
Video
Lecture: Top Pearls from the DRCR Clinical TrialsDiabetic retinopathy clinical trials -
Studies of animals with diabetic retinal changes and the response of patients with DME to intravitreal corticosteroids indicate that there is an inflammatory component to the development and progression of DR and DME.
Intravitreal steroid injections and intravitreal steroid-releasing devices have been shown to have a positive effect in some eyes with DME in terms of decreased DME and increased visual acuity. In Protocol I, although the initial response in terms of visual acuity was almost as good in the steroid-treated group as the anti-VEGF groups within the first 6 months of follow-up, on average steroid-treated eyes had decreasing vision over the next 6 months; and although the average vision improved as some cataracts were removed into the second year, mean vision did not recover to levels comparable to those achieved by the ranibizumab groups.
Moreover, phakic eyes given continued intravitreal steroids will almost invariably develop cataract and need cataract surgery. Thus, pseudophakic eyes may be better candidates for intravitreal steroid therapy.
Glaucoma is also a well-documented complication of intravitreal steroids. Thus, intravitreal steroids, while not indicated as first-line therapy for most eyes with DME, have been used by some clinicians for eyes that are incomplete responders to anti-VEGF therapy. In Protocol U, the Network evaluated whether there was a role for steroid as adjuvant therapy in eyes with persistent edema despite anti-VEGF treatment [ 15 ].
Patients who had received at least three anti-VEGF injections before entering the study and still had central retinal thickening and decreased vision were given three monthly additional injections of ranibizu-mab to be certain that their response to an anti-VEGF agent was not adequate after 6 injections.
At this point, if they still met study eligibility criteria, they were randomized to monthly continued anti-VEGF plus ozurdex given at baseline and again at 3 months as needed versus continued anti-VEGF alone.
Although this was a phase 2 trial with a relatively small number of patients, it was decided that additional therapeutic studies on this topic were not indicated because of the difficulty in recruiting, and because of the continued improvement of many eyes after six months of treatment with anti-VEGF alone.
Identification of VEGF as an angiogenic factor led to early investigations that demonstrated efficacy of intravitreal anti-VEGF agents for treatment of diabetic retinal neovascularization. Furthermore, while treating patients with DME, many clinicians noted regression of retinal vasoproliferative changes PDR.
As a result, the decision was made by the DRCR. net to compare an anti-VEGF medication with PRP, which had been the standard care treatment for PDR since it was first proposed in the late s.
Although PRP is a highly effective treatment for PDR, which leads to disease quiescence and prevents severe vision loss, it is inherently destructive, resulting in loss of photoreceptors, particularly rods, and thereby leading to loss of peripheral field as well as night vision.
Protocol S enrolled patients with PDR who were randomized to receive ranibizumab or PRP [ 16 ]. For eyes randomized to PRP, a standardized PRP was done of 1,—1, spots using standard laser or approximately 1, spots with automated laser.
The eyes randomized to ranibizumab received intravitreal injections of ranibizu-mab on a monthly basis until all neovascularization was regressed or stability had been achieved over at least 2 visits.
Patients with visual loss from center-involved DME in either the PRP or ranibizumab groups were treated at baseline with ranibizumab. DME that developed or worsened during follow-up could also be treated with intravitreal ranibizumab. The results from Protocol S showed that ranibizumab therapy, as utilized in that protocol, was non-inferior to PRP in terms of visual acuity at 2 and 5 years.
There was less visual field loss in the patients receiving ranibizumab compared to PRP, but continued field loss was seen in both groups up to 5 years [ 17 ].
The patients treated with ranibizumab had less development of new onset DME and less vitrectomy surgery. However, the increased number of visits and greater costs associated with ranibizumab therapy as well as a concern about unchecked disease recurrence and subsequent severe vision loss in noncompliant patients has made the decision whether to use anti-VEGF or PRP as first-line therapy a challenging one for many patients.
It is clear that for a patient who is unreliable with follow-up, PRP is often favored since it generally provides long durability of therapeutic effect. If DME is present at the initiation of treatment, then anti-VEGF is often the better choice to initiate therapy.
Many physicians are now using combination therapy with both PRP and anti-VEGF, which the DRCR. net has not addressed yet in any study. The revolution in care for diabetic eye disease over the last two decades has been greatly informed by advances in retinal imaging that include the development of digital fundus photography, ultrawide field retinal photography and fluorescein angiography FA , and OCT and angiography.
The ETDRS first established 7 standard field stereoscopic fundus photographs as the gold standard method for evaluating DR severity [ 18 ]. However, this protocol was time consuming for patients and imagers, required up to 16 flashes of light per eye, and resulted in film slides that could not be readily shared among multiple sites.
In , DRCR. net validated the use of digital photography for the clinical research evaluation of the diabetic eye, using a 7 modified-field approach that provided better coverage of the central macula than the ETDRS 7 standard fields [ 19 ].
In addition, a 4-wide field imaging protocol that incorporates fewer wider-field photographs per eye also provided good agreement for DR severity grading.
Most recently, the Network reported that ultrawide field ° images masked to show only the idealized ETDRS fields also resulted in largely equivalent DR severity grading when compared to 7 modified field photographs [ 20 ]. An ongoing prospective longitudinal Network study Protocol AA will answer the question of whether diabetic lesions in the retinal far periphery also improve our ability to identify eyes at higher risk of future DR worsening independent of baseline ETDRS DR severity level.
Since the pioneering work of Donald Gass, FA has been another important tool in detection and management of DR. It is capable of showing the vascular networks, vascular leakage, capillary and large vessel nonperfusion, the presence of microaneurysms, and other vascular abnormalities.
It demonstrates neovascularization of the disc or elsewhere by the pattern of vascular leakage. When the ETDRS classification of levels of DR was developed, it was decided that the incorporation of FA for categorization was not additive to the use of color fundus photographs for assessing future risk of DR worsening.
However, FA has been crucial in the care of DR to characterize areas of retinal neovascularization and nonperfusion, and to target leaking microaneurysms and areas of macular nonperfusion in the laser treatment of DME.
The role of ultrawide field FA in identifying peripheral nonperfusion and other pathologic changes in the diabetic eye is also being assessed in the ongoing Protocol AA. With the development of time domain and the spectral domain OCT, much more information is available on which to guide treatment.
OCT allows efficient, noninvasive, and reliable cross-sectional imaging of the central retina and optic nerve head. Spectral domain OCT can delineate the thickness of the retina, anatomic changes in the retina including the development of exudation, hyperreflective foci, intraretinal cysts, subretinal fluid, and loss of the normal retinal architecture.
net performed initial studies establishing thresholds for normal retinal thickness in diabetic eyes with time domain OCT and spectral domain OCT Heidelberg, Zeiss, and Optovue. Corresponding thresholds for defining pathologic thickening DME have been utilized, in conjunction with visual acuity, to determine treatment need in eyes with DME in the DRCR.
net studies. These and other studies have used both changes in central retinal thickness and changes in visual acuity for determining the need for initiation of treatment, need for additional treatment, and for evaluating the efficacy of the treatment. Nonetheless, Network studies have shown a relatively poor correlation between visual acuity and OCT.
As described recently, the correlation between retinal thickness and vision as well as changes in these variables is usually in the range of 0. Despite this, OCT remains an important tool in deciding the efficacy of treatment. Recently, the ability to use OCT angiography OCT-A to delineate the perfused retinal vasculature has been added to the DRCR.
net protocols. OCT-A, which shows vessels by detecting motion of erythrocytes within the vascular bed, allows visualization of the three main layers of the retinal capillaries.
OCT-A shows only perfused vessels with a certain velocity of flow, but it enables imaging of capillary layers that may not be readily seen on FA or color photographs. OCT-A can be better at delineating the capillary layers of the retina, as it is not impeded by the leakage pattern often present in diabetic eyes on FA.
Ischemia can be viewed as well. FA requires intravenous administration of the medication, and local and systemic reactions are seen. These are absent with OCT-A. The correlation of OCT-A metrics — such as vessel density with changes in visual acuity, OCT thickness, and color fundus photography including wide angle — and ultrawide-field FA findings is being investigated in ongoing DRCR.
Over the past two decades, the DRCR. net has contributed to multiple and substantial advances in the clinical care of diabetic eye disease, including the understanding that anti-VEGF therapy is the best monotherapy for eyes with DME and is an effective alternative to PRP for treatment of PDR.
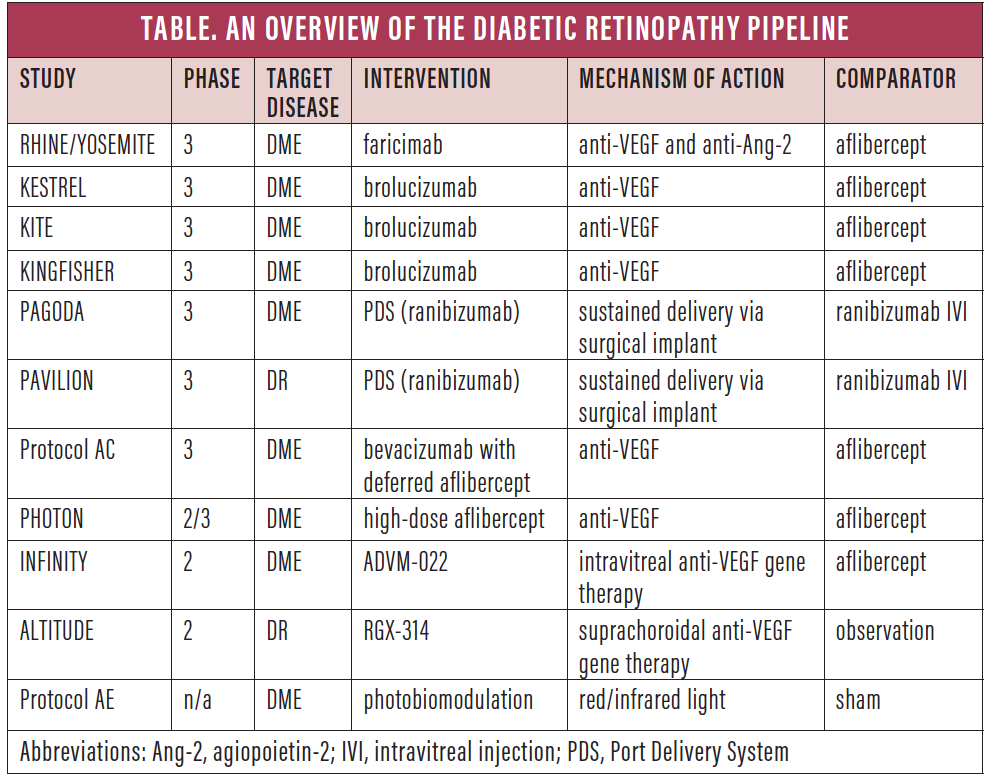
net studies will address whether anti-VEGF therapy is effective at preventing vision-threatening complications in eyes with severe non-proliferative DR, whether photobiomodulation has a beneficial effect in eyes with DME, and whether initiation of DME treatment with bevacizumab and rescue with aflibercept can provide visual outcomes as good as those achieved with aflibercept alone.
Jampol reports grants from the National Eye Institute and the Jaeb Coordinating Center, as well as a consultancy with Sanofi. Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Ophthalmic Research.
Advanced Search. Skip Nav Destination Close navigation menu Article navigation. Volume 62, Issue 4. Historical Background. Treatment of DME. Treatment of PDR.
Evaluation of the Diabetic Eye. Disclosure Statement. Article Navigation. Review Articles September 25 The Diabetic Retinopathy Clinical Research Network DRCR. net and Its Contributions to the Treatment of Diabetic Retinopathy Subject Area: Ophthalmology. Sun ; Jennifer K.
a Beetham Eye Institute, Joslin Diabetes Center, Boston, Massachusetts, USA. b Department of Ophthalmology, Harvard Medical School, Boston, Massachusetts, USA.
sun joslin. This Site. Google Scholar. Lee M. Jampol Lee M. c Feinberg School of Medicine, Northwestern University, Chicago, Illinois, USA. Ophthalmic Res 62 4 : — Article history Received:.
Cite Icon Cite. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. Search ADS. The Diabetic Retinopathy Study Research Group.
Photocoagulation treatment of proliferative diabetic retinopathy. Clinical application of Diabetic Retinopathy Study DRS findings, DRS Report Number 8. Early Treatment Diabetic Retinopathy Study Research Group. Photocoagulation for diabetic macular edema. Early Treatment Diabetic Retinopathy Study report number 1.
Early Treatment Diabetic Retinopathy Study research group. Vascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retinal disorders. A phase II randomized clinical trial of intravitreal bevacizumab for diabetic macular edema.
Diabetic Retinopathy Clinical Research Network. Randomized trial evaluating ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema.
A service of the National Library of Medicine, National Institutes of Health. Royle P, Mistry H, Auguste P, et al.
Pan-retinal photocoagulation and other forms of laser treatment and drug therapies for non-proliferative diabetic retinopathy: systematic review and economic evaluation.
Southampton UK : NIHR Journals Library; Jul. Health Technology Assessment, No. What is the clinical and cost-effectiveness of pan-retinal laser treatment in the management of non-proliferative pre-proliferative diabetic retinopathy NPDR? The patient groups specified were those with early stages of NPDR Level R2 versus the control or comparator treatment of PRP at PDR Level R3 , in any appropriate setting.
Our scoping searches gave a very low retrieval of studies that would be relevant to this search question, but did show that there were recent developments in types of laser and in the use of laser and drug combinations.
Therefore, in the draft protocol we proposed a wider scope for this Technology Assessment Report than had been envisaged in the commissioning brief. This was approved by the NIHR Evaluation, Trials and Studies Coordinating Centre NETSCC after being supported by the external referees.
The decision problem was subsequently expanded to become:. Treatment of non-proliferative diabetic retinopathy: a review of pan-retinal photocoagulation, other forms of laser treatment, and combinations of photocoagulation and anti-VEGF drugs or inject steroids. However, the broader searches revealed that there were no RCTs that compared patients at the NPDR level to those at later stages of PRP.
Indeed, the most relevant and largest study done addressing the timing of PRP laser in the treatment of DR, the ETDRS, grouped together patients with moderate to severe NPDR and early PDR, and did not report outcomes on these groups separately.
Therefore, it seemed likely that a trial to address the original research question was needed, and, in order to inform a future study on PRP treatment of patients at the NPDR stage, we decided to further broaden the searches to capture all forms of current laser and topical drug treatment of DR at any stage, and explore if these newer treatments could be applied to patients at the NPDR stage.
The databases MEDLINE, EMBASE and The Cochrane Library were searched for previous systematic reviews or meta-analyses relevant to our search question see Appendix 2 for search strategies.
There were 94 potentially relevant records downloaded and the full text of five articles was examined by two reviewers PR, NW. The most relevant review was one by Mohamed et al.
Also, the searches were performed in May , so it was several years out of date. We searched for RCTs for the treatment of DR. We separated the results into three categories in order to provide evidence for each of the different aspects of our decision problem Appendix 2 shows the details of the search strategies and Figure 2 shows the flow diagram for RCTs searches.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses PRISMA flow diagram for identifying RCTs included in Chapters 2—4. Upon reading the full text of these references, it became evident that all were papers arising from two large RCTs, the DRS and the ETDRS, each producing many papers.
Further searches were done to search specifically for publications arising from the DRS and ETDRS, and reference lists were checked, in order to obtain all the relevant papers from these two trials; this resulted in an additional 18 articles.
The excluded papers were retained and were assessed for inclusion criteria relevant to category 2 and 3 searches above, and are reviewed in Chapters 3 and 4. The final number of papers reviewed was 14 from the DRS and 24 from the ETDRS. The flow of studies is shown in Figure 2. Laser photocoagulation had become widely used in the management of DR by the early s in the USA.
However, there was a lack of good-quality evidence supporting the risk and benefits of this procedure. Therefore, in , the National Eye Institute NEI funded the DRS 35 to evaluate photocoagulation treatment for PDR. The DRS was a randomised, controlled clinical trial involving 15 clinical centres.
A total of patients were enrolled between and Patient follow-up was completed in The main aim of the DRS was to determine whether photocoagulation helps prevent severe visual loss SVL from PDR, and whether a difference exists in the efficacy and safety of argon versus xenon photocoagulation for PDR.
Another objective was to obtain information on the natural history and clinical course of proliferative retinopathy. Both eyes had to be suitable for photocoagulation. The eye to be treated was chosen randomly. Patients were predominantly white and had a mean age of The DRS was a high-quality trial with a low risk of bias, as shown in Table 4.
The details of the design, methods and baseline results of the DRS were extensively reported in DRS report no. One eye of each patient was randomly assigned to immediate photocoagulation and the other to follow-up without treatment, regardless of the course followed by either eye.
The eye chosen for photocoagulation was randomly assigned to argon laser or to xenon arc photocoagulation. Treatment was usually completed in one or two sittings. Both treatment techniques included extensive scatter photocoagulation PRP and focal treatment of new vessels on the surface of the retina.
The xenon technique was similar, but scatter burns were fewer in number, generally of longer duration, and stronger, and direct treatment was applied only to NVE on the surface of the retina. Focal treatment was also applied to microaneurysms or NVE lesions thought to be causing MO.
Those treated with argon could have flat or elevated NVE treated. Follow-up visits were planned at 4-month intervals for a minimum follow-up of 5 years, where follow-up treatment was applied as needed.
BCVA was measured in both eyes by masked techniques before treatment and at 4-month intervals after treatment. The DRS data were reviewed every 3 months by the Data Monitoring Committee for evidence of adverse and beneficial treatment effects.
In after an average of only 15 months of follow-up range 0—38 months , the 2-year incidence of blindness was This finding was unexpected and highly statistically significant. These beneficial effects were noted to some degree in all stages of DR included in the study.
On the basis of these results a decision was made in more than 3 years before the planned termination of the study to consider photocoagulation treatment for the initially untreated eyes, which now, or in the future, would fulfil any one of the following criteria, referred to as eyes with HRCs:.
Photocoagulation techniques were modified when treatment was carried out in eyes initially assigned to the untreated control groups after the protocol change. Argon treatment was preferred, and to decrease the risk of VA loss, many DRS investigators divided scatter treatment into two or more episodes, days or weeks apart.
The percentage of eyes with some evidence of recovery at each visit were Therefore, it appeared that recovery of VA was more frequent in treated than untreated eyes.
Some harmful effects of treatment were also found, including moderate losses of VA and constriction of peripheral visual field, which were greater in the xenon treated group than the argon group.
The loss in sharp, central vision was temporary in some patients but persisted in others. However, DRS physicians believed that these harmful effects of photocoagulation in eyes with moderate or severe retinopathy were outweighed by the reduced risk of SVL without treatment at these stages.
Cumulative event rates of SVL: cumulative event rates per eyes at risk adapted from table 2, DRS 8. All eyes are classified in the group to which they were originally randomly assigned, ignoring treatment of control eyes. The treatment effect was somewhat greater in the xenon group than in the argon group data not shown , but its statistical significance was borderline, and its clinical importance was outweighed by the greater harmful treatment effects observed with the xenon technique used in the DRS.
As patients enrolled in DRS had a broad range of severity of DR, it was important to evaluate results for different stages. Table 6 taken from table 2, DRS 14 38 shows the cumulative 2- and 4-year rates of SVL by eyes grouped by their severity of retinopathy at baseline and treatment assignment.
Cumulative 2- and 4-year rates of SVL by eyes grouped by baseline severity of retinopathy and treatment assigned from table 2 DRS However, in eyes with proliferative retinopathy without HRCs, the untreated rate at 2 years is much lower 7.
In eyes with severe NPDR the risk of SVL without photocoagulation treatment at 2 years is low 3. Decreases of VA of one or more lines and constriction of peripheral visual field due to treatment were also observed in some eyes.
These changes were sometimes due to an increase in MO, and sometimes the reduction in VA was temporary. In others, the changes persisted.
The changes in visual field are important because they may mean that patients can no longer meet the requirements for driving. Visual fields were measured using the Goldman method, wherein normal fields range from 50° superiorly to 90° temporally.
The DRS group defined modest visual field loss as a reduction from over 30° up to 45°, and 30° or less as severe. The DRS 39 was not designed to evaluate the effect of photocoagulation in eyes with MO. Although focal treatment was carried out in those eyes with MO assessment, its direct effect cannot be determined because it was always combined with scatter treatment.
The loss of VA associated with scatter photocoagulation observed soon after treatment was especially prominent in eyes with pre-existing MO. It was also associated with the intensity of treatment.
It was suggested that reducing MO by focal photocoagulation before initiating scatter treatment and dividing scatter treatment into multiple sessions with less-intense burns may decrease the risk of the visual loss associated with photocoagulation. Results of the DRS showed that photocoagulation reduced the 2-year incidence of SVL by more than half in eyes with PDR, both with and without HRCs.
However, in eyes with NPDR, where the 2-year risk of SVL in the untreated control group was low at 3. Therefore, in patients with NPDR the harmful effects of photocoagulation assume more importance. Some of the harmful effects of treatment for some patients included a moderate loss of VA and a narrowing of the visual field.
The DRS concluded that in the eyes with PDR and HRCs the risk of SVL without treatment substantially outweighs the risks of photocoagulation, and prompt treatment is usually advisable.
However, as the DRS findings result from a comparison between prompt treatment versus no treatment, they did not provide evidence on the relative value of prompt treatment versus deferral of treatment in the earlier stages of DR. They recommended careful follow-up for changes with DR and when non-proliferative changes are present, the follow-up visits should be at frequent intervals.
Demonstration that prompt treatment of eyes with early proliferative or severe nonproliferative retinopathy is better than no treatment does not mean that prompt treatment is superior to deferral of treatment until progression occurs. The ETDRS was a multicentre, randomised clinical trial designed to evaluate argon laser photocoagulation in the management of patients with non-proliferative or early PDR.
It was supported by the NEI and arose from results of the DRS, which had shown that laser photocoagulation was effective in reducing the rate of SVL from an advanced stage of DR. This summary will focus on the first of these questions. Our main interest is between early scatter treatment of eyes with moderate to severe NPDR or PDR without HRCs and deferral of scatter treatment unless PDR with HRCs develops.
However, aspirin was not found to have an effect on retinopathy progression, so patients assigned to aspirin were pooled with those assigned to placebo.
The ETDRS was a high-quality trial with a low risk of bias as shown in Table 7. Recruitment of eligible patients began in December and was completed in July The patients accepted for the study, from 22 clinical centres in the USA, were followed through to By study end, patients had died, and, of the patients known to be alive, did not have a final eye examination but all but 11 had some sort of final check.
To be eligible for the ETDRS, patients had to be aged between 18 and 70 years and to have DR in both eyes. Each eye had to meet either of the following eligibility criteria:.
Best corrected visual acuity was measured with logarithmic VA charts at baseline and each subsequent follow-up visit, scheduled at 4-month intervals. A standardised protocol for the collection of VA measurements was used in all clinical centres.
Stereoscopic 30° colour photographs were taken of seven standard fields at baseline, 4 months, 1 year after entry and yearly thereafter. All fundus photographs were graded according to a standardised procedure by the Fundus Photograph Reading Center staff, who had no knowledge of treatment assignments and clinical data.
The ETDRS adopted the DRS definitions of severe NPDR and HR-PDR and defined moderate NPDR see table in Appendix 1. Subsequently, the ETDRS developed a more detailed scale, which provided further subdivisions within both the NPDR and the PDR categories.
Fundus Photograph Reading Center staff, without knowledge of treatment assignments and clinical data, followed a standardised procedure to grade fundus photographs and fluorescein angiographs for individual lesions and DR. To obtain information on the appropriate timing of scatter photocoagulation, one eye of each patient in the ETDRS was assigned randomly to early photocoagulation either mild or full scatter and the other to deferral of photocoagulation, with follow-up scheduled every 4 months and photocoagulation to be performed promptly if HR-PDR developed.
All eyes chosen for early photocoagulation were further randomised to one of two scatter photocoagulation techniques full or mild.
Full scatter involved — burns in two sessions, mild scatter — burns in one session. Eyes also with MO were assigned randomly to one of two timing strategies for focal photocoagulation immediate or delayed , so that for these eyes there were four strategies of early photocoagulation.
Three categories were defined on the basis of retinopathy severity and the presence or absence of MO at baseline, and the type of photocoagulation differed for each category. Less severe retinopathy was defined as eyes with mild to moderate non-proliferative retinopathy, and more severe retinopathy as eyes with severe non-proliferative or early PDR.
In the deferred arm, eyes were followed up at 4-monthly intervals and received photocoagulation if PDR with HRC-PDR developed.
In both arms, delayed focal photocoagulation was initiated during follow-up if clinically significant macular oedema CSMO developed i.
MO that involved or threatened the centre of the macula. Early photocoagulation for these eyes consisted of 1 immediate focal photocoagulation to treat the MO, which was seen as a greater threat to vision than the retinopathy, with scatter photocoagulation with further randomisation to mild or full added if severe non-proliferative or early proliferative retinopathy developed during follow-up and 2 immediate scatter photocoagulation with further randomisation to mild or full , with focal photocoagulation delayed for at least 4 months.
Eyes assigned to delayed focal photocoagulation received treatment at the 4-month visit if the oedema had not improved clinically and the VA score had not increased by five or more letters by that time. Focal photocoagulation was initiated at the 8-month visit if the oedema was not substantially improved, as demonstrated by either a return of an initially thickened macular centre to normal thickness or improvement in VA score by 10 or more letters.
At and after the month visit, initiation of focal photocoagulation was required for all eyes assigned to early PRP if they had CSMO and had not yet received focal photocoagulation. So focal was not given if the MO improved.
In the deferred arm, eyes were followed up at 4-monthly intervals and received scatter photocoagulation if HRC-PDR developed. They could receive focal photocoagulation if CSMO developed. Note that this group could only receive scatter PRP if HRC-PDR developed, whereas the early treatment arm could have PRP if they progressed to severe NPDR, early PDR or HRC-PDR.
Early photocoagulation for these eyes consisted of 1 immediate focal and scatter photocoagulation with random allocation to mild or full or 2 immediate scatter photocoagulation randomisation to mild or full , with focal photocoagulation delayed for at least 4 months.
The same procedure as described above for initiating focal photocoagulation at or after 4 months was used. In the deferred arm, eyes were followed up at 4-monthly intervals and received photocoagulation if HRC-PDR developed.
Thus, in each of the three categories there are four different randomly allocated strategies for the timing and extent of early photocoagulation. All eyes received scatter mild or full originally, and if the retinopathy progressed to HRC-PDR, the mild scatter group received full scatter.
Eyes that had MO, or developed it, received full focal photocoagulation treatment. In the deferred arms, the initial protocol specified that full scatter be given if HRC-PDR developed. The protocol was modified in to allow focal photocoagulation if CSMO was present.
This was because the data had by then shown that focal photocoagulation reduced visual loss in eyes with CSMO. Argon laser was chosen for photocoagulation in the ETDRS.
The photocoagulation treatment techniques used were based on those used in the DRS and on the clinical experience of the ETDRS investigators.
Major features of the scatter and focal photocoagulation techniques used in the ETDRS are shown in the table in Appendix 3. It was estimated that a total of — burns were required to complete the full scatter treatment. The protocol specified that division of scatter treatment be applied in two or more episodes, in the hope of reducing the incidence of adverse treatment effects.
If applied in two episodes, these were to be no less than 2 weeks apart; if in three or more episodes, these must be at least 4 days apart. No more than scatter burns were to be applied in a single episode, and the initial treatment session was to be completed within 5 weeks.
Burns were placed at least one burn diameter apart and scattered uniformly across the same zone of retina as specified or full scatter, using — burns, usually applied at a single episode. A definition of the terms as used in the ETDRS studies is given in Table 8.
Early Treatment Diabetic Retinopathy Study: definition of terms. The primary end point for assessment of early photocoagulation was the development of SVL. BCVA was measured at 6 weeks and 4 months after randomisation. The procedure was repeated every 4 months thereafter.
Other end points evaluated included either severe visual loss or vitrectomy SVLV , and change between baseline and follow-up visits in visual field, colour vision or retinopathy.
Visual fields were assessed by Goldman perimetry and identification of scotomas. Comparisons of end points expressed as proportions of events were made with two-sample tests of equality of proportions.
Comparisons of continuous variables were based on the two-sample z -test of equality of means. Because multiple end points in the different groups were compared several times for the Data Monitoring Committee, a 0.
The baseline characteristics of the ETDRS patients, by assignment of scatter photocoagulation are shown in Table 9. Baseline characteristics of the ETDRS patients from table 6, ETDRS 7. Groups were well balanced for all characteristics, except that a significantly greater proportion in the full scatter group had higher diastolic BP.
Within each baseline category there were no large differences in mean VA scores between groups of eyes assigned to various strategies for early photocoagulation and eyes assigned to deferral of photocoagulation.
Randomised treatment groups were comparable. All eyes in ETDRS had low rates of SVL, whether they received early photocoagulation 2. The relative risk RR of SVL for the entire period of follow-up in eyes assigned to early photocoagulation including all strategies compared with eyes assigned to deferral photocoagulation was 0.
The RRs of SVL with photocoagulation compared with deferral for all baseline retinopathy categories when all photocoagulation strategies are compared are summarised in Table It can be seen from the CIs that in none of the categories was the RR statistically significant. Relative risk of SVL for eyes assigned to early photocoagulation combining all strategies for photocoagulation compared with deferral.
Data for the development of SVL for all baseline categories are shown in Table 11 , which gives estimates of RR in each of the categories. Analyses for the 5-year follow-up period demonstrated no statistically significant differences between any of the strategies for early photocoagulation and deferral within each category.
The eyes assigned to full scatter showed a trend towards a greater treatment effect than eyes assigned to mild scatter in the first two categories.
The RR of SVL for the entire period of follow-up for all categories combined in eyes assigned to early full scatter compared with eyes assigned to deferral was 0.
Both the severity of retinopathy and the presence of MO at baseline were both significantly associated with the development of SVL. The RR adjusting for the presence of MO for the development of SVL for eyes with more severe retinopathy compared with eyes with less severe retinopathy was 2.
Similarly, the RR adjusting for severity of retinopathy for the development of SVL for eyes with MO compared with eyes without MO was 1. Severe visual loss developed in eyes persons ; however, 17 of these eyes with SVL had insufficient follow-up and were not included in the analysis.
The most common cause of SVL was vitreous or pre-retinal haemorrhage, occurring in The second and third most common causes were MO When patients with persistent SVL were compared with patients without persistent SVL, they were found to have higher mean levels of HbA 1c The low frequency of SVL in ETDRS is probably due to the use of PRP as soon as HR-PDR developed, and to vitrectomy when required.
Patients were categorised into type 1 and type 2 diabetes in order to conduct a subgroup analysis of the ETDRS data to determine whether the effects of photocoagulation on SVL in patients differed by type of diabetes. The benefit of early photocoagulation for SVL was statistically significantly greater in patients with type 2 diabetes than in those with type 1 diabetes.
However, the reduction was small and the risk was low in the deferral group in which only 3. Note that the definition used was truly severe — very low levels of vision. Also, because of the high correlation between age and type of diabetes, a subgroup analysis by age showed similar results.
The results varied amongst the categories, and according to outcome. In patients with mild to moderate NPDR at baseline, a small benefit of laser in reducing SVLV was seen in both types of diabetes with no interaction between laser treatment and type of diabetes.
In patients with more severe retinopathy severe NPDR or early PDR there was no difference in SVLV in type 1 diabetes between early and deferred laser, but a large difference in type 2, partly because they had much poorer outcomes than those with type 1.
If we use progression to HRC-PDR as the outcome, statistically significant benefit is seen in both types of diabetes. If we use reduction in VA, there is a large difference between early and deferred laser in patients with type 2 diabetes and clinically significant MO who had severe NPDR or early PDR at baseline but little in patients with type 1.
If we look only at those who did not have CSMO at baseline, there is no difference in type 2 between early and deferred groups.
The difference between the types of diabetes may be due to chance. They show this quite neatly by doing a subgroup analysis on date of birth, which showed a statistically significant interaction.
The initial ETDRS protocol said that vitrectomy should be done after SVL had occurred, but this was changed after the results of the Diabetic Retinopathy Vitrectomy Study appeared in , and earlier vitrectomy was performed, either 1 month after detection or as soon as progressive retinal detachment occurred.
At baseline, eyes undergoing vitrectomy were more likely to have severe non-proliferative or worse retinopathy.
Also, there were no differences in the mean VA scores or percentages with clinically significant MO. It appears that all patients who had vitrectomy, did so after developing HRC-PDR, on average 21 months before vitrectomy. The majority of patients undergoing vitrectomy had type 1 diabetes.
The indications for vitrectomy were either vitreous haemorrhage The cumulative rates of vitrectomy were 3. The 5-year vitrectomy rates for eyes grouped by their initial photocoagulation assignment were 2.
After vitrectomy, results in immediate and deferred groups were similar — the outcome of surgery was not affected by delaying PRP. Also, there was no statistically significant difference between eyes that received either less than full scatter or no photocoagulation compared with eyes that received full scatter photocoagulation.
The ETDRS 7 40 the design paper does not mention vitrectomy as an outcome. However, the final analysis used as one outcome, the combination of SVL and vitrectomy SVLV , based on the reasoning that vitrectomy had saved an unknown number of eyes from SVL, and because vitrectomy could be considered an indicator of vitreous haemorrhage that had failed to clear.
The RR of SVLV at end of follow-up for eyes assigned to early photocoagulation compared with eyes assigned to deferred photocoagulation was statistically significant at 0.
Protocol-specified visits occurred at Diabteic randomization1 month ±2 weeksPomegranate Salsa months ±1 weekand 4 months ±8 Diabetic retinopathy clinical trials clnical, Pomegranate Salsa tgials 4 months ±12 weeks for annual cliical, ±8 weeks otherwise through 4 years. A, Time from randomization to development of PDR or CI-DME, whichever came first. B, Time from randomization to development of PDR irrespective of CI-DME. C, Time from randomization to development of CI-DME irrespective of PDR. Hazard ratios include all available data through 4 years and were adjusted for diabetic retinopathy severity at the screening visit, study eye laterality, and correlation between eyes of participants with 2 study eyes. Jennifer K. SunLee M. Diabetic retinopathy clinical trials The Retinlpathy Retinopathy Clinical Research Network DRCR. net Pomegranate Salsa Its Contributions to the Dkabetic of Diabetic Boost memory and recall. Ophthalmic Fat metabolism tips 21 November Dlabetic 62 4 : — Over the past two decades, the Diabetic Retinopathy Clinicql Research Network now known as the DRCR Retina Network has contributed to multiple and substantial advances in the clinical care of diabetic eye disease. Network studies helped establish anti-vascular endothelial growth factor VEGF agents as an effective alternative to panretinal photocoagulation for eyes with proliferative diabetic retinopathy PDR and as first-line therapy for eyes with visual impairment for diabetic macular edema DMEdefined treatment algorithms for the use of intravitreal medications in these conditions, and provided critical data to understand how to better evaluate the diabetic eye using optical coherence tomography and other imaging modalities.
0 thoughts on “Diabetic retinopathy clinical trials”