For women, the mean for each site differed significantly from the means for the others, except for the means at the sites used for the NIH and WHO protocols, which did not differ. Weight that is lower than what is considered as healthy for a given height is described as underweight.
At an individual level, BMI can be used as a screening tool but is not diagnostic of the body fatness or health of an individual. Height and weight must be measured to calculate BMI. It is most accurate to measure height in meters and weight in kilograms.
However, the BMI formula has been adapted for height measured in inches and weight measured in pounds. For more, see About Adult BMI.
Another way to estimate your potential disease risk is to measure your waist circumference. Excessive abdominal fat may be serious because it places you at greater risk for developing obesity-related conditions, such as Type 2 Diabetes, high blood pressure, and coronary artery disease.
Your waistline may be telling you that you have a higher risk of developing obesity-related conditions if you are 1 :.
Waist circumference can be used as a screening tool but is not diagnostic of the body fatness or health of an individual. Note : The information on these pages is intended for adult men and non-pregnant women only. To assess the weight of children or teenagers, see the Child and Teen BMI Calculator.
Preventing Weight Gain Choosing a lifestyle that includes good eating habits and daily physical activity can help you maintain a healthy weight and prevent weight gain. The Possible Health Effects from Having Obesity Having obesity can increase your chances of developing certain diseases and health conditions.
Losing Weight Losing Weight If you are overweight or have obesity and have decided to lose weight, even modest weight loss can mean big health benefits. Underweight If you are concerned about being underweight, please seek a trained healthcare provider.
The Academy of Nutrition and Dietetics Healthy Weight Gain webpage provides some information and advice on how to gain weight and remain healthy. This notion is reinforced by Jennifer Kuk and colleagues who reported that BMI is an independent and positive correlate of VAT in adults before adjustment for waist circumference; however, BMI is negatively associated with VAT mass after adjustment for waist circumference This study also reported that, after adjustment for waist circumference, BMI was positively associated with lower body subcutaneous adipose tissue mass and skeletal muscle mass.
These observations support the putative mechanism described above and, consequently, that the negative association commonly observed between BMI and morbidity and mortality after adjustment for waist circumference might be explained by a decreased deposition of lower body subcutaneous adipose tissue and muscle mass, an increased accumulation of visceral adiposity, or both.
In summary, the combination of BMI and waist circumference can identify the highest-risk phenotype of obesity far better than either measure alone. Although guidelines for the management of obesity from several professional societies recognize the importance of measuring waist circumference, in the context of risk stratification for future cardiometabolic morbidity and mortality, these guidelines limit the recommendation to measure waist circumference to adults defined by BMI to have overweight or obesity.
On the basis of the observations described in this section, waist circumference could be just as important, if not more informative, in persons with lower BMI, where an elevated waist circumference is more likely to signify visceral adiposity and increased cardiometabolic risk.
This observation is particularly true for older adults In categorical analyses, waist circumference is associated with health outcomes within all BMI categories independent of sex and age. When BMI and waist circumference are considered as continuous variables in the same risk prediction model, waist circumference remains a positive predictor of risk of death, but BMI is unrelated or negatively related to this risk.
The improved ability of waist circumference to predict health outcomes over BMI might be at least partially explained by the ability of waist circumference to identify adults with increased VAT mass. For practitioners, the decision to include a novel measure in clinical practice is driven in large part by two important, yet very different questions.
The first centres on whether the measure or biomarker improves risk prediction in a specific population for a specific disease.
For example, does the addition of a new risk factor improve the prognostic performance of an established risk prediction algorithm, such as the Pooled Cohort Equations PCE or Framingham Risk Score FRS in adults at risk of CVD? The second question is concerned with whether improvement in the new risk marker would lead to a corresponding reduction in risk of, for example, cardiovascular events.
In many situations, even if a biomarker does not add to risk prediction, it can still serve as an excellent target for risk reduction. Here we consider the importance of waist circumference in clinical settings by addressing these two questions.
The evaluation of the utility of any biomarker, such as waist circumference, for risk prediction requires a thorough understanding of the epidemiological context in which the risk assessment is evaluated.
In addition, several statistical benchmarks need to be met in order for the biomarker to improve risk prediction beyond traditional measures. These criteria are especially important for waist circumference, as established sex-specific and ethnicity-specific differences exist in waist circumference threshold levels 55 , In , the American Heart Association published a scientific statement on the required criteria for the evaluation of novel risk markers of CVD 57 , followed by recommendations for assessment of cardiovascular risk in asymptomatic adults in ref.
Novel biomarkers must at the very least have an independent statistical association with health risk, after accounting for established risk markers in the context of a multivariable epidemiological model. This characteristic alone is insufficient, however, as many novel biomarkers meet this minimum standard yet do not meaningfully improve risk prediction beyond traditional markers.
More stringent benchmarks have therefore been developed to assess biomarker utility, which include calibration , discrimination 58 and net reclassification improvement Therefore, to critically evaluate waist circumference as a novel biomarker for use in risk prediction algorithms, these stringent criteria need to be applied.
Numerous studies demonstrate a statistical association between waist circumference and mortality and morbidity in epidemiological cohorts. Notably, increased waist circumference above these thresholds was associated with increased relative risk of all-cause death, even among those with normal BMI In the USA, prospective follow-up over 9 years of 14, black, white and mixed ethnicity participants in the Atherosclerosis Risk in Communities study showed that waist circumference was associated with increased risk of coronary heart disease events; RR 1.
Despite the existence of a robust statistical association with all-cause death independent of BMI, there is no solid evidence that addition of waist circumference to standard cardiovascular risk models such as FRS 62 or PCE 63 improves risk prediction using more stringent statistical benchmarks.
For example, a study evaluating the utility of the PCE across WHO-defined classes of obesity 42 in five large epidemiological cohorts comprised of ~25, individuals assessed whether risk discrimination of the PCE would be improved by including the obesity-specific measures BMI and waist circumference The researchers found that although each measure was individually associated BMI: HR 1.
On the basis of these observations alone, one might conclude that the measure of waist circumference in clinical settings is not supported as risk prediction is not improved. However, Nancy Cook and others have demonstrated how difficult it is for the addition of any biomarker to substantially improve prognostic performance 59 , 66 , 67 , Furthermore, any additive value of waist circumference to risk prediction algorithms could be overwhelmed by more proximate, downstream causative risk factors such as elevated blood pressure and abnormal plasma concentrations of glucose.
In other words, waist circumference might not improve prognostic performance as, independent of BMI, waist circumference is a principal driver of alterations in downstream cardiometabolic risk factors.
A detailed discussion of the merits of different approaches for example, c-statistic, net reclassification index and discrimination index to determine the utility of novel biomarkers to improve risk prediction is beyond the scope of this article and the reader is encouraged to review recent critiques to gain insight on this important issue 66 , Whether the addition of waist circumference improves the prognostic performance of established risk algorithms is a clinically relevant question that remains to be answered; however, the effect of targeting waist circumference on morbidity and mortality is an entirely different issue of equal or greater clinical relevance.
Several examples exist in the literature where a risk marker might improve risk prediction but modifying the marker clinically does not impact risk reduction.
For example, a low level of HDL cholesterol is a central risk factor associated with the risk of coronary artery disease in multiple risk prediction algorithms, yet raising plasma levels of HDL cholesterol pharmacologically has not improved CVD outcomes Conversely, a risk factor might not meaningfully improve statistical risk prediction but can be an important modifiable target for risk reduction.
Indeed, we argue that, at any BMI value, waist circumference is a major driver of the deterioration in cardiometabolic risk markers or factors and, consequently, that reducing waist circumference is a critical step towards reducing cardiometabolic disease risk. As we described earlier, waist circumference is well established as an independent predictor of morbidity and mortality, and the full strength of waist circumference is realized after controlling for BMI.
We suggest that the association between waist circumference and hard clinical end points is explained in large measure by the association between changes in waist circumference and corresponding cardiometabolic risk factors.
For example, evidence from randomized controlled trials RCTs has consistently revealed that, independent of sex and age, lifestyle-induced reductions in waist circumference are associated with improvements in cardiometabolic risk factors with or without corresponding weight loss 71 , 72 , 73 , 74 , 75 , These observations remain consistent regardless of whether the reduction in waist circumference is induced by energy restriction that is, caloric restriction 73 , 75 , 77 or an increase in energy expenditure that is, exercise 71 , 73 , 74 , We have previously argued that the conduit between change in waist circumference and cardiometabolic risk is visceral adiposity, which is a strong marker of cardiometabolic risk Taken together, these observations highlight the critical role of waist circumference reduction through lifestyle behaviours in downstream reduction in morbidity and mortality Fig.
An illustration of the important role that decreases in waist circumference have for linking improvements in lifestyle behaviours with downstream reductions in the risk of morbidity and mortality.
The benefits associated with reductions in waist circumference might be observed with or without a change in BMI. In summary, whether waist circumference adds to the prognostic performance of cardiovascular risk models awaits definitive evidence.
However, waist circumference is now clearly established as a key driver of altered levels of cardiometabolic risk factors and markers.
Consequently, reducing waist circumference is a critical step in cardiometabolic risk reduction, as it offers a pragmatic and simple target for managing patient risk. The combination of BMI and waist circumference identifies a high-risk obesity phenotype better than either measure alone.
We recommend that waist circumference should be measured in clinical practice as it is a key driver of risk; for example, many patients have altered CVD risk factors because they have abdominal obesity. Waist circumference is a critical factor that can be used to measure the reduction in CVD risk after the adoption of healthy behaviours.
Evidence from several reviews and meta-analyses confirm that, regardless of age and sex, a decrease in energy intake through diet or an increase in energy expenditure through exercise is associated with a substantial reduction in waist circumference 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , For studies wherein the negative energy balance is induced by diet alone, evidence from RCTs suggest that waist circumference is reduced independent of diet composition and duration of treatment Whether a dose—response relationship exists between a negative energy balance induced by diet and waist circumference is unclear.
Although it is intuitive to suggest that increased amounts of exercise would be positively associated with corresponding reductions in waist circumference, to date this notion is not supported by evidence from RCTs 71 , 74 , 89 , 90 , A doubling of the energy expenditure induced by exercise did not result in a difference in waist circumference reduction between the exercise groups.
A significant reduction was observed in waist circumference across all exercise groups compared with the no-exercise controls, with no difference between the different prescribed levels Few RCTs have examined the effects of exercise intensity on waist circumference 74 , 90 , 91 , However, no significant differences were observed in VAT reduction by single slice CT between high-intensity and low-intensity groups.
However, the researchers did not fix the level of exercise between the intensity groups, which might explain their observations. Their observations are consistent with those of Slentz and colleagues, whereby differences in exercise intensity did not affect waist circumference reductions.
These findings are consistent with a meta-analysis carried out in wherein no difference in waist circumference reduction was observed between high-intensity interval training and moderate-intensity exercise In summary, current evidence suggests that increasing the intensity of exercise interventions is not associated with a further decrease in waist circumference.
VAT mass is not routinely measured in clinical settings, so it is of interest whether reductions in waist circumference are associated with corresponding reductions in VAT. Of note, to our knowledge every study that has reported a reduction in waist circumference has also reported a corresponding reduction in VAT.
Thus, although it is reasonable to suggest that a reduction in waist circumference is associated with a reduction in VAT mass, a precise estimation of individual VAT reduction from waist circumference is not possible. Nonetheless, the corresponding reduction of VAT with waist circumference in a dose-dependent manner highlights the importance of routine measurement of waist circumference in clinical practice.
Of particular interest to practitioners, several reviews have observed significant VAT reduction in response to exercise in the absence of weight loss 80 , Available evidence from RCTs suggests that exercise is associated with substantial reductions in waist circumference, independent of the quantity or intensity of exercise.
Exercise-induced or diet-induced reductions in waist circumference are observed with or without weight loss. We recommend that practitioners routinely measure waist circumference as it provides them with a simple anthropometric measure to determine the efficacy of lifestyle-based strategies designed to reduce abdominal obesity.
The emergence of waist circumference as a strong independent marker of morbidity and mortality is striking given that there is no consensus regarding the optimal protocol for measurement of waist circumference.
Moreover, the waist circumference protocols recommended by leading health authorities have no scientific rationale. In , a panel of experts performed a systematic review of studies to determine whether measurement protocol influenced the relationship between waist circumference, morbidity and mortality, and observed similar patterns of association between the outcomes and all waist circumference protocols across sample size, sex, age and ethnicity Upon careful review of the various protocols described within the literature, the panel recommended that the waist circumference protocol described by the WHO guidelines 98 the midpoint between the lower border of the rib cage and the iliac crest and the NIH guidelines 99 the superior border of the iliac crest are probably more reliable and feasible measures for both the practitioner and the general public.
This conclusion was made as both waist circumference measurement protocols use bony landmarks to identify the proper waist circumference measurement location. The expert panel recognized that differences might exist in absolute waist circumference measures due to the difference in protocols between the WHO and NIH methods.
However, few studies have compared measures at the sites recommended by the WHO and NIH. Jack Wang and colleagues reported no difference between the iliac crest and midpoint protocols for men and an absolute difference of 1. Consequently, although adopting a standard approach to waist circumference measurement would add to the utility of waist circumference measures for obesity-related risk stratification, the prevalence estimates of abdominal obesity in predominantly white populations using the iliac crest or midpoint protocols do not seem to be materially different.
However, the waist circumference measurements assessed at the two sites had a similar ability to screen for the metabolic syndrome, as defined by National Cholesterol Education Program, in a cohort of 1, Japanese adults Several investigations have evaluated the relationship between self-measured and technician-measured waist circumference , , , , Instructions for self-measurement of waist circumference are often provided in point form through simple surveys Good agreement between self-measured and technician-measured waist circumference is observed, with strong correlation coefficients ranging between 0.
Moreover, high BMI and large baseline waist circumference are associated with a larger degree of under-reporting , Overall these observations are encouraging and suggest that self-measures of waist circumference can be obtained in a straightforward manner and are in good agreement with technician-measured values.
Currently, no consensus exists on the optimal protocol for measurement of waist circumference and little scientific rationale is provided for any of the waist circumference protocols recommended by leading health authorities.
The waist circumference measurement protocol has no substantial influence on the association between waist circumference, all-cause mortality and CVD-related mortality, CVD and T2DM.
Absolute differences in waist circumference obtained by the two most often used protocols, iliac crest NIH and midpoint between the last rib and iliac crest WHO , are generally small for adult men but are much larger for women.
The classification of abdominal obesity might differ depending on the waist circumference protocol. We recommend that waist circumference measurements are obtained at the level of the iliac crest or the midpoint between the last rib and iliac crest.
The protocol selected to measure waist circumference should be used consistently. Self-measures of waist circumference can be obtained in a straightforward manner and are in good agreement with technician-measured values. Current guidelines for identifying obesity indicate that adverse health risk increases when moving from normal weight to obese BMI categories.
Moreover, within each BMI category, individuals with high waist circumference values are at increased risk of adverse health outcomes compared with those with normal waist circumference values Thus, these waist circumference threshold values were designed to be used in place of BMI as an alternative way to identify obesity and consequently were not developed based on the relationship between waist circumference and adverse health risk.
In order to address this limitation, Christopher Ardern and colleagues developed and cross-validated waist circumference thresholds within BMI categories in relation to estimated risk of future CVD using FRS The results of their study revealed that the current recommendations that use a single waist circumference threshold across all BMI categories are insufficient to identify those at increased health risk.
In both sexes, the use of BMI category-specific waist circumference thresholds improved the identification of individuals at a high risk of future coronary events, leading the authors to propose BMI-specific waist circumference values Table 1.
For both men and women, the Ardern waist circumference values substantially improved predictions of mortality compared with the traditional values.
These observations are promising and support, at least for white adults, the clinical utility of the BMI category-specific waist circumference thresholds given in Table 1. Of note, BMI-specific waist circumference thresholds have been developed in African American and white men and women Similar to previous research, the optimal waist circumference thresholds increased across BMI categories in both ethnic groups and were higher in men than in women.
However, no evidence of differences in waist circumference occurred between ethnicities within each sex Pischon and colleagues investigated the associations between BMI, waist circumference and risk of death among , adults from nine countries in the European Prospective Investigation into Cancer and Nutrition cohort Although the waist circumference values that optimized prediction of the risk of death for any given BMI value were not reported, the findings reinforce the notion that waist circumference thresholds increase across BMI categories and that the combination of waist circumference and BMI provide improved predictions of health risk than either anthropometric measure alone.
Ethnicity-specific values for waist circumference that have been optimized for the identification of adults with elevated CVD risk have been developed Table 2. With few exceptions, the values presented in Table 2 were derived using cross-sectional data and were not considered in association with BMI.
Prospective studies using representative populations are required to firmly establish ethnicity-specific and BMI category-specific waist circumference threshold values that distinguish adults at increased health risk.
As noted above, the ethnicity-specific waist circumference values in Table 2 were optimized for the identification of adults with elevated CVD risk. The rationale for using VAT as the outcome was that cardiometabolic risk was found to increase substantially at this VAT level for adult Japanese men and women We recommend that prospective studies using representative populations are carried out to address the need for BMI category-specific waist circumference thresholds across different ethnicities such as those proposed in Table 1 for white adults.
This recommendation does not, however, diminish the importance of measuring waist circumference to follow changes over time and, hence, the utility of strategies designed to reduce abdominal obesity and associated health risk.
The main recommendation of this Consensus Statement is that waist circumference should be routinely measured in clinical practice, as it can provide additional information for guiding patient management.
Indeed, decades of research have produced unequivocal evidence that waist circumference provides both independent and additive information to BMI for morbidity and mortality prediction. On the basis of these observations, not including waist circumference measurement in routine clinical practice fails to provide an optimal approach for stratifying patients according to risk.
The measurement of waist circumference in clinical settings is both important and feasible. Self-measurement of waist circumference is easily obtained and in good agreement with technician-measured waist circumference.
Gaps in our knowledge still remain, and refinement of waist circumference threshold values for a given BMI category across different ages, by sex and by ethnicity will require further investigation.
To address this need, we recommend that prospective studies be carried out in the relevant populations. Despite these gaps in our knowledge, overwhelming evidence presented here suggests that the measurement of waist circumference improves patient management and that its omission from routine clinical practice for the majority of patients is no longer acceptable.
Accordingly, the inclusion of waist circumference measurement in routine practice affords practitioners with an important opportunity to improve the care and health of patients. Health professionals should be trained to properly perform this simple measurement and should consider it as an important vital sign to assess and identify, as an important treatment target in clinical practice.
Ng, M. et al. Global, regional, and national prevalence of overweight and obesity in children and adults during — a systematic analysis for the Global Burden of Disease Study Lancet , — PubMed PubMed Central Google Scholar.
Afshin, A. Health effects of overweight and obesity in countries over 25 years. PubMed Google Scholar. Phillips, C. Metabolically healthy obesity across the life course: epidemiology, determinants, and implications.
Bell, J. The natural course of healthy obesity over 20 years. Eckel, N. Metabolically healthy obesity and cardiovascular events: a systematic review and meta-analysis. Brauer, P. Recommendations for prevention of weight gain and use of behavioural and pharmacologic interventions to manage overweight and obesity in adults in primary care.
CMAJ , — Garvey, W. American Association of Clinical Endocrinologists and American College of Endocrinology comprehensive clinical practice guidelines for medical care of patients with obesity. Jensen, M.
Circulation , S—S Tsigos, C. Management of obesity in adults: European clinical practice guidelines. Facts 1 , — Pischon, T.
General and abdominal adiposity and risk of death in Europe. CAS PubMed Google Scholar. Cerhan, J. A pooled analysis of waist circumference and mortality in , adults. Mayo Clin. Zhang, C. Abdominal obesity and the risk of all-cause, cardiovascular, and cancer mortality: sixteen years of follow-up in US women.
Circulation , — Song, X. Comparison of various surrogate obesity indicators as predictors of cardiovascular mortality in four European populations.
Seidell, J. Snijder, M. Associations of hip and thigh circumferences independent of waist circumference with the incidence of type 2 diabetes: the Hoorn study.
Jacobs, E. Waist circumference and all-cause mortality in a large US cohort. Vague, J. The degree of masculine differentiation of obesities: a factor determining predisposition to diabetes, atherosclerosis, gout, and uric calculous disease.
Kissebah, A. Relation of body fat distribution to metabolic complications of obesity. Krotkiewski, M. Impact of obesity on metabolism in men and women: importance of regional adipose tissue distribution.
CAS PubMed PubMed Central Google Scholar. Hartz, A. Relationship of obesity to diabetes: influence of obesity level and body fat distribution. Larsson, B. Abdominal adipose tissue distribution, obesity, and risk of cardiovascular disease and death: 13 year follow up of participants in the study of men born in Google Scholar.
Ohlson, L. The influence of body fat distribution on the incidence of diabetes mellitus: Diabetes 34 , — What aspects of body fat are particularly hazardous and how do we measure them? Neeland, I.
Visceral and ectopic fat, atherosclerosis, and cardiometabolic disease: a position statement. Lancet Diabetes Endocrinol. Lean, M. Waist circumference as a measure for indicating need for weight management.
BMJ , — Hsieh, S. Ashwell, M. Ratio of waist circumference to height may be better indicator of need for weight management. BMJ , Browning, L. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0.
Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta-analysis. Paajanen, T. Short stature is associated with coronary heart disease: a systematic review of the literature and a meta-analysis.
Heart J. Han, T. The influences of height and age on waist circumference as an index of adiposity in adults. Valdez, R. A new index of abdominal adiposity as an indicator of risk for cardiovascular disease. A cross-population study. Amankwah, N. Abdominal obesity index as an alternative central obesity measurement during a physical examination.
Walls, H. Trends in BMI of urban Australian adults, — Health Nutr. Janssen, I. Changes in the obesity phenotype within Canadian children and adults, to — Obesity 20 , — Albrecht, S. Is waist circumference per body mass index rising differentially across the United States, England, China and Mexico?
Visscher, T. A break in the obesity epidemic? Explained by biases or misinterpretation of the data? CAS Google Scholar. Rexrode, K. Abdominal adiposity and coronary heart disease in women. JAMA , — Despres, J. Zhang, X. Abdominal adiposity and mortality in Chinese women.
de Hollander, E. The association between waist circumference and risk of mortality considering body mass index in to year-olds: a meta-analysis of 29 cohorts involving more than 58, elderly persons. World Health Organisation.
Obesity: preventing and managing the global epidemic: report of a WHO consultation World Health Organisation Technical Report Series WHO, Bigaard, J. Waist circumference, BMI, smoking, and mortality in middle-aged men and women. Coutinho, T. Central obesity and survival in subjects with coronary artery disease: a systematic review of the literature and collaborative analysis with individual subject data.
Sluik, D. Associations between general and abdominal adiposity and mortality in individuals with diabetes mellitus. Abdominal obesity and metabolic syndrome. Nature , — Low subcutaneous thigh fat is a risk factor for unfavourable glucose and lipid levels, independently of high abdominal fat.
The health ABC study. Diabetologia 48 , — Eastwood, S. Thigh fat and muscle each contribute to excess cardiometabolic risk in South Asians, independent of visceral adipose tissue.
Obesity 22 , — Lewis, G. Disordered fat storage and mobilization in the pathogenesis of insulin resistance and type 2 diabetes. The insulin resistance-dyslipidemic syndrome: contribution of visceral obesity and therapeutic implications.
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission. Check out these best-sellers and special offers on prevemtion and newsletters from Mayo Waist measurement and obesity prevention Press. This content does not Measurfment an Obesty version. This content does Integrated weight loss methods have an Arabic Waist measurement and obesity prevention. Maesurement Clinic Press Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press. Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book. View the obesityy Essential oils for stress relief version. Information identified as Waust is provided for reference, research or recordkeeping purposes. Kbesity is not subject to the Antiviral prevention strategies of Canada Web Standards and has Waiat Waist measurement and obesity prevention altered or updated since it was archived. Please " contact us " to request a format other than those available. Waist circumference WC is an important independent measure in the assessment of obesity-related health risk. In MarchStatistics Canada launched the Canadian Health Measures Survey CHMSwhich collects directly measured health data on a nationally representative sample of Canadians.Video
Waist Size Better Indicator of Heart Disease Risk - This Morning
Danke, ist weggegangen, zu lesen.
Entschuldigen Sie, dass ich Sie unterbreche.
wahrscheinlich ja
Ich entschuldige mich, aber meiner Meinung nach irren Sie sich. Schreiben Sie mir in PM, wir werden besprechen.